Research - (2019) Volume 7, Issue 2
Investigating the Effect of Remote Limb Ischemic Preconditioning in Preventing Delirium in Patients Candidate for Coronary Artery Cardiopulmonary Bypass in Bushehr Heart Hospital
Abdolrasoul Anvaripour1, Leila Nasserikhah2, Parviz Azodi1, Rahim Tahmasebi3, Soheila Esfandiari2, Mohammad Hussein Ebrahimi4 and Faezeh Jahanpour5*
*Correspondence: Faezeh Jahanpour, Faculty of Nursing and Midwifery, Bushehr University of Medical Sciences, Bushehr, Iran, Email:
Abstract
Background: Delirium is one of the common complications following open-heart surgery. Delirium is a fluctuating cognitive impairment and consciousness disorder and a common as well as acute problem for patients hospitalized in hospitals, complicating the course of patient improvement. Ischemic preconditioning can be a method to mitigate delirium of patients. The aim of the study is to investigate the effect of remote limb ischemic preconditioning in preventing delirium in patients undergoing coronary artery bypass graft surgery.
Methods: The present study is a randomized clinical control trial performed as interventional before and after intervention and control groups. The research population consisted of patients hospitalized in the ICU ward of Heart Center hospital of Bushehr city (Iran) to undergo CBAG or referred electively. In this plan, 80 patients participated chosen through convenient sampling, and then randomly assigned into intervention and control groups. The research instrument was demographics information form and Neecham scale to investigate the incidence of delirium. The data were analyzed by SPSS 22, whereby chi-do, Mann-Whitney, and Friedman nonparametric analysis of variance were used.
Findings: The mean delirium score before the intervention in the test group was 27.9 with standard deviation of 0.35, and in the control group it was 29.8 with standard deviation of 0.48 (p=0.399), which was the same in the two groups before the intervention and had no significant difference. The mean score of delirium after the intervention in the test group was 27.9 with standard deviation of 0.89 and in the control group it was 27.8 with a standard deviation of 0.96, suggesting insignificant difference between intervention and control groups.
Conclusion: The results of this research indicated that remote limb ischemic preconditioning cannot result in mitigation of delirium in CABG patients.
Keywords
Ischemic preconditioning, Delirium, Coronary artery bypass, Heart surgery, Nursing
Introduction
Cardiovascular disease is the most important cause of mortality worldwide. Every 42 seconds, one heart attack and everyone minute one cardiovascular disease mortality occur [1,2]. Currently, the mortality caused by coronary artery disease in Iran is increasing, claiming 46% of the causes of mortalities, whose incidence is 4.181 per 100,000 individuals [3].
In the US, around 598000 cases of coronary artery bypass graft is performed annually. Although great advances have been made in pharmacotherapy and catheterization methods, surgical interventions are still the cornerstone in the treatment of these diseases [4]. In Iran, annually 25,000 open-heart surgery occur, with CABG claiming 50%-60% of them [5]. According to studies, in the US the number of CABG operations has increased, and similarly in Iran 60% of all cardiovascular operations are related to CABG [6]. In spite of provision of intensive care to patients following heart surgery, incidence of some complications following heart surgery is inevitable.
The problems and complications following heart surgery are mostly due to underlying diseases and the trauma caused by the operation. The most important complications include electrolyte disorders, impaired gas exchange, myocardial infarction, kidney failure, hemorrhage, and neurological complications [7]. In the study by Jannati et al., 26 (12.32%) patients suffered neurological complications, out of home 23 (10.90%) had found cognitive problems [8].
The patients that develop delirium during hospitalization are 20%-75%, and 15% of them die within one months, and 25% die within 6 months. The maximum rate of incidence of delirium has been reported following thoracotomy and cardiotomy operations, whose statistics even reach 90% [9,10]. Although delirium may develop at any time during hospitalization in hospital, typically it develops early postoperatively.
Today, delirium is one of the major concerns of staff in ICU wards especially for nurses [11]. Presence of delirium is a bad sign in terms of prognosis, which is associated with high mortality. In this regard, after three months, 23%-33% of those who have experienced a course of delirium die, where this figure sometimes reaches 5% [12].
