Research - (2021) Volume 9, Issue 8
Intrabony Defects Management Using Growth Factor Enhanced Matrix versus Platelet Rich Fibrin Utilizing Minimally Invasive Surgical Technique: A Randomized Control Study
Nora Saeed Elsayed Raslan*, Mohammed Mohammed Nassar, Omaima Helmy Afifi and Malak Yousef Mohamed Shoukheba
*Correspondence: Nora Saeed Elsayed Raslan, Department of Oral medicine, Periodontology, Oral Diagnosis and Oral Radiology, Tanta University, Egypt, Email:
Abstract
The present study aimed to assess the regenerative effect of minimally invasive surgical technique (MIST) alone or combined with growth factor enhanced matrix (GEM 21S) versus platelet rich fibrin (PRF) in the treatment of intra-bony defects clinically and radiographically. Subject and Methods: 21 intra-bony defects in fifteen systemically healthy patients with moderate to severe chronic periodontitis were randomly classified into 3 groups, 7 sites each. Group І treated by MIST alone, group ІІ treated by MIST+ethylenediamine-tetraaceticacid (EDTA) + PRF and group III treated by MIST+EDTA+GEM 21S. The clinical parameters including probing pocket depth (PPD), clinical attachment level (CAL) and bleeding on probing (BOP), were recorded at baseline, 3, 6 and 9 months’ post-surgery. Cone beam computed tomography (CBCT) was performed at baseline and 9 months’ post-surgery to evaluate bone level and bone density. Results: Group II showed the marked improvements in clinical parameters followed by group III; while group I showed the least improvements. CBCT analysis showed statistically significant improvement in bone level, area of defect (AD) and bone density (BD) for the three studied groups at 9 months as compared to the mean baseline value with no significant differences between them at 9 months’ period. However, group III showed the best improvement followed by group II and group I. Conclusion: MIST with or without regenerative materials yielded improvement clinically and radiographically. The adjunctive use of PRF or GEM 21S provided superior benefits on the outcome of MIST for the treatment of intra-bony defects.
Keywords
Chronic periodontitis, Intra-bony defects, minimally invasive surgical technique, Platelet rich fibrin, Growth factor enhanced matrix 21S, Cone beam computed tomographyIntroduction
Periodontal regenerative techniques include soft tissue grafts, bone grafts, root bio modifications, and guided tissue regeneration (GTR). The introduction of biomimetic agents, such as platelet rich plasma (PRP), platelet derived growth factors (PDGFs), bone morphogenic proteins (BMP), and other growth factors have given new promise for better outcomes in periodontal regeneration [1].
A convenient technique to obtain a high concentration of PDGFs is by preparing autologous platelet-rich protein (PRP) which is considered the first generation of platelet concentrate. A second generation of platelet concentrate is called platelet-rich fibrin (PRF) [2]. The PRF clot forms a strong natural fibrin matrix, which concentrates almost all the platelets and growth factors of the blood harvest [3]. This unique structure act as a vehicle for carrying cells, cell migration and proliferation, that are essential for tissue regeneration. Many growth factors, such as platelet derived growth factor (PDGF), transforming growth factor (TGF-β), vascular endothelial growth factor (VEGF), insulin growth factor (IGFs), and fibroblast growth factor (FGF) are released from PRF [1].
New and superior wound healing and bone regeneration technology termed growth factor enhanced matrix (GEM 21S) has recently become available for clinical use. This graft material consists of a concentrated solution of pure recombinant human platelet derived growth factor (rh- PDGF-BB), the synthetic form of the body’s key natural wound healing stimulator PDGF-BB and an Osteoconductive matrix which is beta-tricalcium phosphate (β-TCP) that is approved by Food and Drug Administration (FDA) for human application [4]. This graft material is a highly porous and resorb able matrix that provides a three-dimensional scaffold which acts as a framework for bone ingrowth, preventing the collapse of the soft tissues and promotes stabilization of the blood clot, thus facilitating bone healing [5].
The conventional periodontal surgery showed extensive tissue reflection which could result in attachment loss and lead to thermal sensitivity, food impaction and compromised esthetics [6,7]. Nowadays, a new periodontal surgical approach known as minimally invasive surgery (MIS) was proposed by Cortillini et al. [8]. They have the ability to perform a conventional surgical procedure utilizing a surgical opening that is smaller than the conventional access to achieve the same or better outcomes with less post-operative discomfort, more rapid healing, less morbidity, reduction in surgical chair time [9,10].
The background foundations for a novel surgical approach for periodontal regeneration (MIST) blended the concepts of MIS with the application of the papilla preservation techniques and the use of passive internal mattress sutures to seal the regenerating wound from the oral environment [11].
