Research - (2021) Volume 9, Issue 6
Is Legacy Technique of Anatomically Bowed Ante Grade Intramedullary Device Fixed at Metaphysis Cancellous Bones & Single Proximal Screw Locking Suffice for Good Outcome in Femoral Fractures?
Vivek Amritbhai Patel, Vishal Ashokraj Pushkarna*, Dhruvin J Patel, Smit Divyesh Bhai Dave and Pranay Bhatt
*Correspondence: Vishal Ashokraj Pushkarna, Department of Orthopaedics, Gujarat Adani Institute of Medical Sciences, India, Email:
Abstract
Introduction: Intramedullary device considered as a load sharing device is one of the commonest surgeries now a days. From the era of straight nails, flexible nails to anatomically curved nails have been used to fix the fractures of the femur. It provides biological environment to the fracture being a potentially closed reduction method. Objective: To measure the outcome of the method of femur fixation by anatomically curved interlocking nail & proximal single locking with two distal locking. Material & Methods: We have studied the (n=37) patients retrospectively. All the fractures treated with femur interlocking nail & proximal single (preferentially dynamic) locking .95% was males & 5% were females in our study. Mean age was 28 years. Fractures were classified by AO classification preoperatively. Results: Mean union time was 22 weeks. (n=34)92 % of patients had excellent outcome & (n=3) 8% had poor outcome. 91.80 % of patients had no limb length discrepancy.70.27% patients of excellent outcome had high velocity trauma & 75% were operated within ten days of trauma incidence. Injury & surgery interval has no effect on the results. Conclusion: Out of different methods of fixation our studied method was anatomically curved femur interlocking nail for treatment of femoral shaft fractures achieves good functional outcome. The single proximal screw allows shorter surgery time, prevents added stress risers at the base of neck & possibly primary dynamicity & callous micro motion. These devices can achieve good anatomical alignment & reduces the future chances of knee arthritis.
Keywords
Anatomical, Femur, Interlocking nail, Metaphysis, Single proximal screw
Introduction
The chances of injury to the human population has increased considerably due to increasing vehicular traffic population and industrialization and one of the most common bone to be fractured is fracture shaft femur. Some of the advantages of nailing are as follows. Intramedullary nail is a load sharing device and bio mechanically an axial fixation of bone which is very important in weight bearing bones. It resists bending and shearing forces and rotational forces and allows axial compressive forces important for early union of fracture. Closed intramedullary nailing apart from preventing exposure of the fracture hematoma important for early healing of bone and prevents damage to the periosteal blood vessels and soft tissues. It allows early weight bearing and joint motion and prevents the dangers of fracture disease.
But except in transverse or short oblique fractures of the isthmic (middle 3rd) region, Kuntscher nailing alone is not ideal. Hence the recent trend is in favour of interlocking nailing of long oblique, comminute or spiral fractures especially in the upper and lower thirds of the shaft because locking provides stability to these highly unstable fractures.
The close technique developed by Kuntscher respects the fracture site and periosteal vascularization by not damaging the soft tissue attachments of the bone fragment and by not disturbing the fracture hematoma. It should be called a ‘Biological Nail’
The shaft is roughly cylindrical and narrowest at its middle; it expands a little as it is traced upwards, but widens appreciably near the lower end of the bone. Its long axis inclines about 10o from the vertical axis of tibia. It is slightly bowed anterolaterally. Crist BD, Wolinsky PR in 2009 studied reamed intramedullary nailing is the current gold standard for the treatment of diaphyseal fractures of the femur [1]. The incidence of shortening was 3.1% as reported by Rothwell et al. [2] reported a 6% incidence of valgus angulation and Winquist & Hansen reported a 2% of angulation in any plane [3]. During the 1960s and 1970s the ideology for femoral fractures treatment was shifted to rigid fixation of the fractures than only external fixation & traction method [4-6]. Intramedullary nailing has almost overcome the concepts of platting for these fractures [7-12]. Comminuted fractures and fractures below isthmus of femoral shaft contain specific biomechanical advantage for the nail fixation. For these type of unstable fractures k-nailing shows poor results [13,14].