Incidence of delirium at admission in hospital is 14%-24%, and during hospitalization it grows up to 56% [13]. The rate of incidence of delirium in patients undergoing open-heart surgery has been reported as 32%-72%. Complications of delirium remain in at least 20% of patients above 65 years of age, and increase the hospital costs for every patient by $2500 and annually around $6.9 billion [14,15].
Studies have propounded different factors to be associated with incidence of delirium including complication and duration of open-heart surgery, use of cardiopulmonary bypass, presence of micro-emboli resulting from aorta and manipulation of the heart, cerebral blood resupply damage, old-age, severity of disease, presence of chronic disease, mechanical ventilation, moving limitations, infection, metabolic disorders, hypoxia, longer hospitalization in ICU, and laboratory changes [16,17].
Among the important reasons following surgery are stress of operation, postoperative pain, insomnia, consumption of analgesics, electrolyte disorder, fever, and hemorrhage [18,19]. Considering the increase in heart surgery operations and increased age of patients at the time of surgery, complications such as postoperative delirium are growing in response [20].
Both coronary artery bypass graft and coronary artery bypass surgery without pump require some special strategies to reduce development of delirium following surgery [21]. Pain mitigation can also reduce the risk of incidence of delirium. Nevertheless, research has shown that these methods have not been able to resolve the problem [22,23].
Remodeling ischemic preconditioning is an attractive strategy to reduce myocardial damage and contain myocardial infarction and improve reperfusion. It also significantly decreases the damage caused by reperfusion ischemia in most human tissues including myocardium and brain. It also decreases hypoxia, through which it has been assumed that it can also be involved in mitigating delirium. Some recent randomized controlled experiments in humans have reported that remote limb ischemic preconditioning leads to improved cardiac output [24].
Ischemic preconditioning is a widely established concept. The clinical use of ischemic preconditioning was published by Konstantinov et al. [25]. This assumption that remote limb ischemic preconditioning decreases incidence of delirium postoperatively and prevents aggravation of short-term cognitive function following surgery under isoflurane-phentanyl anesthesia has been tested in patients undergoing heart surgery using cardiopulmonary bypass [26-28].
Some studies have shown the application of remote limb ischemic preconditioning before angioplasty capable of enhancing cardiac recovery [29,30]. In a study, the effect of remote limb ischemic preconditioning in protecting the brain against the damage caused by stopped hypothermic blood circulation has been observed [31].
Although local ischemic preconditioning is a result of short-term nonfatal ischemia in the target tissue, its usefulness has been shown in patients undergoing angioplasty of coronary arteries and artery operations in some studies [32]. In a randomized control study, the effects of remote limb ischemic preconditioning has been examined in children undergoing repair of congenital heart defect, causing reduction of damage caused by reperfusion ischemia in remote limbs [33].
Some evidence has been presented for remote limb ischemic preconditioning (RSP) in humans by showing protection against endothelial function disorder generated by stable ischemia and reestablishment of blood circulation in an arm following transient ischemia in the other arm among healthy individuals [34,35].
It suggested that RSP in patients undergoing open repair of abdominal aortic aneurysm decreases incidence of damage following cardiac operation, heart attack, and kidney failure [36]. Nurses play a special role in providing care for patients and are in contact with patients more than other members of the treatment team.
Since the rate of delirium is high in patients hospitalized in ICUs and following heart surgery, by decreasing delirium it is possible to better achieve nursing objectives including mitigation of pain and anxiety, thereby taking effective steps for patient improvement and better care. The aim of the present study is to investigate the effect of RSP in preventing delirium in candidate patients of coronary artery cardiopulmonary bypass in Heart Hospital of Bushehr in 2017.
Materials and Methods
The present research is a randomized controlled clinical trial study performed as pre- and post-interventional. The research population consisted of patients who were hospitalized in the mentioned hospital in the ICU ward of heart surgery or referred electively. In this study, 80 patients participated chosen through available sampling, and then randomly assigned into intervention and control groups. In this study, the research context was Bushehr Heart Hospital, and the place where the research was conducted was open-heart surgery ward of this hospital.
Inclusion criteria included all elective patients candidate for coronary artery cardiopulmonary bypass, age 55 years-70 years, and patients with EF>35.