Accordingly, the present study was conducted to assess the effect of MIST combined with GEM 21S versus PRF in the treatment of the contained intra-bony defects clinically and radiographically.
Materials and Methods
Trial plan
All patients were selected from the outpatient Periodontology Clinic, Faculty of Dentistry, Tanta University. They were diagnosed with moderate to severe chronic periodontitis according to Armitage criteria [12] and stage II/III grade B according to the new classification [13]. The age ranged between 30 and 55 years. We explained our work to them and took consenting from all of the participants under supervision of the Ethics committee of Faculty of Dentistry, Tanta University and Clinical trial.gov ID: NCT04786327.
Inclusion criteria
At least one tooth with PPD and CAL loss of ≥ 5 mm associated with an intra-bony defect of ≥ 2 mm according to Cortellini et al. [8].
Exclusion criteria
• Cases with poorly controlled Diabetes Mellitus and other conditions need antibiotic prophylaxis.
• Smokers.
• Pregnant patients.
• Patients with aggressive periodontitis.
Clinical examination and Radiographical outcome variables
Clinical parameters were measured at baseline, 3, 6 and 9 months following surgical treatment including: probing pocket depth (PPD) [14], clinical attachment level (CAL) [14] and bleeding on probing (BOP) [15]. Occlusal stent was fabricated to be used for standardization as a fixed reference point and fixed angulation for accurate positioning of the probes along the study evaluation periods Figure 1. CBCT was taken to measure the total depth of the intra-bony component of the defect (INFRA) [16], area of the defect (AD) and bone density using Hounsfield unit (HU).
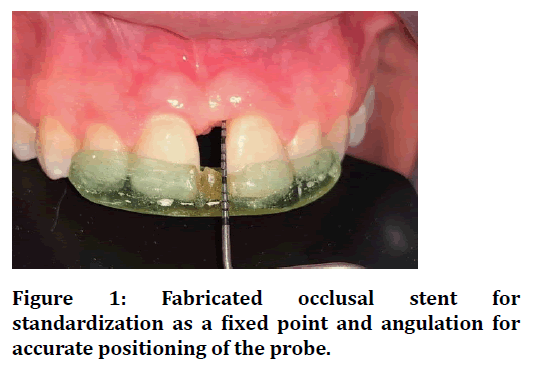
Figure 1. Fabricated occlusal stent for standardization as a fixed point and angulation for accurate positioning of the probe.
Sites grouping
Full mouth SRP was done followed by a comprehensive oral hygiene instruction. Occlusal therapy was performed as a part of periodontal therapy. Re-evaluation was conducted after one month to evaluate patient’s response to phase Ι therapy and to find if surgery is needed.
A total of 21 interproximal intra-bony defects in fifteen patients with moderate to severe chronic periodontitis (Stage II/III Grade B) were randomly classified into three groups 7 sites each by using sealed envelopes method as follow:
• Group Ι: treated by using MIST (Control group).
• Group ΙΙ: treated by using MIST with root conditioning (EDTA) and PRF (Test group).
• Group III: treated by using MIST with root conditioning (EDTA) and GEM 21S (Test group).
PRF preparation
10 ml of blood was drawn from the patient and collected in a sterile glass test tube without anti-coagulant. Immediately centrifuged using centrifuge machine at 3000 rpm for 10 minutes. The result was a fibrin clot located in the middle of a mass of a cellular plasma in the top and red cell layer in the bottom. The fibrin clot was carefully removed from the tube with tweezers then putted in sterile cup. PRF buffy coat layer was then grasped to be inserted in defects to treat group ΙΙ (Figures 2 and Figure 3).
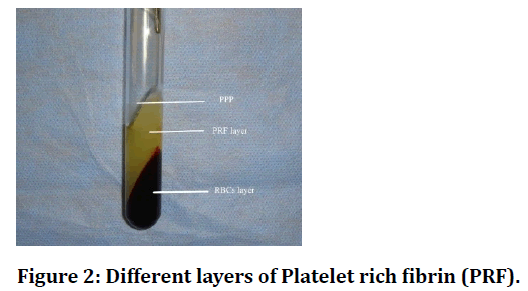
Figure 2. Different layers of Platelet rich fibrin (PRF).
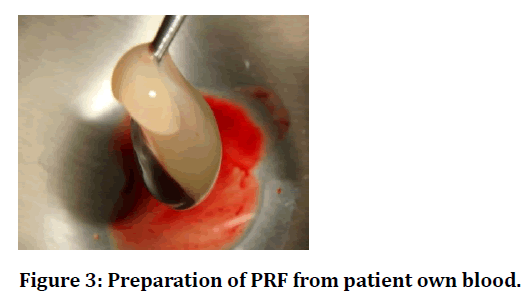
Figure 3. Preparation of PRF from patient own blood.
