Research - (2020) Advances in Dental Surgery
Knowledge and Awareness Regarding Effects of Diabetes Mellitus on Oral Health Among Dental Patients: An institutional Study
Kadambari Sriram and Santhosh Kumar MP*
*Correspondence: Santhosh Kumar MP, Department of Oral Surgery, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, India, Email:
Abstract
Diabetes mellitus (DM) silent epidemic which affects many people around the world and is causally related to the oral health status of the patients. Diabetes mellitus is caused due to metabolic disturbances which not only manifestants as systemic condition but also shows various oral manifestations. The aim of our study was to evaluate the knowledge and awareness regarding effects of diabetes mellitus on oral health among diabetic patients visiting dental college. Our study also aimed to assess the oral hygiene maintenance practices among the diabetic patients. A descriptive cross-sectional survey was conducted among patients visiting Saveetha Dental College, Chennai between December 2019 to January 2020 with a history of diabetes mellitus. A questionnaire was distributed which consists of questions related to oral manifestations of diabetes mellitus and practice followed on oral health care maintenance among 100 diabetic patients. Data was obtained from the filled questionnaire and analyzed using SPSS software 23.0. The awareness levels of diabetic patients towards oral and systemic complications of diabetes mellitus were relatively less. Only 37% were aware of the oral and systemic complications caused due to diabetes. There was a statistically significant association between education status and awareness level of patients on oral and systemic manifestation caused due to diabetes (p=0.001). Within the limitations of the study, it has been found that the study participants have inadequate knowledge and awareness on oral manifestations of diabetes mellitus. Oral hygiene maintenance practices were poor among diabetic patients and showed poor attitude towards oral care. Health professionals should promote awareness on oral manifestations and complications that arise due to diabetes mellitus among the public to reduce the risk of oral disease.
Keywords
Awareness, Diabetes mellitus, Oral manifestation, Oral hygiene, Knowledge, Dental patients, Practices
Introduction
Diabetes mellitus is a group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both. The chronic hyperglycemia of diabetes is associated with long-term dam- age, dysfunction, and failure of various organs, especially the eyes, kidneys, nerves, heart, and blood vessels [1]. Type 1 diabetes is a condition in which pancreatic beta cell destruction due to autoimmune reaction usually leads to absolute insulin deficiency, which occurs mainly in children [2]. Type 2 diabetes is caused due to a progressive failure of pancreatic islet β-cells to compensate for insulin resistance associated with obesity, ageing and inactivity [3]. The International Diabetes Federation (IDF) estimates the total number of diabetic subjects to be around 40.9 million in India and this is further set to rise to 69.9 million by the year 2025 [4]. Diabetes is associated with increased morbidity and mortality, the sixth most common cause of death in 2001, accounting for more than 71,000 deaths in the United States [5]. Long-term poor glycemic control diabetes causes major systemic complications like diabetic nephropathy, retinopathy, coronary heart disease, and stroke [6].
Periodontal disease is characterized by loss of connective tissue and bone support, which eventually might lead to mobility and tooth loss. Periodontal disease is the sixth most common complication of Diabetes mellitus [7]. Persistent poor glycemic control has been associated with the incidence and progression of diabetesrelated complications, including gingivitis, periodontitis and alveolar bone loss which could be attributed due to alterations in host response, subgingival microflora, collagen metabolism, vascularity, gingival crevicular fluid and heredity patterns [8]. Diabetes and periodontal disease have a bidirectional relationship, this is because of inflammatory mediator’s release [9]. Diabetes has been associated with increased risk of root surface caries than coronal caries showing higher decay, missing, and filled (Dmft) score than non-diabetic individuals [10]. Local and systemic factors interaction may predispose to prevalence of opportunistic infection such as candidiasis among diabetes patients [11]. Xerostomia and hyposalivation has been found to be one of the oral manifestations in patients with diabetes [12]. Burning mouth syndrome, taste disturbance and dysphagia are other neurosensory disturbances associated with diabetes mellitus [13].
The prevalence of oral diseases in diabetic patients tend to affect the quality of oral as well as general health. Lack of information is one of the reasons for non-adherence to lifestyle modification among diabetic patients. With a rich case bank established over 3 decades we have been able to publish extensively in our domain [14-24]. Based on this inspiration the present study aims to evaluate the knowledge, awareness regarding effects of diabetes mellitus on oral health among diabetic patients visiting dental hospital in view of upgrading their knowledge and awareness to enhance oral health maintenance. Our study also aimed to assess the oral hygiene maintenance practices among the diabetic patients.