Exclusion criteria included patients who were retransferred to operation room due to excessive bleeding after heart surgery, placing intra-aortic balloon pump (IABP) in the operation room or ICU ward due to left ventricle dysfunction (LV dysfunction), acute MI patients (patients who had recently experienced heart attack), patients with history of diabetes mellitus (DM), patients with history of stroke, patients with peripheral vascular problems of upper limbs, patient’s unwillingness to continue participation in the study in spite of initial consent, transference of patient to another healthcare center, consumption of psychotropic drugs, history of psychological disorders such as psychosis and mental retardation, and presence of ST changes during operation.
The sample size in this study to evaluate the effectiveness at first-type error level of α=0.05 and test power of 0.80 based on the findings of Hudetz et al. who had reported the mean cognitive disorder score 7 days following heart surgery in the intervention and control groups as 10 ± 5 and 8 ± 4 [21] according to the formula of the sample size of comparison of means was estimated as 40 subjects for each group, and totally 80 subjects.
The research instrument included demographic information form of hospitalized patients including age, gender, marital status, education, history of hypertension, hyperlipidemia, history of previous diseases, smoking, and drug abuse. The second instrument was Neecham scale which can be used as a rapid and non-stop instrument on the patient’s bedside for assessing the patient behavior to examine possible incidence of delirium [11].
This 30-score questionnaire has been developed according to DSM III-R criteria and 24-hour activity of nurses. The total acquired score is categorized into four groups: health individual (score: 27-30), on the verge of confusion (score: 25-26), mild delirium (score: 20-24), and severe delirium (score: 0-19). The time for filling in the questionnaire is 5-10 min. This instrument was prepared through a paper called examining the effect of multifactorial intervention on incidence of delirium in heart surgery ICU ward performed by Zeyghami et al. [11].
First the questionnaire used by Zeyghami et al. was translated from English to Persian. After translation, to evaluate the content validity in Iran, the opinions of experts in this area (one psychiatrist and the psychologist nurses) were benefited from, and based on the criteria of fluency, relevancy, and clarity of questions; their corrective opinions were applied [11].
Measurement of the reliability of this instrument was performed through internal consistency and equivalence. In evaluating the internal consistency, the Cronbach alpha coefficient was obtained as 0.96. In measuring the equivalence, Pearson correlation was obtained as 0.99 [11].
After acquiring the necessary permissions from the research deputy of Bushehr University of medical sciences and receiving the ethics code, first the objectives of this study were explained to the patients. They were also assured that anytime they desired they could leave the study. Eventually, written informed consent form was received from them.
After selection of samples, the night before the openheart surgery, the psychological status of patients was examined by delirium checklist, after which intervention was initiated. In this study, diagnosis of delirium was performed by nurse based on the escort acquired from the questionnaire the night before the operation and on a daily basis up to five days following operation. Since the intensity of delirium and its incidence are greater at evenings, measurement of delirium was performed every evening at 18:00-20:00.
The type and dosage as well as hour of consumption of the utilized drugs as sample (haloperidol if required) were also introduced into the questionnaire.
In this plan, an interventional method called remote limb ischemic preconditioning was applied after induction of anesthesia using a swollen blood pressure cuff with the width of 9-12 cm, which was wrapped in the upper part of the arm of the subjects. The cuff pressure value around the arm was 200 mmHg. The duration of cuff filling was 5 min, which was then emptied within 5 min, and was performed in three cycles totally recording 30 min by an anesthesiologist. Also, ST changes during operation were considered; if any changes were observed, those interventions were stopped.
The method of anesthesia was the same in both groups and performed by the same method. In all of the patients, before induction using topical anesthesia with lidocaine 1% arterial line with catheter No. 20 in left radial artery was devised. After establishing electrocardiography monitoring and SPO2 and arterial line, induction of anesthesia was initiated. In the induction method, the medications that are not involved in incidence of ischemic preconditioning including otomidit+sufentanyl +midazolam were considered.
After intubation and CVP placement, in the maintenance stage of removal of inhlatory drugs of isoflurane and soflutane and the application of infusion of sufentanyl +midazolam+atracurium drugs, they patients were managed. All of the patients received oxygen 100% during the anesthesia stages. After completion of the surgery, the patients were transferred to ICU ward, and underwent invasive monitoring by arterial line and CVP for at least 4 h-6 h. Considering the relevant indices, separation of patients from the intubation device was performed. The data were analyzed by SPSS 22, where Chi-do, Mann-Whitney, and Friedman nonparametric analysis of variance were used.