Surgical procedure
We followed the surgical technique explained by Cortellini et al. [17] which included small flap elevation and interdental papilla incision, transverse in wide inter dental space or diagonal in short space [18] (Figure 4A and 4 4B).
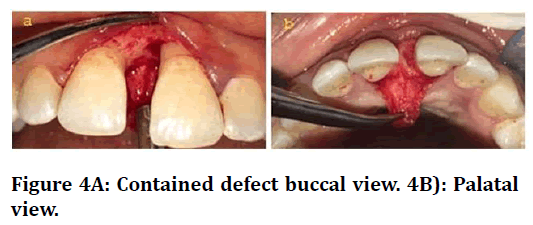
Figure 4A: Contained defect buccal view. 4B): Palatal view.
Full thickness flaps were therefore elevated with minimal mesiodistal and corono-apical. Vertical and periosteal incisions were avoided. Pocket epithelium and granulation tissue adherent to the inner surfaces of the flaps were carefully removed with micro-surgical scissors and mini-curettes to provide full access and visibility to the root surfaces (Figure 5A and 5B).
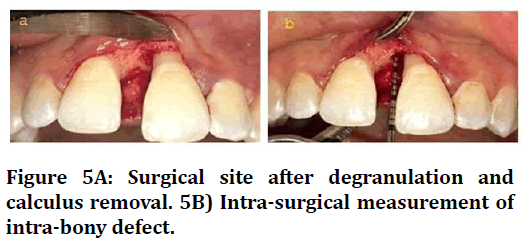
Figure 5A: Surgical site after degranulation and calculus removal. 5B) Intra-surgical measurement of intra-bony defect.
The defect was sutured in group Ι (MIST). While in group ΙΙ (PRF) and group III (GEM 21S), the exposed root surfaces were conditioned by EDTA gel for two minutes to allow to remove the smear (Figure 6A and B).
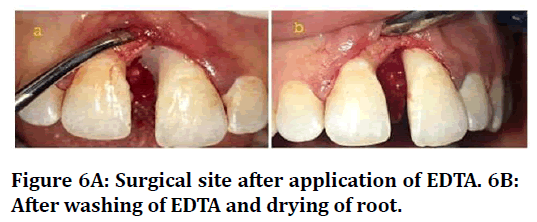
Figure 6A: Surgical site after application of EDTA. 6B: After washing of EDTA and drying of root.
After thoroughly rinsing the root surfaces with saline, PRF was directly applied to fill the defect in group II. While in group III, β-TCP granules were mixed with rh- PDGF-BB and allowed to sit for 10 minutes to permit binding of the rh-PDGF-BB protein to the β-TCP and ensure saturation before the graft was placed into the defect [19] (Figure 7A and B). Then, the buccal and lingual flaps were repositioned to their original level without any tension in the healing area and sutured using monofilament polypro line 6-0 with single modified internal mattress suture to reach primary closure of the papilla. The areas were then packed by periodontal dressing for 10 days (Figure 8).
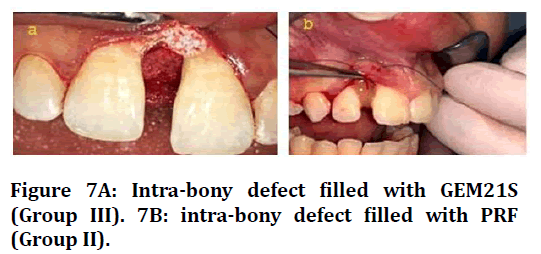
Figure 7A: Intra-bony defect filled with GEM21S (Group III). 7B: intra-bony defect filled with PRF (Group II).
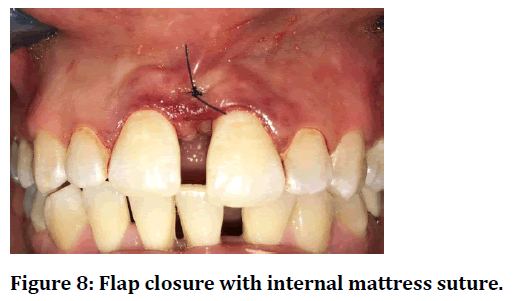
Figure 8. Flap closure with internal mattress suture.
Post-operative care
Augmentin 1gm once per day and Ibuprofen 400 mg twice daily were prescribed to the patients for one week. Subjects were ordered to wash by 0.12% Chlorhexidine (CHX) three times per day for one week. The subjects were ordered to avoid brushing, flossing or chewing on the treated area for periods of 3-4 weeks.