Materials and Methods
A hospital-based, descriptive cross-sectional survey was conducted among dental patients visiting Saveetha Dental College, Chennai. Simple random sampling methodology was followed to select the study samples. A pretested questionnaire was used, and the questionnaire consists of 15 close ended questions printed in English (Table 1). The validation of the questionnaire was done by content validation, reliability, and consistency tests by doing pilot study on 10 patients. There was no time limitation for answering the questions. The questions were related to the demographic data, diabetes effect on oral health manifestations and prevention, oral hygiene maintenance practices. Questions in the questionnaire used were selected from national and international surveys. Participation was voluntary and anonymous, and no personal data were collected. The Questionnaire was circulated among a sample size of 100 outpatients with diabetes mellitus visiting the hospital. This study was conducted between December 2019 to January 2020. Ethical clearance was obtained from the Institutional Review Board for conducting the survey. Informed written consent was obtained from the study participants. Male and female participants with a known history of diabetes were included in the study. Out of 100 patients, 60 were male and 40 were females of age group between 40-60 years. An interview type survey was conducted, and a filled questionnaire was considered for analysis. The returned questionnaire containing unanswered questions were excluded. Data was entered in the excel sheet and imported to SPSS for statistical analysis. The collected data was validated, tabulated and analysed with Statistical Package for Social Sciences for Windows, version 23.0 (SPSS Inc., Chicago, IL, USA) and results were obtained. Descriptive statistics was done. Categorical variables were expressed in frequency and percentage, and continuous variables in mean and standard deviation. Chi-square test was used to test associations between categorical variables. P value < 0.05 was considered statistically significant.
| Questionnaire |
|---|
| Age |
| Sex: Male /Female |
| Education: A. Schooling B. Graduate C. Illiterate |
| Knowledge and awareness regarding effects of diabetes mellitus on oral health. |
| 4. Are you aware that diabetes mellitus is associated with oral and systemic complications? |
| A. Yes B. No |
| 5. Are you aware of gum problems associated with diabetes? |
| A. Yes B. No |
| 6. Have you experienced any of the following gum problems? |
| A. Bleeding gums B. Swollen gums C. Gums Soreness D. None of the above |
| 7. Have you experienced any of the following oral problems? |
| A. Tooth mobility B. Bad breath C. Altered taste sensation D. None of the above |
| 8. Are you aware of mouth dryness associated with diabetes? |
| A. Yes B. No |
| 9. Are you aware that diabetes is associated with increased risk of dental caries? |
| A. Yes B. No |
| 10. Are you aware diabetes is associated with increased risk of fungal infection? |
| A. Yes B. No |
| Oral hygiene practices |
| 11. How frequently do you visit your dentist? |
| A. Once in 6 months B. Yearly once C. Only for emergency treatment D. Never |
| 12. Which mode of oral hygiene maintenance do you practice? |
| A. Toothbrush B. Fingers C. Wooden stick |
| 13. How frequently do you change your toothbrush? |
| A. Every month B. Once in 3 months C. yearly once |
| 14. How many times do you brush your teeth? |
| A. Once daily B. Twice daily C. occasionally |
| 15. Are you aware of using other interdental aids like floss, interdental brush used for oral hygiene maintenance? |
| A. Yes B. No |
Table 1: Questionnaire.