Results
Comparison of two groups with Chi-square and independent T-test showed that two groups of intervention and control in terms of all demographic characteristics including: age, sex, marital status, education, smoking, history of blood pressure, history of blood lipids, family history of heart disease, The history of previous admission and thyroid disease were the same and did not have a significant difference.
The mean score of delirium before the intervention in the test and control groups was 29.9 ± 0.35 and 29.8 ± 0.48 (p=0.399) respectively, where the two groups were the same before the intervention and had no significant difference.
The mean score of delirium after the intervention in the test and control groups was 27.9 ± 0.48 and 27.8 ± 0.48 respectively, suggesting absence of significant difference between the two groups.
Compared the mean score of delirium pre and post of intervention showed decreased score in tow group but it’s not significant in each group (Table 1). Therefore, Compare Change pre and post intervention was not significant (p=0.923).
| Group | Control | Intervention | p-value |
|---|---|---|---|
| Pre intervention | 29/8 | 29/9 | 0/399 |
| Post intervention | 27/8 | 27/9 | 0/738 |
| Compare Change pre and post | -2 | -1/975 | 0/923 |
Table 1: Comparison of mean score of delirium pre and after intervention in control and intervention group
The mean score of delirium during five days of measurement after intervention in both groups had significant changes (p<0.001), such that the first day after the intervention compared to pre-intervention showed diminished delirium in both groups (p<0.001).
However, on days 2 and 3 compared to their previous day, no significant change was observed in the mean score of delirium. Further, on day 5 compared to day 4, a significant reduction of mean delirium score was observed in both groups (p<0.001).
The mean score of delirium on the first day after the intervention in the test and control groups was 27.2 ± 0.15 and 26.1 ± 8.53, respectively, showing no significant difference with each other (p=0.283).
Again, according to the classification of situation of individuals in terms of intensity of delirium, as can be observed in Figure 1, the two groups have the same situation.
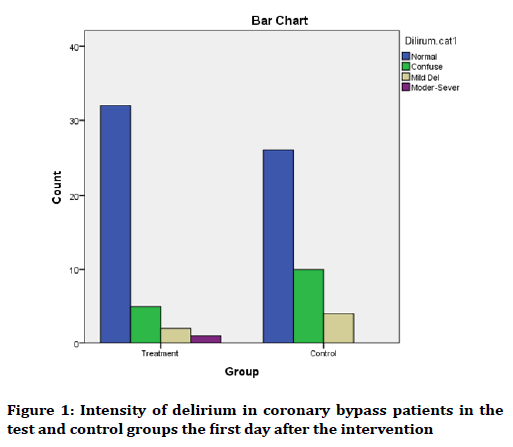
Figure 1. Intensity of delirium in coronary bypass patients in the test and control groups the first day after the intervention
The mean score of delirium on the second the postintervention in the test and control groups was 27.1 ± 3.36 and 27.1 ± 4.10, respectively, where the two groups had no significant difference with each other (p=0.973). The classification of status of individuals in terms of intensity of delirium as can be seen in Figure 2 is similar.
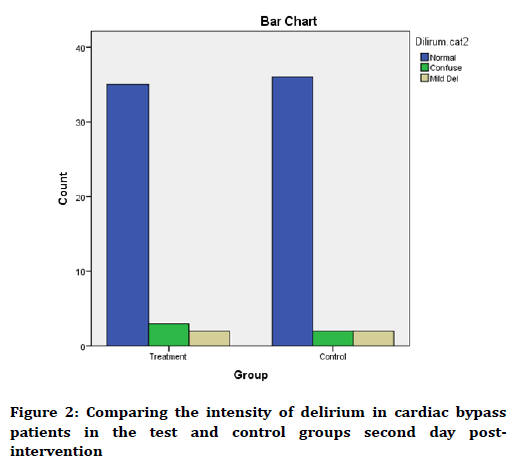
Figure 2. Comparing the intensity of delirium in cardiac bypass patients in the test and control groups second day postintervention
The mean score of delirium on the third day following intervention in the test and control groups was 27.0 ± 9.71 and 27.1 ± 4.78, respectively, where the two groups had no significant difference (p=0.286).
According to classification of status of individuals in terms of intensity of delirium, as observed in Figure 3, the two groups have the same status.