All subjects were recalled for professional prophylaxis, and oral hygiene instructions once a month until the final assessment 9 months’ post-surgery. They also advised to seek for consultation if they had postoperative edema, hematoma, bleeding or any other complications.
Data analysis
The collected data was organized, tabulated and statistically analysed using computer software statistical package for social science (SPSS version 20).
The Kolmogorov-Smirnov test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean, standard deviation and median. Significance of the obtained results was judged at the 5% level.
Results
At baseline the three groups showed no significant differences regarding the clinical and radiographical parameters as evidenced by their mean baseline values (P>0.05).
Clinical results
The three studied groups showed statistically significant improvement in PPD, CAL and BOP at 3, 6- and 9-months post-surgery as compared to the mean baseline value (P ≤ 0.05) (Tables 1 to Table 3).
| Time of assessment | Group I MIST (n=7) | Group II MIST+EDTA+PRF (n=7) | Group III MIST+EDTA+GEM 21S (n=7) | ANOVA | Tukey's test | |||
|---|---|---|---|---|---|---|---|---|
| F | P | P1 | P2 | P3 | ||||
| Baseline Mean ± SD | 5.29 ± 0.49 | 6.0 ± 1.41 | 5.43 ± 0.79 | 1.05 | 0.37 | 0.377 | 0.96 | 0.53 |
| 3 Months Mean ± SD | 3.57 ± 0.53 | 3.43 ± 1.40 | 2.71 ± 1.60 | 0.921 | 0.416 | 0.976 | 0.43 | 0.55 |
| PPD reduction at 3ms | 1.71 ± 0.49 | 2.57 ± 1.51 | 2.71 ± 1.11 | 2.964 | 0.227 | NS | NS | NS |
| 6 Months Mean ± SD | 3.0 ± 0.82 | 2.57 ± 0.79 | 2.43 ± 1.27 | 0.639 | 0.539 | 0.699 | 0.53 | 0.96 |
| PPD reduction at 6ms | 2.29 ± 0.49 | 3.43 ± 1.51 | 3.0 ± 0.82 | 4.047 | 0.132 | NS | NS | NS |
| 9 Months Mean ± SD | 2.71 ± 0.76 | 2.29 ± 0.49 | 2.0 ± 1.0 | 1.5 | 0.25 | 0.567 | 0.23 | 0.77 |
| PPD reduction at 9ms | 2.57 ± 0.53 | 3.71 ± 1.25 | 3.43 ± 0.79 | 6.698* | 0.035* | 0.031* | 0.06 | 1 |
| Paired t-test | P0<0.05* | P0<0.05* | P0<0.05* | |||||
| MIST: Minimally invasive surgical technique | ||||||||
| EDTA: Ethylenediamine-tetraaceticacid | ||||||||
| GEM21S: Growth factor enhanced matrix 21S | ||||||||
| PRF: Platelet rich fibrin | ||||||||
| n=Number of patients | ||||||||
| Data expressed by Mean ± Standard deviation (X ± SD) | ||||||||
| Comparison of each period to baseline using paired t-test | ||||||||
| F: ANOVA test, pairwise comparison between each 2 group was done using Post Hoc-Test (Tuky) | ||||||||
| p: p value for comparing between the three studied groups | ||||||||
| p1: p value for comparing between Group I and Group II | ||||||||
| p2: p value for comparing between Group I and Group III | ||||||||
| p3: p value for comparing between Group II and Group III | ||||||||
| *: Statistically significant at P ≤ 0.05 | ||||||||
| **: Highly significant at P ≤ 0.001 | ||||||||
| Non-significant at P > 0.05 | ||||||||
Table 1: Effect of different treatment modalities on the mean probing pocket depth (PPD) in mm at the study evaluation periods.