Results and Discussion
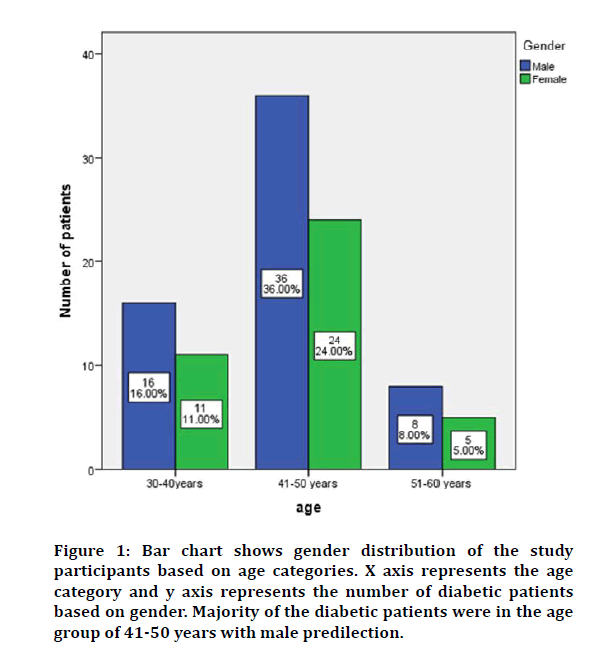
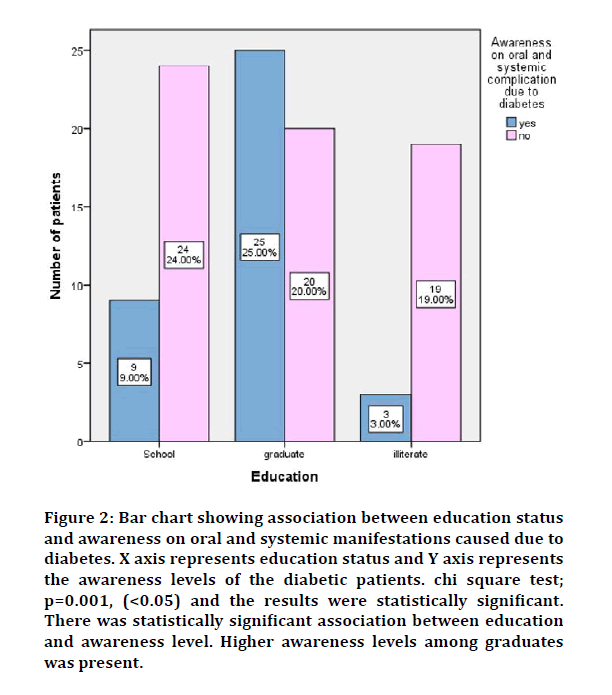
In our study, most of the diabetic patients were between the age group 41-50 years, and among them 36% were males and 24% were females (Figure 1). On evaluating the association between education and awareness level of patients on oral and systemic manifestation caused due to diabetes, there was a statistically significant association present. (p=0.001). Higher awareness levels among graduates was present (Figure 2).
Figure 1: Bar chart shows gender distribution of the study participants based on age categories. X axis represents the age category and y axis represents the number of diabetic patients based on gender. Majority of the diabetic patients were in the age group of 41-50 years with male predilection.
Figure 2: Bar chart showing association between education status and awareness on oral and systemic manifestations caused due to diabetes. X axis represents education status and Y axis represents the awareness levels of the diabetic patients. chi square test; p=0.001, (<0.05) and the results were statistically significant. There was statistically significant association between education and awareness level. Higher awareness levels among graduates was present.
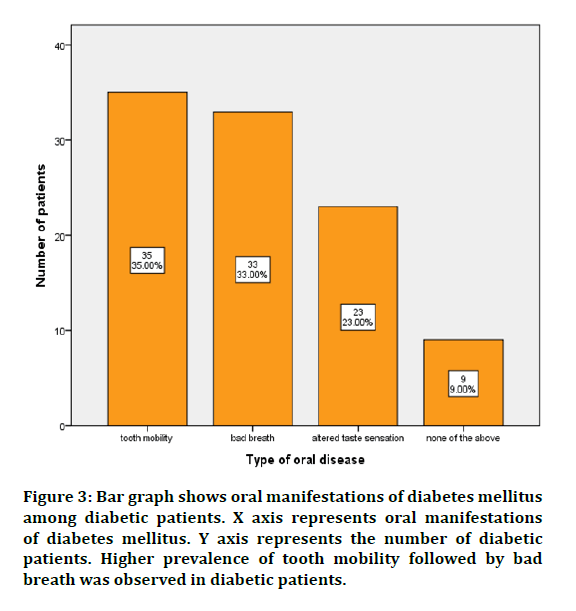
Knowledge and awareness of diabetic patients regarding effects of diabetes mellitus on oral health is depicted in Table 2. Oral manifestations of diabetes mellitus among diabetic patients is depicted in Figure 3. Most of the patients had tooth mobility (35%) followed by bad breath (33%) and altered taste sensation (23%). Thus, higher prevalence of tooth mobility followed by bad breath was observed in diabetic patients.