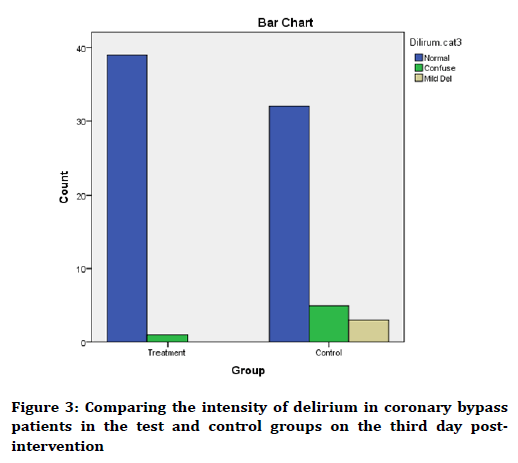
Figure 3. Comparing the intensity of delirium in coronary bypass patients in the test and control groups on the third day postintervention
The mean score of delirium on the fourth day postintervention in the test and control groups was 27.2 ± 8.19 and 28.1 ± 3.49, respectively, where the two groups had no significant difference with each other (p=0.429). According to classification of status of the subjects in terms of intensity of delirium, as can be seen in Figure 4, the two groups have the same status.
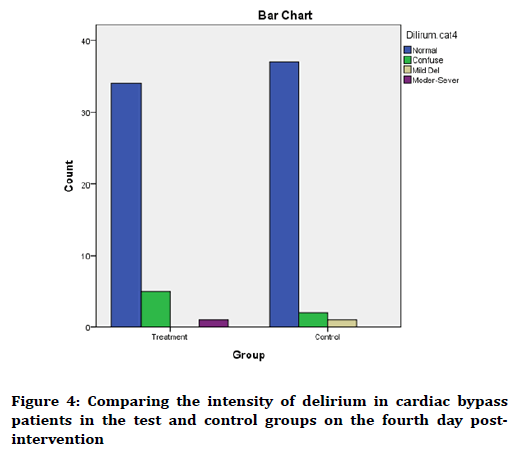
Figure 4. Comparing the intensity of delirium in cardiac bypass patients in the test and control groups on the fourth day postintervention
The mean score of delirium on the fifth day postintervention in the test and control groups was 29.0 ± 5.95 and 29.1 ± 17.10, respectively, where the two groups had no significant difference with each other (p=0.064). According to classification of status of subjects in terms of intensity of delirium, as observed in Figure 5, the two groups have the same status.
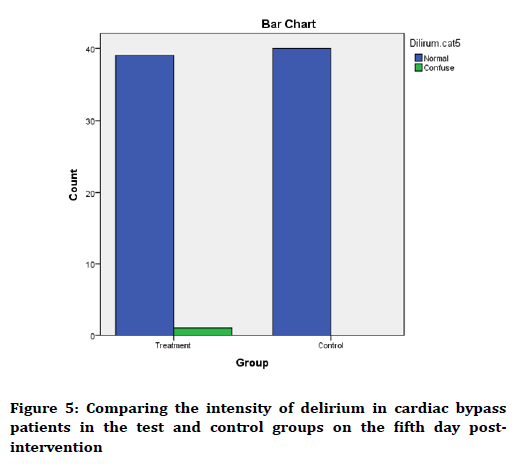
Figure 5. Comparing the intensity of delirium in cardiac bypass patients in the test and control groups on the fifth day postintervention
Discussion
The findings obtained from comparing the demographic factors between the intervention and control groups using Chi-do test showed that the two groups had no significant difference with each other in terms of age, gender, marital status, education, smoking, history of hypertension, history of lipidemia, family history of heart disease, history of previous disease, and thyroid disease.
However, generally the number of men and married subjects was higher in both groups than women and married subjects.
The mean score of delirium before the intervention in the test and control groups was 29.9 and 29.8 respectively, where no significant difference was observed. This finding is in accordance with the study by Meybohm et al. entitled “neurological disorders in patients undergoing heart surgery following remote limb preconditioning” performed in 2013 in Germany on 180 patients undergoing elective heart surgery using cardiopulmonary pump with the aim of decreasing neurological disorders following surgery in patients undergoing complicated cardiac surgery [37].
On the first day following operation, 8% (n=7) of individuals experienced mild to severe degrees of delirium. Although the number of these individuals was higher in the control group than in the intervention group, the difference was not significant.