Materials and Method
This is a retrospective study of 37 patients and 39 fractures treated with close reduction and femur interlock nailing. All the patients operated by senior orthopaedic surgeon at duration May 2018 to May 2019.
Inclusion criteria: a. Patient with closed femur fracture, b. Patient with associated closed fracture of tibia and other lower limb fractures. Exclusion criteria: a. Patient with compound injuries.
All the femur fractures Patients were thoroughly informed & consented for the procedure. In our series, age varied from 20 to 75 years, with a mean age of 28 years. There was male preponderance. Male: Female ratio was 18:1. AO classification was used to classify the fracture (Table 1). Nail Diameter used in the patient was also noted (Table 2).
| A | B | C | Total | |
|---|---|---|---|---|
| 1.1 | - | - | 1 | 1 |
| 1.2 | - | 4 | 1 | 5 |
| 1.3 | - | 1 | - | 1 |
| 2.1 | 2 | 2 | - | 4 |
| 2.2 | 2 | 5 | 1 | 8 |
| 2.3 | 2 | 2 | - | 4 |
| 3.1 | - | 2 | 1 | 3 |
| 3 | 7 | 1 | - | 8 |
| 2 | ||||
| 3.3 | 3 | 3 | - | 6 |
| Total | 15 | 20 | 4 | 39 |
Table 1: AO classification of our patients. (According to AO classification there were 15 (39%) patients of type A, 20 patients (51%) of type B and 4 patients (10%) of type C.
| Length of Nail (cm) | Patients | Diameter of Nail (mm) | Patients |
|---|---|---|---|
| 36 | 2 (5%) | 8 | 1 (3%) |
| 38 | 11 (27.5%) | 9 | 9 (23%) |
| 40 | 19 (51%) | 10 | 12 (31%) |
| 42 | 4 (11%) | 11 | 13 (34%) |
| 44 | 1 (2.5%) | 12 | 2 (6%) |
Table 2: Number of patients & nail diameter used.(Commonest nail size used 40cm and commonest nail diameter used was 11mm).
Results
In our study (n=35) 95% males & (n=2) 5% were females. In our study 22 patients were between 20-30 years,7 of 31-40,3 of 41-50,3 of 51-60,1 of 61-70,1 of >70 years of age out of (n=37) patients (Figure 1). Right side was affected in 15 patients (39%) and left side was affected in 20 patients (55%) and 2 patients (6%) had bilateral injuries (Figure 2). Associated injury was present in 14 patients includes Tibia fracture, calcaneum fracture. In all patients (100%) fractures united within 9 months. (n=31) patients united within <6 months’ time, 3 patients were united in 6-9 months & 3 patients went for non-union (Figure 3).
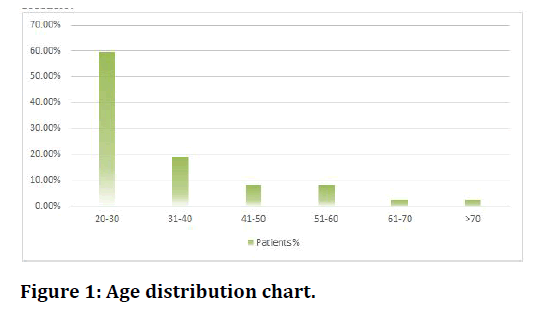
Figure 1. Age distribution chart.
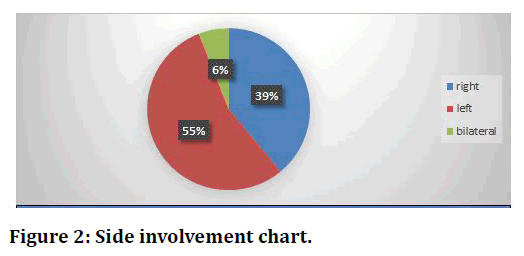
Figure 2. Side involvement chart.