| Time of assessment | Group I MIST (n=7) | Group II MIST+EDTA+PRF (n=7) | Group III MIST+EDTA+GEM 21S (n=7) | Kruskal Wallis test | Dunn's for multiple comparisons test | |||
|---|---|---|---|---|---|---|---|---|
| H | P | P1 | P2 | P3 | ||||
| Baseline Mean ± SD | 5.14 ± 1.21 | 4.86 ± 1.35 | 5.43 ± 0.79 | 0.265 | 0.876 | NS | NS | NS |
| 3 Months Mean ± SD | 3.86 ± 1.35 | 2.29 ± 1.70 | 3.29 ± 1.25 | 3.697 | 0.157 | NS | NS | NS |
| CAL gain at 3ms | 1.29 ± 0.49 | 2.57 ± 1.51 | 2.14 ± 0.69 | 5.466 | 0.065 | NS | NS | NS |
| 6 Months Mean ± SD | 3.14 ± 1.35 | 1.43 ± 1.62 | 3.0 ± 1.0 | 4.686 | 0.096 | NS | NS | NS |
| CAL gain at 6ms | 2.0 ± 0.58 | 3.43 ± 1.51 | 2.43 ± 0.53 | 5.886 | 0.053 | NS | NS | NS |
| 9 Months Mean ± SD | 2.86 ± 1.21 | 1.14 ± 1.21 | 2.57 ± 0.79 | 6.295* | 0.043* | 0.019* | 0.688 | 0.052 |
| CAL gain at 9ms | 2.29 ± 0.76 | 3.71 ± 1.25 | 2.86 ± 0.69 | 7.874* | 0.020* | 0.005* | 0.116 | 0.22 |
| Paired t-test | P0<0.05* | P0<0.05* | P0<0.05* | |||||
| MIST: Minimally invasive surgical technique | ||||||||
| EDTA: Ethylenediamine-tetraaceticacid | ||||||||
| GEM21S: Growth factor enhanced matrix 21S | ||||||||
| PRF: platelet rich fibrin | ||||||||
| n=number of patients | ||||||||
| Data expressed by Mean ± Standard deviation (X ± SD) | ||||||||
| Comparison of each period to baseline using paired t-test | ||||||||
| F: ANOVA test, pairwise comparison between each 2 group was done using Post Hoc-Test (Tuky) | ||||||||
| p: p value for comparing between the three studied groups | ||||||||
| p1: p value for comparing between Group I and Group II | ||||||||
| p2: p value for comparing between Group I and Group III | ||||||||
| p3: p value for comparing between Group II and Group III | ||||||||
| *: Statistically significant at P ≤ 0.05 | ||||||||
| **: Highly significant at P ≤ 0.001 | ||||||||
| Non-significant at P>0.05 | ||||||||
Table 2: Effect of different treatment modalities on the mean clinical attachment level (CAL) in mm at the study evaluation periods.
| Time of assessment | Group I MIST (n=7) | Group II MIST+EDTA+PRF (n=7) | Group III MIST+EDTA+GEM 21S (n=7) | Chi Square | Pairwise comparison | |||
|---|---|---|---|---|---|---|---|---|
| χ2 | MCp | FEp1 | FEp2 | FEp3 | ||||
| Baseline | 7 (100.0%) | 7 (100.0%) | 7 (100.0%) | - | - | - | - | - |
| 3 Months | 2 (28.6%) | 0 (0.0%) | 2 (28.6%) | 2.486 | 0.487 | 0.462 | 1 | 0.462 |
| 6 Months | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | - | - | - | - | - |
| 9 Months | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | - | - | - | - | - |
| Paired t-test | P0<0.05* | P0<0.05* | P0<0.05* | |||||
| MIST: Minimally invasive surgical technique | ||||||||
| EDTA: Ethylenediamine-tetraaceticacid | ||||||||
| GEM21S: Growth factor enhanced matrix 21S | ||||||||
| PRF: platelet rich fibrin | ||||||||
| n=number of patients | ||||||||
| Data expressed using No (%) | ||||||||
| χ2 Chi square test MC: Mon Carlo FE: Fisher Extract | ||||||||
| pairwise comparison between each 2 groups was done using Chi square test | ||||||||
| p: p value for comparing between the three studied groups | ||||||||
| p1: p value for comparing between Group I and Group II | ||||||||
| p2: p value for comparing between Group I and Group III | ||||||||
| p3: p value for comparing between Group II and Group III | ||||||||
| *: Statistically significant at P ≤ 0.05; **: Highly significant at P ≤ 0.001; Non-significant at P > 0.05 | ||||||||
Table 3: Effect of different treatment modalities on the mean % bleeding on probing (BOP) score at the study evaluation periods.
The intergroup comparison demonstrated nonsignificant differences between the studied groups for all clinical parameters at all study evaluation periods (P>0.05) however, a statistically significant improvement in the mean PPD reduction and CAL gain were observed at 9 months (P<0.05) between group I and group II in favour to group II.