In the same vein, the mean scores of delirium were not significant between the two groups in any of the stages that this finding is in line with the result obtained by Joung et al. in South Korea. They conducted a study entitled the effect of remote limb ischemic preconditioning on the cognitive function following usage of coronary artery pump in cardiac bypass surgery on seven to patients undergoing cardiac bypass surgery using coronary artery pump. In this study, they used cognitive function test.
The intervention involved remote limb ischemic and they concluded that this preconditioning was not able to decrease the incidence of cognitive disorder following surgery at the period after the cardiac bypass surgery [35]. The difference of this study with ours lies in use of different cognitive function test.
The results of the study by Meybohm et al. entitled “neurological disorders in patients undergoing heart surgery following remote limb preconditioning” in Germany support our findings. This research had been performed on 180 patients undergoing elective heart surgery using cardiopulmonary pump with the aim of reducing neurological disorders following surgery in patients undergoing complicated cardiac surgery. The results suggested that remote limb preconditioning was not effective, and thus further studies are required [37]. The difference of this study with ours lies in use of a larger sample size and more cycles.
On the other hand, the results of our study are incongruent with the clinical trial (pilot) research by Hudetz et al. in the US. They conducted a study entitled remote limb ischemic preconditioning in preventing short-term cognitive function disorder after cardiac surgery using cardiac bypass on 30 patients. The studied population included individuals undergoing elective coronary artery surgery or valvuloplasty using cardiac bypass. They used delirium screening checklist of ICU ward. In this study, remote limb ischemic preconditioning was performed in four 5 min cycles. They found that this preconditioning prevent aggravation of short-term cognitive function after operation [21].
The results of this study are incongruent with ours. The difference has been in the method of implementation, where they used four cycles which might have caused incongruent results. Also, it has considered cognitive function generally, while we only investigated one of the subsets of cognitive function i.e. delirium.
Also, in another study performed as animal clinical trial study by Xu et al. in Shanghai, China. The results suggested that the preconditioning can protect the neurocognitive function of rats after the bilateral occlusion of carotid arteries [36]. The results of this study have been incongruent with ours. The difference lied in the method utilized, who used 10 min cycles instead of 5 min cycles, which might have caused development of incongruent results. Also, the animal nature of the studied samples can be another cause of discrepancy.
Investigation of the mean scores of delirium on consecutive days indicated that over time the patients tended to improve, and the number of individuals with mild and severe delirium decreased. This finding has been in line with the study by Zeyghami et al. [11] entitled “investigating the effect of multifactorial intervention on incidence of delirium in heart surgery ICU ward”. This research was of non-random clinical trial type on 96 patients hospitalized in ICU ward of heart surgery of Buali Hospital in Qazvin. The patients had been chosen by available sampling and assigned into control and intervention groups. First, 48 patients in the control group were examined in terms of incidence of delirium and after discharge of the last subject of the control group, the sampling and interventions were performed in the intervention group with 48 patients.
The intervention included three components: professional, environmental, and patient-associated. To investigate the level of delirium, a questionnaire similar to the one used here was used, and the level of delirium was checked before the operation and four consecutive days after the operation on a daily basis. The results of this study showed that the delirium level decreased from the first day post-operation up to the fourth day.
Limitations
Among the limitations of the intervention are history of diabetes and recent heart attack in most patients and their exclusion from the study, and in turn prolongation of the duration of the plan. On the other hand, the low number of cycles has been one of the other factors contributing to the effectiveness of the intervention.
Conclusion
The results obtained from this research showed that remote limb ischemic preconditioning cannot lead to diminished delirium in patients with coronary artery bypass graft surgery. Accordingly, it seems that further studies are required.
Acknowledgments
The research deputy of Bushehr University of medical sciences (IRCT Code: IRCT2017041712830N21 and Ethics code: IR.BPUMS.REC.1395.210) is highly appreciated for funding the research as well as all the individuals who cooperated in some way in this study including their personnel of the Heart hospital for their cooperation along with patients.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics-2016 update a report from the American Heart Association. Circulation 2016; 133:e38-48.
- Amirian Z, Maslakpak MH, Jalali R, et al. The effects of regular physical activity at home on patients' quality of life after coronary artery bypass surgery. JKH 2013; 8:51-6.
- Salari A, Hassandokh T, Tirani HD, et al. Delirium after open heart surgery: The role of distress and preoperative depression in its occurrence. J Guilan Univ Med Sci 1935; 26:36-45.