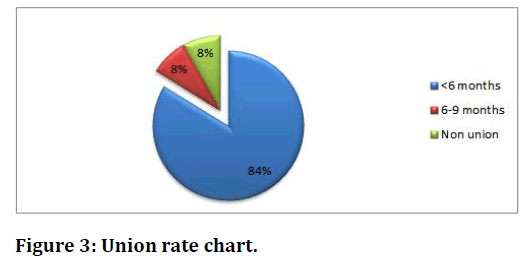
Figure 3. Union rate chart.
But there were three incidences of non-union. Mean union time was 22 weeks.
Minimum follow up was of 1-year duration and maximum follow up was of 6 years, with a mean follow up of 2 years. One patient had complaint of mild pain at the time of final follow-up. In 33 patients walking distance was unlimited. While walking was restricted to 1 km in 3 patients (8.1%). All the patients were able to climb stairs. 33 patients (90%) were able to climb stair without use of banister while only 4 patients (10%) used banister for climbing stairs.32 patients (86.48%) were able to sit cross-legged with ease, 5 patients (13.51%) had some difficulty in sitting cross legged. 34 Patients (91.9%) were able to squat with ease and only 3 patients (8.1%) have difficult to squat. All our patients were able to enter public transport.35 patients (91.80%) had no limb length discrepancy, 3 patients (7.5%) had discrepancy more than 1cm.No patient has lengthening of affected limb. No hip deformities were noted in any case on final follow-up. On final follow up, in 35 patients (95%) implants were in the same position as immediate post operatively.
All except one patient with high velocity trauma had excellent results (Table 3). So even in patients with high velocity trauma results were good. The time between the injury and surgery has not caused any major influence over the results in our study (Table 4). All patients with associated injuries had no bearing on results but had effect on mobilization protocol. 36 of 37 (97.29%) patients treated with closed procedure were united and out of 3 non-union 2 (67%) were treated with open procedure. 1 patient with mild pain had excellent result and 2 patients with poor result have no hip pain because of non-union. 2 patients having no limp but poor result. All patients with no limp had excellent results. 3 patients with non-union (poor result) had mild limp (Table 5). Average hospital stay was around 2 weeks (Table 6).
| Excellent | Good | Fair | Poor | Total | |
|---|---|---|---|---|---|
| Low velocity trauma | 8 (21.6%) | - | - | 2 (6%) | 10(25%) |
| High velocity trauma | 26 (70.27%) | - | - | 1 (2%) | 27(90%) |
| Total | 34 (92%) | - | - | 3 (8%) | 37 |
Table 3: Mode of injuries and results.
| Interval (Weeks) | Excellent | Good | Fair | Poor |
|---|---|---|---|---|
| 7 days | 26 (45%) | - | - | 3 |
| 7-10 days | 8 (30%) | - | - | - |
| > 10 days | 3 (17.5%) | - | - | - |
| Total | 37 (92.5%) | - | - | 3 (7.5%) |
Table 4: Injury to operation interval and results.
| Age | Excellent | Good | Fair | Poor | Total |
|---|---|---|---|---|---|
| 20-30 | 21 | - | 1 | 22 | |
| 31-40 | 6 | - | - | 1 | 7 |
| 41-50 | 3 | - | - | - | 3 |
| 51-60 | 2 | - | - | 1 | 3 |
| 61-70 | 1 | - | - | - | 1 |
| 71-80 | 1 | - | - | - | 1 |
| Total | 34 (92%) | - | 3 (8%) | 37 |
Table 5: Result.
| Stay (Days) | Patients |
|---|---|
| 10-15 | 19 (51.35%) |
| 16-20 | 15 (40.54%) |
| >21 | 3 (8.1%) |
| Total | 37 |
Table 6: Mean hospital stay of our patients was 2½ weeks.
Discussion
In unstable femoral shaft fractures conventional nailing has its own disadvantages viz. (a) Rotational instability which required some form of supplementary fixation or traction or both because of instability there are more chances of delayed and non-union (b) Chances of late collapse at fracture site with resultant limb shortening. So there is more no. of mal union present in fractures treated with K-nailing. (c) In cases of comminute fracture there are more chances of non-union when treated with K-nail because of in adequate stability both rotational and axial.