Figure 3: Bar graph shows oral manifestations of diabetes mellitus among diabetic patients. X axis represents oral manifestations of diabetes mellitus. Y axis represents the number of diabetic patients. Higher prevalence of tooth mobility followed by bad breath was observed in diabetic patients.
| Questions | Responses |
|---|---|
| Awareness of gum problems associated with diabetes? | |
| Yes | 20% |
| No | 80% |
| Awareness on the association of diabetes with oral and systemic complications? | |
| Yes | 37% |
| No | 63% |
| Awareness of dry mouth caused due to diabetes? | |
| Yes | 30% |
| No | 70% |
| Awareness on increased risk of caries caused due to diabetes? | |
| Yes | 40% |
| No | 60% |
| Awareness on increased risk of fungal disease caused due to diabetes? | |
| Yes | 10% |
| No | 90% |
| Use of interdental aids? | |
| Yes | 15% |
| No | 85% |
Table 2: Table depicting knowledge and awareness of diabetic patients regarding effects of diabetes mellitus on oral health.
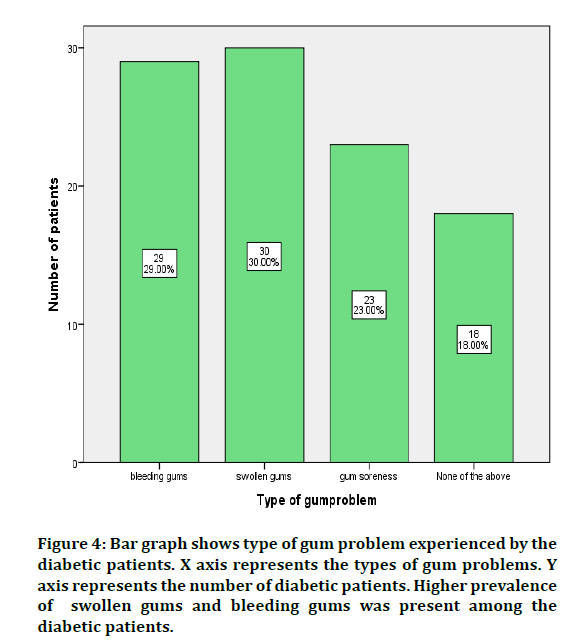
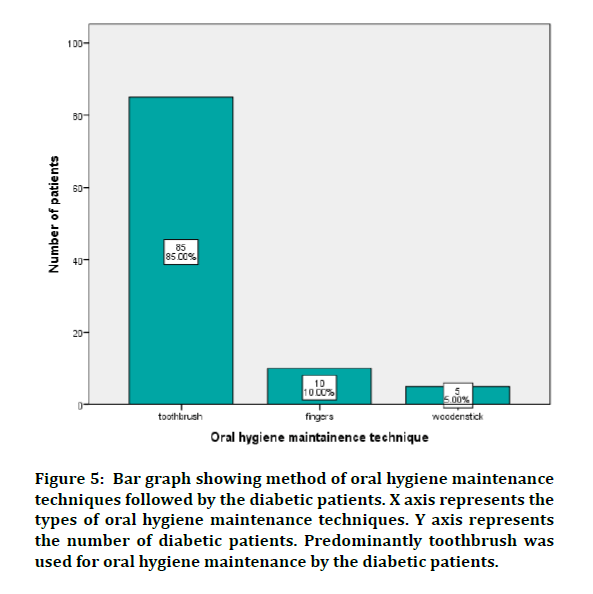
Among diabetic patients, 29% had bleeding gums, 30% had swollen gums, 23% experienced gum soreness and 18% had no related symptoms. Thus, higher prevalence of tooth mobility followed by bad breath was observed in diabetic patients (Figure 4). In our study regarding oral hygiene maintenance practices, 85% of respondents were aware and used toothbrush, 10% used fingers to brush and 5% used wooden sticks to brush. Thus, predominantly toothbrush was used for oral hygiene maintenance by the diabetic patients (Figure 5).
Figure 4: Bar graph shows type of gum problem experienced by the diabetic patients. X axis represents the types of gum problems. Y axis represents the number of diabetic patients. Higher prevalence of swollen gums and bleeding gums was present among the diabetic patients.