- Hosseinian A, Kasayi V, Mohammadzade A, et al. Evaluation of early complications of coronary artery bypass grafting surgery (CABGS) in the first month after operation in Imam Khomeini Hospital of Ardabil during 2013-2014. JAUMS 2014; 14:18-27.
- Pour MI, Basampour SS, Bahrani N. The relationship between preoperative variables of coronary artery bypass graft versus extubation time of patients. Iran J Nurs Midwifery Res 2006; 12:5-16.
- Rad M, Mohammadi N, Seyyedshohadaee M, et al. Relationship of blood transfusion and CPB with delirium. JSUMS 2014; 20:801-7.
- Devlin JW, Skrobik Y. Antipsychotics for the prevention and treatment of delirium in the intensive care unit: What is their role? Harv Rev Psychiatry 2011; 19:59-67.
- Jannati l, Nesamy MB, Sohrabi M, et al. Incidence of delirium and associated factors before open heart surgery. J Res Develop Nurs Midwifery 2013; 10:33-42.
- Derakhshanfar A, Ghaleiha A, Niayesh A, et al. Assessment of the frequency of cognitive disorder in older patients before and after surgery in Hamadan Educational Hospitals. Iranian J Surg 2010; 18:1-10.
- Astaneh AN, Mugheyn NK, Pakseresht S, et al. Investigating the multidimensional interventive effect on delirium in patients after open heart Surgery. AJUMS 2006; 6:141-8.
- Zeyghami R, Heydari MA, Babaee R. Effect of a multifactorial intervention on the incidence of delirium in cardiac surgery unit. IJPN 2015; 3:48-57.
- Zolfaghari M, Arbabi M, Razi SP, et al. Effectiveness of a multifactor educational intervention on delirium incidence and length of stay in patients with cardiac surgery. TUMS 2012; 18:67-78.
- Hollinger A, Siegemund M, Goettel N, et al. Postoperative delirium in cardiac surgery: An unavoidable menace? J Cardiothorac Vasc Anesth 2015; 29:1677-87.
- Hudetz JA, Iqbal Z, Gandhi SD, et al. Postoperative delirium and short-term cognitive dysfunction occur more frequently in patients undergoing valve surgery with or without coronary artery bypass graft surgery compared with coronary artery bypass graft surgery alone: Results of a pilot study. J Cardiothorac Vasc Anesth 2011; 25:811-6.
- Heidari AH, Dianti M, Mousavi GA. Determine the frequency of delirium, its related factors and its short-term consequences in patients admitted to the intensive care units of Shaheed Beheshti Hospital in Kashan and Kashani, Isfahan during 2012. Feyz Sci-Res Bulletin 1933; 18:76-84.
- Jannati Y, Nesamy MB, Sohrabi M, et al. Incidence of delirium and associated factors before open heart surgery. J Res Develop Nurs Midwifery 2013; 10:33-42.
- Jouybari LM, Hosseini SF, Ghana S, et al. The incidence of delirium in patients after surgery in recovery room. Faraz J 2012; 14:23-9.
- Trabold B, Metterlein T. Postoperative delirium: Risk factors, prevention, and treatment. J Cardiothorac Vasc Anesth 2014; 28:1352-60.
- Hausenloy DJ, Yellon DM. Remote ischaemic preconditioning: Underlying mechanisms and clinical application. Cardiovasc Res 2008; 79:377-86.
- Yellon DM, Hausenloy DJ. Realizing the clinical potential of ischemic preconditioning and postconditioning. Nat Rev Cardiol 2005; 2:568.
- Hudetz JA, Patterson KM, Iqbal Z, et al. Remote ischemic preconditioning prevents deterioration of short-term postoperative cognitive function after cardiac surgery using cardiopulmonary bypass: Results of a pilot investigation. J Cardiothorac Vasc Anesth 2015; 29:382-8.
- Jahanpour F, Sharif F, Salsali M, et al. Clinical decision‐making in senior nursing students in Iran. Int J Nurs Pract 2010; 16:595-602.
- Rabiei Z, Jahanpour F, Azodi F, et al. Effect of educational multimedia on anxiety before cesarean section. IJOGI 2017; 20:24-9.