The use of closed technique gives us the added benefits of biological fixation by not disturbing the fracture hematoma or soft tissue attachments of comminute fragments. In closed technique there is preservation of fracture hematoma, no periosteal stripping less size of incision and minimal blood loss. It is more preferred. Because of this closed technique the fracture biology is well preserved. So, it is called biological fixation.
The concept of locking of intramedullary nail has overcome these difficulties and subsequent long-term experience has shown that interlocking intramedullary nailing is to date the best answer for unstable femoral shaft fractures.
Intramedullary nail is a load sharing device and biomechanically an axial fixation of bone which is very important in weight bearing bones. It resists bending and shearing forces and rotational forces and allows axial compressive forces important for early union of fracture.
This highlights the fact that fractures of shaft of femur are common in relatively younger age group leading to major disability in terms of loss of working man hours. In our study the age varied from 20 to 75 years with mean age of 28 years. 79% of patients in our series in 20 to 40 years age group. Subsequently leading of major disability in terms of loss of working man-hours, the patient being in ‘productive’ age group.
In our series 55% of fractures were comminute these shows that the no. of fractures that we have treated is at par with other series. This high incidence of comminution stresses upon severity of initial trauma and the need for stable fixation. In such type of comminution statically locked nail is preferred over K-nail because such type of fractures required more rotational stability than transverse type of fractures.
In Bansal series there were less no. of comminute fractures than others and our series was at par with Sojbjerg [15] series (Table 7) concluded that static interlocking of intramedullary nails in femoral shaft fractures does not appreciably inhibit the process of healing of the fracture Attal et al. [17]. The optimal time for nailing of closed femoral diaphyseal fracture has been suggested by Brumback et al. [18] as 7–10 days for elective cases and immediately for patients with polytrauma, to allow prompt mobilization.
| R. Brumback et al. [18] | Grosee & Kempf | Pati al. [16] | Sojbjerg et al. [15] | Present Series | |
|---|---|---|---|---|---|
| Union rate | 85 (87) | 47 (52) | 88 (90) | 37 (37) | 34 (37) |
| Union time (in weeks) | 19 | 18 | 24 | 20 | 22 |
| Infection | 1 | 1 | 3 | 0 | 0 |
| Shortening | 2 | 11 | 4 | 5 | 2 |
| Non union | 2 | 5 | 2 | 0 | 3 |
| Knee movement restriction<15o | 0 | 3 | 15 | 3 | 2 |
Table 7: Comparison of results of different study. (We have compared our results with available literature in parameters selected by almost all authors).
We believe that unprotected full weight bearing should not be started before radiological union is present as it may lead to problem of implant failure because locked intra-medullary nail is a load-bearing device and particularly high stresses pass through distal locking screw (Particularly in type IV fractures) which usually bend and break as a result of stresses.
We had allowed weight bearing at 6 weeks on an average after noting definite signs of callus on x-ray. Our results are at par with Bansal et al.
[16] and better than Christi’s series. The early weight bearing in Brumback series (Table 7) was because of more no. of transverse and short oblique fractures.
32 out of 37 patients i.e. 87% there was no restriction of hip movements. Out of 5 patients with restricted hip range of movement 2 has non-union 1 patients has protruding nail tip at pyriformis fossa of 1cm, and 2 patients has restricted hip range of motion because of previous K-nailing. So, all the patients which we have operated primarily have very good hip range of movement. Which is at par with most of the studies both Indian and Western.
At the time of final follow up 89% of patients having no limp. Only 3 patients (11%) have limp at final follow up. All this 3 patients have non-union and because of this non-union they have limp. 33 of 37 (89%) patients were able to walk without any support and only 1 patient was using cane at the time follow-up. On final follow up 87% patients were able to sit cross leg with ease and only 5 patients were able to sit cross leg with difficulty. 92% patients (34) were able to squat with ease.