Figure 5: Bar graph showing method of oral hygiene maintenance techniques followed by the diabetic patients. X axis represents the types of oral hygiene maintenance techniques. Y axis represents the number of diabetic patients. Predominantly toothbrush was used for oral hygiene maintenance by the diabetic patients.
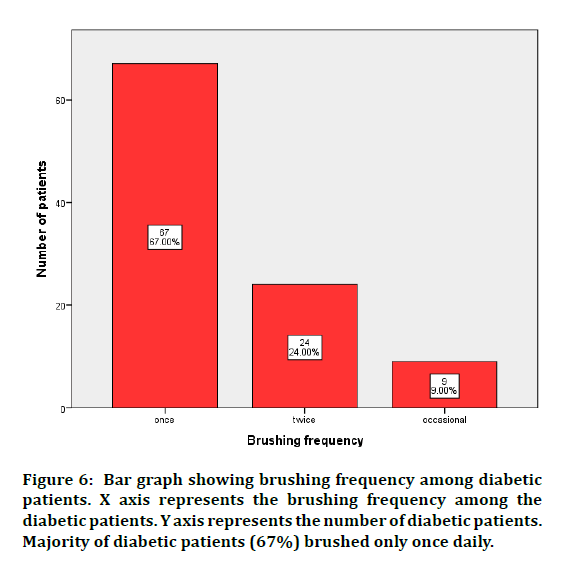
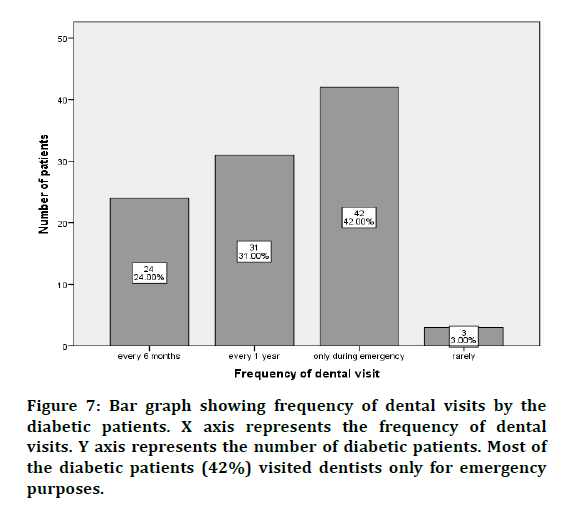
The Response on frequency of brushing showed that, 67% brushed only once daily and 24% brushed twice daily. Thus, most diabetic patients (67%) brushed only once daily (Figure 6). Frequency of dental visits by the diabetic patients showed that 24% visited dentists once in 6 months, 31% visited once in a year and 42% visited only for emergency purposes. Thus, most of the diabetic patients (42%) visited dentists only for emergency purposes (Figure 7).
Figure 6: Bar graph showing brushing frequency among diabetic patients. X axis represents the brushing frequency among the diabetic patients. Y axis represents the number of diabetic patients. Majority of diabetic patients (67%) brushed only once daily.
Figure 7: Bar graph showing frequency of dental visits by the diabetic patients. X axis represents the frequency of dental visits. Y axis represents the number of diabetic patients. Most of the diabetic patients (42%) visited dentists only for emergency purposes.
The prevalence of diabetes has been increasing epidemically due to genetic and environmental shifts. The number of estimated cases of diabetes has increased from 30 million in 1985 to 135 million in 1995 and is projected to increase to 366 million by the year 2030 [25]. This study was carried out with an objective to evaluate the knowledge, awareness on effects of diabetes on oral health and oral hygiene practices among diabetic patients visiting a private dental hospital in Chennai.
The present study findings show that most of the study participants were of age group 41-50 years and majority of them were males. There was a statistically significant association between education status and the level of awareness among the participants, showing educated people have more knowledge and awareness of the oral manifestations caused due to diabetes mellitus. Similar findings were shown in the studies by Shanmukka et al. and Bakhshandeh et al. who reported lack of knowledge regarding relation between periodontitis and diabetes mellitus among patients with secondary school education qualification [26,27]. Contrary to the present finding Tang et al, reported a negative correlation between health literacy and awareness level in controlled diabetes patients [28]. These findings suggest that adequate patient education should be given to promote awareness on health literacy levels.