Radiographic evaluation results
There was significant reduction in the mean value of defect depth (DD) for all three groups after surgery compared to baseline at 9 months (P < 0.05) (Table 4 and Figure 9).
| Time of assessment | Group I MIST (n=7) | Group II MIST+EDTA+PRF (n=7) | Group III MIST+EDTA+GEM 21S (n=7) | Kruskal Wallis test | Dunn's for multiple comparisons test | |||
|---|---|---|---|---|---|---|---|---|
| H | p | p1 | p2 | p3 | ||||
| Baseline Mean ± SD | 2.06 ± 1.80 | 1.81 ± 1.72 | 3.48 ± 1.27 | 4.727 | 0.094 | 0.295 | 0.324 | 0.457 |
| 9 Months Mean ± SD | 1.17 ± 0.92 | 0.83 ± 0.55 | 2.38 ± 1.67 | 4.13 | 0.127 | NS | NS | NS |
| p0 | 0.018* | 0.028* | 0.018* | |||||
| Defect depth reduction Mean ± SD. | 0.89 ± 1.01 | 0.99 ± 1.24 | 1.10 ± 0.92 | 0.618 | 0.734 | NS | NS | NS |
| MIST: Minimally invasive surgical technique | ||||||||
| EDTA: Ethylenediamine-tetraaceticacid | ||||||||
| GEM21S: Growth factor enhanced matrix 21S | ||||||||
| PRF: platelet rich fibrin | ||||||||
| n=number of patients | ||||||||
| H: H for Kruskal Wallis test, pairwise comparison between each 2 groups was done using | ||||||||
| Post Hoc Test (Dunn's for multiple comparisons test) | ||||||||
| p: p value for comparing between the three studied groups | ||||||||
| p1: p value for comparing between Group I and Group II | ||||||||
| p2: p value for comparing between Group I and Group III | ||||||||
| p3: p value for comparing between Group II and Group III | ||||||||
| *: Statistically significant at P ≤ 0.05; **: Highly significant at P ≤ 0.001; Non-significant at P > 0.05 | ||||||||
Table 4: Comparison between the three studied groups according to total depth of the intra-bony component of the defect (INFRA) in mm at baseline and 9 months’ post-surgery.
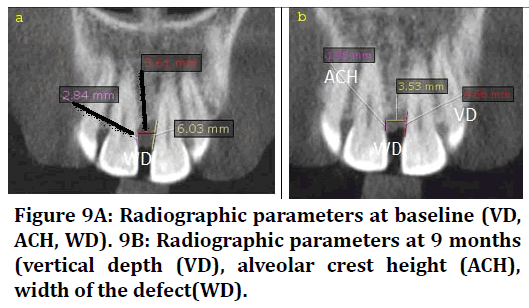
Figure 9A: Radiographic parameters at baseline (VD, ACH, WD). 9B: Radiographic parameters at 9 months (vertical depth (VD), alveolar crest height (ACH), width of the defect(WD).
There was a statistically non-significant difference between all the groups at 9 months’ post-surgery (p>0.05). However, group III showed the highest DD reduction followed by group II while group I showed the least reduction.
Regarding the defect area (DA) results showed a statistically significant reduction in the mean values of DA at 9 months as compared to their baseline values for all groups (P ≤ 0.05) (Table 5 and Figure 10).
| Time of assessment | Group I MIST (n=7) | Group II MIST+EDTA+PRF (n=7) | Group III MIST+EDTA+GEM 21S (n=7) | Kruskal Wallis | Dunn's for multiple comparisons test | ||||
|---|---|---|---|---|---|---|---|---|---|
| H | P | P1 | P2 | P3 | |||||
| Baseline Mean ± SD | 13.48 ± 3.54 | 13.27 ± 8.27 | 20.41 ± 6.61 | 5.128 | 0.077 | NS | NS | NS | |
| 9 months Mean ± SD | 10.55 ± 3.26 | 10.09 ± 4.77 | 16.24 ± 5.52 | 5.039 | 0.081 | NS | NS | NS | |
| p0 | 0.018* | 0.018* | 0.018* | ||||||
| AD fill Mean ± SD | 2.93 ± 2.46 | 3.17 ± 3.79 | 4.17 ± 1.63 | 2.293 | 0.318 | NS | NS | NS | |
| MIST: Minimally invasive surgical technique | |||||||||
| EDTA: Ethylenediamine-tetraaceticacid | |||||||||
| GEM21S: Growth factor enhanced matrix 21S | |||||||||
| PRF: platelet rich fibrin | |||||||||
| n= number of patients | |||||||||
| H: H for Kruskal Wallis test, pairwise comparison between each 2 groups was done using | |||||||||
| Post Hoc Test (Dunn's for multiple comparisons test) | |||||||||
| p: p value for comparing between the three studied groups | |||||||||
| p1: p value for comparing between Group I and Group II | |||||||||
| p2: p value for comparing between Group I and Group III | |||||||||
| p3: p value for comparing between Group II and Group III | |||||||||
| *: Statistically significant at P ≤ 0.05; **: Highly significant at P ≤ 0.001; Non-significant at P > 0.05 | |||||||||
Table 5: Comparison between the three studied groups according to defect area (DA) in mm2 at baseline and 9 months’ post-surgery.