Being a small incision ante grade nailing entry it has always attracted the surgeons compare to platting. The strong metal biomechanical advantage makes it more attractive than flexible nailing. The retrograde nailing has not shown any knee biomechanical friendliness. The nail offers different locking options being 2-3 proximal to 2-3 distal screws. Our minimal locking screw approach looks attractive but in the presence of great comminution long results to be awaited & we also prefer to go for more locking screws. The optimize use of screws also helps in some micro motion at the fracture site & early vascularization of the fracture callous (Figure 4 to Figure 8).
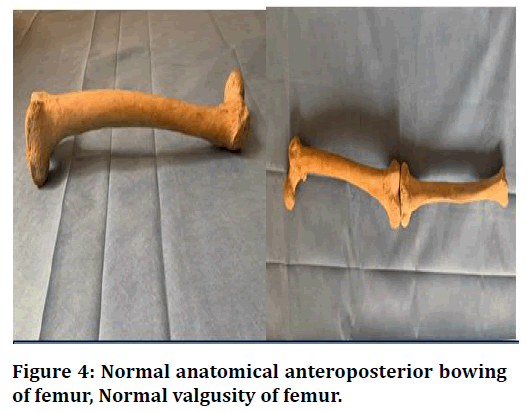
Figure 4. Normal anatomical anteroposterior bowing of femur, Normal valgusity of femur.
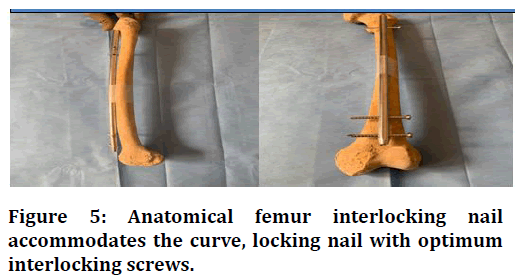
Figure 5. Anatomical femur interlocking nail accommodates the curve, locking nail with optimum interlocking screws.
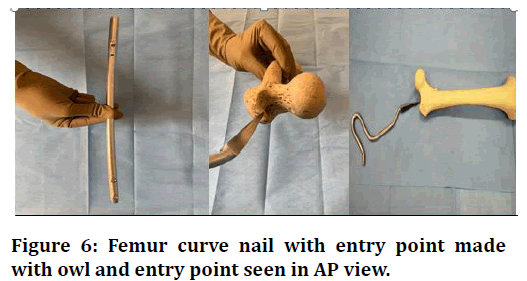
Figure 6. Femur curve nail with entry point made with owl and entry point seen in AP view.
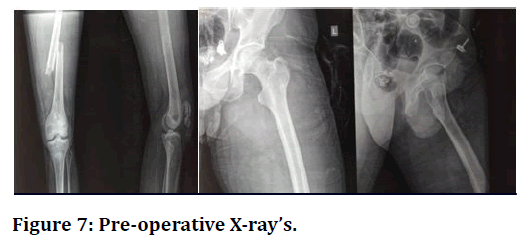
Figure 7. Pre-operative X-ray’s.
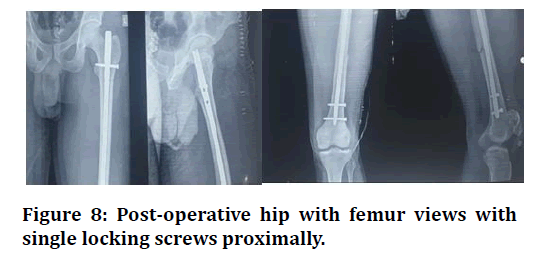
Figure 8. Post-operative hip with femur views with single locking screws proximally.
Conclusion
Anatomically bowed femur interlocking nail from antegrade fashion yields good purchase across the fracture site with locking screws. Single proximal locking screw preferentially dynamic if fracture stable also decrease the chance of stress induction at proximal site. It achieved good functional outcome & early ambulation. All though very large multicentric trials for long duration warranted for this, our results were quite satisfactory reducing the lower limb morbidity.
References
- Crist BD, Wolinsky PR. Reaming does not add significant time to intramedullary nailing of diaphyseal fractures of the tibia and femur. J Trauma Acute Care Surg 2009; 67:727-34.