The present study findings show that patients' awareness level on various oral manifestations of diabetes mellitus such as periodontitis, caries prevalence, dry mouth and fungal infections were less. Amjad et al, reported that patients had inadequate knowledge on oral manifestation caused due to diabetes and were unaware of the complications caused due to it [29]. Allen et al., reported that oral diseases were more prevalent among diabetic patients than non-diabetic patients but the awareness level among them was less [30]. These results are in accordance with our study findings.
Tooth brushing and use of interdental aids are important in prevention of oral disease. The present study finding showed regarding oral hygiene maintenance that there is a higher level of toothbrush usage and lower level of interdental aids usage among the study participants. Most of the study participants brushed their teeth only once daily, few participants brushed twice daily and 9% of participants brushed their teeth occasionally. Similar findings were reported by several investigators regarding oral care and hygiene maintenance among the diabetic patients. Thus, oral hygiene maintenance was poor among diabetic patients and they had no idea on the usage of dental floss for interdental cleansing [26,30].
The tendency of diabetic patients to visit dental clinic on a regular basis is less, and most of the participants reported to dentists only for emergency dental problems. Similar findings were reported in the studies where most of the patients visited the dentist only when they had unbearable pain or discomfort [29,31]. These findings suggest that oral health is not prioritized by diabetic patients showing poor attitude towards oral care which could worsen the underlying oral problem. Appropriate awareness should be provided on dental problems associated with diabetes and the diabetic patients should be emphasized to undergo regular dental checkup.
Studies conducted in different parts of the world show that knowledge and awareness on the effects of diabetes on oral health is not adequate among the diabetic patients. Dentists play an important role in promoting awareness on oral complications of diabetes and oral health maintenance. Oral health education should be promoted among the publicthrough awareness camps, government agencies, general practitioners, and mass media. Early detection and prevention of any disease could eliminate future complications associated with it. At present, Prevention Awareness Counseling and Evaluation (PACE) Diabetes programmed is a large awareness and prevention programmed underway in Chennai conducted among the public to create massive awareness about diabetes and related diseases to reach millions of people.
The limitation of the study is less sample size, patients are from a particular geographic location and there is possibility of biases, as the data were collected based on participants' responses.
Conclusion
Within the limitations of the study, it has been found that the study participants have inadequate knowledge and awareness on oral manifestations of diabetes mellitus. Oral hygiene maintenance practices were poor among diabetic patients and showed poor attitude towards oral care. Health professionals should promote awareness of oral manifestations and complications that arise due to diabetes mellitus among the public to reduce the risk of oral disease.
Acknowledgement
Nil.
Conflict of Interests
None declared.
References
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2006; 29: S43–8.
- Daneman D. Type 1 diabetes. Lancet 2006; 367:847-858.
- Donath MY and Shoelson SE. Type 2 diabetes as an inflammatory disease. Nature Reviews. Immunology 2011; 11:98–107.
- Sicree R. Diabetes and impaired glucose tolerance. Diabetes atlas. Int Diabetes Federation 2006; 15–109.
- Arias E and Smith D. Preliminary data for 2001. National vital statistics reports: from the centers for disease control and prevention, national center for health statistics. National Vital Statistics System 2003; 51:1–45.
- Gadsby R. Epidemiology of diabetes. Adv Drug Delivery Reviews 2002; 54:1165–1172.
- Löe H. Periodontal disease. The sixth complication of diabetes mellitus. Diabetes Care 1993; 16:329–334.
- Taylor GW, Burt BA, Becker MP, et al. Glycemic control and alveolar bone loss progression in type 2 diabetes. Annals Periodontol 1998; 3:30–39.
- Taylor GW. Bidirectional interrelationships between diabetes and periodontal diseases: an epidemiologic perspective. Annals Periodontol 2001; 6:99–112.
- Tanwir F, Altamash M Gustafsson A. Effect of diabetes on periodontal status of a population with poor oral health. Acta Odontologica Scandinavica 2009; 67:129–133.
- Tapper-Jones LM, Aldred MJ, Walker DM, et al. (1981) Candidal infections and populations of Candida albicans in mouths of diabetics. Journal of Clinical Pathology. J Clin Pathol 1981; 34:706-711.
- Moore PA, Guggenheimer J, Etzel KR, et al. Type 1 diabetes mellitus, xerostomia, and salivary flow rates. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont 2001; 92:281–291.