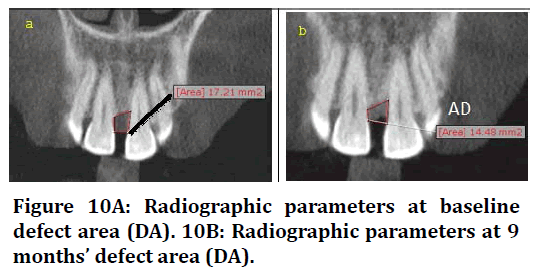
Figure 10A: Radiographic parameters at baseline defect area (DA). 10B: Radiographic parameters at 9 months’ defect area (DA).
However, there was a statistically non-significant difference between all groups at 9 months’ study interval (p>0.05) and group III showed the highest DA fill mm2 followed by group II while group I showed the least DA fill.
The radiographic results of bone density revealed that the mean values of BD have been improved for the three studied groups, this improvement was statistically significant when comparing baseline to 9 months’ postsurgery (P ≤ 0.05) (Table 6 and Figure 11).
| Time of assessment | Group I MIST (n=7) | Group II MIST+EDTA+PRF (n=7) | Group III MIST+EDTA+GEM 21 (n=7) | Kruskal Wallis | Dunn's for multiple comparisons test | |||
|---|---|---|---|---|---|---|---|---|
| H | P | P1 | P2 | P3 | ||||
| Baseline Mean ± SD | 350.9 ± 246.5 | 401.4 ± 260.5 | 756.5 ± 365.4 | 5.662 | 0.059 | NS | NS | NS |
| 9 months Mean ± SD | 509.5 ± 265.9 | 645.6 ± 234.4 | 1027.0 ± 443.7 | 5.766 | 0.056 | NS | NS | NS |
| p0 | 0.018* | 0.018* | 0.043* | |||||
| Bone fill Mean ± SD | 158.61 ± 134.37 | 244.17 ± 128.65 | 270.43 ± 252.62 | 2.16 | 0.34 | NS | NS | NS |
| MIST: Minimally invasive surgical technique | ||||||||
| EDTA: Ethylenediamine-tetraaceticacid | ||||||||
| GEM21S: Growth factor enhanced matrix 21S | ||||||||
| PRF: platelet rich fibrin | ||||||||
| n=number of patients | ||||||||
| H: H for Kruskal Wallis test, pairwise comparison between each 2 groups was done using | ||||||||
| Post Hoc Test (Dunn's for multiple comparisons test) | ||||||||
| p: p value for comparing between the three studied groups | ||||||||
| p1: p value for comparing between Group I and Group II | ||||||||
| p2: p value for comparing between Group I and Group III | ||||||||
| p3: p value for comparing between Group II and Group III | ||||||||
| *: Statistically significant at P ≤ 0.05; **: Highly significant at P ≤ 0.001; Non-significant at P > 0.05 | ||||||||
Table 6: Comparison between the three studied groups according to bone density (BD) in Hounsfield unit at baseline and 9 months’ post-surgery.
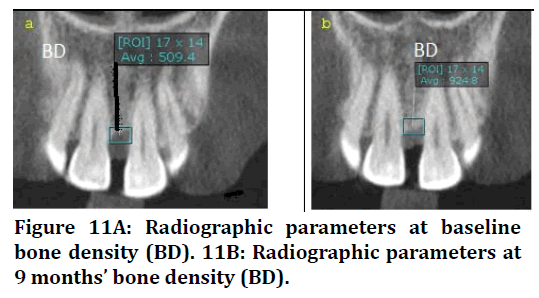
Figure 11A: Radiographic parameters at baseline bone density (BD). 11B: Radiographic parameters at 9 months’ bone density (BD).
There was a statistically non-significant difference between three groups at 9 months post-operatively (P=0.056). However, group III showed the highest bone fill followed by group II while group I showed the least bone fill.
Discussions
No adverse effects were observed in any patient during the follow up evaluation periods matching other clinical trials which have shown that neither GEM 21S nor PRF caused any allergic reactions throughout their study periods [19-21]. The results illustrated the improvement in all clinical parameters including PPD reduction, CAL gain, and decrease in BOP, with minimal recession in all groups which was maintained up to 9 months. It seems to be that MIST significantly enhanced the clinical outcomes of periodontal treatment in all groups. This was in accordance with systematic reviews conducted by Barbato et al. [22] Reedy et al. [23] meta-analysis performed by Liu et al. [24] and Perumal et al. [25]. Group II results showed the best improvement in PPD reduction and CAL gain followed by group III while group I showed the least improvement. The significant improvement in group I might be attributed to less surgical trauma, minimize flap elevation and reflection with minimal flap mobility which resulted in an extraordinary clinical healing capacity than the conventional flaps [17,22-28]. PPD and CAL reduction which was maintained till the end of the study evaluation periods regarding group II agrees with the slow sustained release of various growth factors and leukocytes cytokines present in the PRF matrix that have been proven to be released one month [29] which means that the PRF clot stimulates remodelling accelerating soft and hard tissue healing [30-33].