- Rothwell AG. Closed Kuntscher nailing for comminuted femoral shaft fractures. J Bone Joint Surg 1982; 64:12-6.
- Winquist RA, Hansen ST. Comminuted fractures of the femoral shaft treated by intramedullary nailing. Orthop Clin North Am 1980; 11:633-48.
- Obletz BE. Vertical traction in the early management of certain compound fractures of the femur. J Bone Joint Surg 1946; 28:113-6.
- Denker H. Shaft fractures of the femur: A comparative study of the results of various methods of treatment in 1003 cases. Acta Chir Scand 1965; 130:173-84.
- Seligson D, Harman K. Negative experiences with pins in plaster for femoral fractures. Clin Orthop 1979; 138:243-5.
- Gant GC, Shafton GW, Herbsman H. Experience with the ASIF compression plate in the management of femoral shaft fractures. J Trauma 1970; 10:458-71.
- Fisher WD, Hamblen DL. Problems and pitfalls of compression fixation of long bone fractures: A review of results and complications. Injury 1978; 10:99-107.
- Decoster TA, Miller RA. Closed lock intramedullary nailing of femoral shaft fractures in the elderly. Lowa Orthop J 2003; 23:43-5.
- Devnani AS. Open reamed femoral intramedullary nailing – revisited. Eastern J Med 2003; 8:7-11.
- Meena RC, Kundani V, Hussain Z. Fractures of the shaft of femur closed versus open interlocking intramedullary nailing. Indian J Orthopadics 2006; 49:243-6.
- Bashir A, Mir BA, Halwai MA, et al. First experience with locked intramedullary nailing of femur in Kashmir. Internet J Orthop Surg 2008; 8:1.
- Kyle RF, Schaffhausen JM, Bechtold, JE. Biomechanical characteristics of interlocking femoral nails in the treatment of complex femoral fractures. Clin Orthop Related Res 1991; 267:169-73.
- Bankston AB, Keating M, Saha S. The biomechanical evaluation of intramedullary nails in distal femoral shaft fractures. Clin Orthop Related Res 1992; 276:277-82.
- Søjbjerg JO, Eiskjaer S, Møller-Larsen F. Locked nailing of comminuted and unstable fracturesof the femur. J Bone Joint Surg Br 1990; 72:23-25
- Pati BN, Bansal VP, Krishna LG, et al. Interlocking nail of femur. A review of 90 cases. Ind J Orthop 2001; 35:49-51.
- Attal R, Blauth M. Unreamed intramedullary nailing, Sports Traumatol Med University Germany 2010; 39:182-91.
- Brumback RJ, Uwagie-Ero S, Lakatos RP, et al. Intramedullary nailing of femoral shaft fractures. Part II: Fracture-healing with static interlocking fixation. J Bone Joint Surg Am 1988; 70:1453-62.
Author Info
Vivek Amritbhai Patel, Vishal Ashokraj Pushkarna*, Dhruvin J Patel, Smit Divyesh Bhai Dave and Pranay Bhatt
Department of Orthopaedics, Gujarat Adani Institute of Medical Sciences, India1Department of Orthopaedics, Gujarat Adani Institute of Medical Sciences, India
2Department of Orthopaedics, Gujarat Adani Institute of Medical Sciences, India
3Department of Orthopaedics, Gujarat Adani Institute of Medical Sciences, India
4Department of Orthopaedics, Gujarat Adani Institute of Medical Sciences, India
Citation: Vivek Amritbhai Patel, Vishal Ashokraj Pushkarna, Dhruvin J Patel, Smit Divyesh Bhai Dave, Pranay Bhatt,Is Legacy Technique of Anatomically Bowed Ante Grade Intramedullary Device Fixed at Metaphysis Cancellous Bones & Single Proximal Screw Locking Suffice for Good Outcome in Femoral Fractures?, J Res Med Dent Sci, 2021, 9(6): 319-324
Received: 02-Apr-2021 Accepted: 23-Jun-2021 Published: 06-Mar-2021