- Ship JA. Diabetes and oral health: An overview. J Am Dent Assoc 2003; 134:4S–10S.
- Abdul Wahab PU, Senthil Nathan P, Madhulaxmi M, et al. Risk factors for post-operative infection following single piece osteotomy. J Maxillofac Oral Surg 2017; 16:328–332.
- Abhinav RP, Selvarasu K, Maheswari GU, et al. The patterns and etiology of maxillofacial trauma in South India. Annals Maxillofac Surg 2019; 9:114–117.
- Eapen BV, Baig MF, Avinash S. An assessment of the incidence of prolonged postoperative bleeding after dental extraction among patients on uninterrupted low dose aspirin therapy and to evaluate the need to stop such medication prior to dental extractions. J Maxillofac Oral Surg 2017; 16:48–52.
- PC J, Marimuthu T, Devadoss P, et al. Prevalence and measurement of anterior loop of the mandibular canal using CBCT: A cross sectional study. Clin Implant Dent Related Res 2018; 20:531–534.
- Jain M and Nazar N. Comparative evaluation of the efficacy of intraligamentary and supraperiosteal injections in the extraction of maxillary teeth: A randomized controlled clinical trial. J Contemporary Dent Prac 2018; 19:1117–1121.
- Marimuthu M, Andiappan M, Wahab A, et al. Canonical Wnt pathway gene expression and their clinical correlation in oral squamous cell carcinoma. Indian J Dent Res 2018; 29:291–297.
- Patil SB, Durairaj D, Suresh Kumar G, et al. Comparison of extended nasolabial flap versus buccal fat pad graft in the surgical management of oral submucous fibrosis: a prospective pilot study. J Maxillofac Oral Surg 2017; 16:312–321.
- Ramadorai A, Ravi P, Narayanan V. Rhinocerebral mucormycosis: A prospective analysis of an effective treatment protocol. Annals Maxillofac Surg 2019; 9:192–196.
- Senthil Kumar MS, Ramani P, Rajendran V, et al. Inflammatory pseudotumour of the maxillary sinus: Clinicopathological report. Oral Surg 2019; 12:255–259.
- Sweta VR, Abhinav RP and Ramesh A. Role of virtual reality in pain perception of patients following the administration of local anesthesia. Annals Maxillofac Surg 2019; 9:110–113.
- Wahab PUA, Madhulaxmi M, Senthilnathan P, et al. (2018) Scalpel versus diathermy in wound healing after mucosal incisions: A split-mouth study. J Oral Maxillofac Surg 2018; 76:1160–1164.
- Smyth S, Heron A. Diabetes and obesity: The twin epidemics. Nature Med 2006; 12:75–80.
- Bakhshandeh S, Murtomaa H, Vehkalahti MM, et al. Oral self-care and use of dental services among adults with diabetes mellitus. Oral Health Prevent Dent 2008; 6:279–286.
- Shanmukappa SM, Nadig P, Puttannavar R, et al. Knowledge, attitude, and awareness among diabetic patients in davangere about the association between diabetes and periodontal disease. J Int Society Prevent Community Dent 2017; 7:381–388.
- Tang YH, Pang SMC, Chan MF, et al. Health literacy, complication awareness, and diabetic control in patients with type 2 diabetes mellitus. J Adv Nursing 2008; 62:74–83.
- Amjad F, Aziz S (2014) Trends awareness and attitudes of patients towards replacement of missing teeth at university college of dentistry. Pakistan Oral Dent J 2004; 34.
- Allen EM, Ziada HM, O’halloran D, et al. Attitudes, awareness, and oral health-related quality of life in patients with diabetes. J Oral Rehab 2008; 35:218-23.
- Almas K, Albaker A, Felembam N. Knowledge of dental health and diseases among dental patients, a multicentre study in Saudi Arabia. Indian J Dent Res 2000; 11:145–155.
Author Info
Kadambari Sriram and Santhosh Kumar MP*
Department of Oral Surgery, Saveetha Dental College, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, IndiaCitation: Kadambari Sriram, Santhosh Kumar MP,Efficacy of Buffered Local Anaesthetics in Dental Practice: A Review, J Res Med Dent Sci, 2020, 8 (7): 268-274.
Received: 16-Sep-2020 Accepted: 02-Nov-2020 Published: 09-Nov-2020