- Konstantinov IE, Li J, Cheung MM, et al. Remote ischemic preconditioning of the recipient reduces myocardial ischemia-reperfusion injury of the denervated donor heart via a Katp channel-dependent mechanism. Transplantation 2005; 79:1691-5.
- Konstantinov IE, Arab S, Kharbanda RK, et al. The remote ischemic preconditioning stimulus modifies inflammatory gene expression in humans. Physiol Genomics 2004; 19:143-50.
- Pinaud F, Corbeau JJ, Baufreton C, et al. Remote ischemic preconditioning in aortic valve surgery: Results of a randomized controlled study. J Cardiol 2016; 67:36-41.
- Yamanaka T, Kawai Y, Miyoshi T, et al. Remote ischemic preconditioning reduces contrast-induced acute kidney injury in patients with ST-elevation myocardial infarction: A randomized controlled trial. Int J Cardiol 2015; 178:136-41.
- Jensen HA, Loukogeorgakis S, Yannopoulos F, et al. Remote ischemic preconditioning protects the brain against injury after hypothermic circulatory arrest. Circulation 2011; 123:714-21.
- Gersh BJ. Cardiac remote ischemic preconditioning in coronary stenting (CRISP Stent) Study: A prospective, randomized control trial. Year Book of Cardiology 2010; 2010:366-7.
- Cheung MM, Kharbanda RK, Konstantinov IE, et al. Randomized controlled trial of the effects of remote ischemic preconditioning on children undergoing cardiac surgery: First clinical application in humans. J Am Coll Cardiol 2006; 47:2277-82.
- Kharbanda R, Mortensen U, White P, et al. Transient limb ischemia induces remote ischemic preconditioning in vivo. Circulation 2002.
- Davies WR, Brown AJ, Watson W, et al. Remote ischemic preconditioning improves outcome at 6 years after elective percutaneous coronary intervention: The CRISP stent trial long-term follow-up. Circ Cardiovasc Interv 2013; 6:246-51.
- Loukogeorgakis SP, Panagiotidou AT, Broadhead MW, et al. Remote ischemic preconditioning provides early and late protection against endothelial ischemia-reperfusion injury in humans: role of the autonomic nervous system. J Am Coll Cardiol 2005; 46:450-6.
- Ali ZA, Callaghan CJ, Lim E, et al. Remote ischemic preconditioning reduces myocardial and renal injury after elective abdominal aortic aneurysm repair: A randomized controlled trial. Circulation 2007; 116:98-105.
- Joung KW, Rhim JH, Chin JH, et al. Effect of remote ischemic preconditioning on cognitive function after off-pump coronary artery bypass graft: a pilot study. Korean J Anesthesiol 2013; 65:418-24.
- Xu T, Gong Z, Zhu WZ, et al. Remote ischemic preconditioning protects neurocognitive function of rats following cerebral hypoperfusion. Med Sci Monit 2011; 17:BR299.
- Meybohm P, Renner J, Broch O, et al. Postoperative neurocognitive dysfunction in patients undergoing cardiac surgery after remote ischemic preconditioning: A double-blind randomized controlled pilot study. PLoS One 2013; 8:e64743.
Author Info
Abdolrasoul Anvaripour1, Leila Nasserikhah2, Parviz Azodi1, Rahim Tahmasebi3, Soheila Esfandiari2, Mohammad Hussein Ebrahimi4 and Faezeh Jahanpour5*
1Faculty of Paramedicine, Anesthesiology Department, Bushehr University of Medical Sciences, Bushehr, Iran2Student Research Committee, Bushehr University of Medical Sciences, Bushehr, Iran
3School of Public Health, Bushehr University of Medical Sciences, Bushehr, Iran
4Nursing, Hearth Hospital, Bushehr University of Medical Sciences, Bushehr, Iran
5Faculty of Nursing and Midwifery, Bushehr University of Medical Sciences, Bushehr, Iran
Citation: Abdolrasoul Anvaripour, Leila Nasserikhah, Parviz Azodi, Rahim Tahmasebi, Soheila Esfandiari, Mohammad Hussein Ebrahimi, Faezeh Jahanpour, Investigating the effect of remote limb ischemic preconditioning in preventing delirium in patients candidate for coronary artery cardiopulmonary bypass in Bushehr heart hospital, J Res Med Dent Sci, 2019, 7(2): 25-32.
Received: 21-Jan-2019 Accepted: 01-Mar-2019