Concerning group III, PPD and CAL reduction was attributed to the presence of rh-PDGF-BB that possess neo-vessel formation and regenerative ability for gingival and PDL fibroblasts and cement oblasts initiating better connective tissue healing [34,35]. Additionally, it can be explained by the presence of β-TCP which considered being an effective delivery system as it entraps rh-PDGFBB within its microspores, prolonging their action. Invitro studies showed that β-TCP play a synergistic role in the mitogenic effects of PDGF on human PDL cells [36]. These results were in correspondence with several studies that showed significant improvements in PDD and CAL gain with soft tissue healing after application of rh- PDGF-BB (0.3 mg/ml) and β-TCP for treating bone deficiency [35]. On contrary, our results disagreed with a study performed by Liu et al. [24] to compare the clinical outcomes of MIST with EMD as a regenerative biomaterials and MIST alone in patients with intra-bony defects. The meta-analysis revealed no significant difference regarding PPD reduction and CAL gain between the two studied groups. This could be attributed to different regenerative material (EMD) used in this meta-analysis.
The improvement in BOP may be attributed to the advantageous effect of MIST, the effect of the biomaterials used (PRF-GEM 21S), the suturing material and technique used and the patient compliance. Patient motivation and oral hygiene reinforcement might have a role to decrease the bacterial load which reduces the inflammatory response and disease activity, provides superior conditions for regeneration to occur [8].
A new observation regarding aesthetics was the minimal gingival recession in the three studied groups at all following up evaluation periods. This prove the advantageous effect of the novel approach (MIST) alone or with other regenerative biomaterials (PRF, GEM 21S).
Interestingly, the improvement in group II when compared to group III in all evaluated clinical parameters may be attributed to higher concentration of PDGF in PRF than GEM 21S. Additionally, the sustainability of PDGF in PRF is up to 10 days, [37] while in GEM 21S, the release of rh-PDGF-BB occurred more rapidly from β-TCP [38].
The three studied groups showed statistically significant improvement at the end of the study evaluation periods. In contrast, the intergroup results showed that, there was no significant difference when comparing all groups at baseline and after 9 months. However, group III showed the best improvement in bone level parameters followed by group II and group I which were nearly the same. Moreover, group III showed the highest bone density followed by group II while group I showed the least bone fill. The improvement in bone level and bone density in group I may be attributed to that the three-wall defects facilitates filling. These observed results were in context with, Liu et al. [24].
Regarding group II, the improvement may be because of PRF entraps circulating stem cells that differentiates into osteoblast phenotype30 and due to regenerative ability of PRF autogenous growth factors [21].
The highest favourable radiographic results regarding group III, may be explained by the physical effect of β-TCP as Osteoconductive three-dimensional framework which was improved by rh-PDGF that directed migration of osteoblasts coronal and into the defect leading to osteogenesis and defect fill [5,19].
Conclusion
Our research showed that MIST with regenerative materials is a useful surgical technique for regeneration of periodontal tissue which opened a new avenue in the field of periodontal therapy. The use of GEM 21 S with mist was proved to be effective, safe and biocompatible in the treatment of periodontal osseous defects clinically and radiographically.
Limitations and Future Study
With the limitations in this study, in terms of small sample size, short term follows up evaluation periods with lack of experimental and histological evaluations, more precise results may be achieved if long-term assessment and expanded sample size were performed. Additionally, histological study on animals is needed to verify the bone and periodontal regeneration.
Acknowledgements
I wish to thank my colleagues at Periodontology Department Faculty of dentistry, Tanta University, for their help and encouragement in this study.
References
- Khiste SV, Naik Tari R. Platelet-rich fibrin as a biofuel for tissue regeneration. Biomat 2013; 2013:1-6.
- Dohan DM, Choukroun J, Diss A, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part II: Platelet-related biologic features. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101:45-50 .
- Panda S, Ramamoorthi S, Jayakumar ND, et al. Platelet rich fibrin and alloplast in the treatment of intrabony defect. J Pharm Bioallied Sci 2014; 6:127–131.
- Lynch SE, Wisner-Lynch L, Nevins M, et al. A new era in periodontal and periimplant regeneration: use of growth-factor enhanced matrices incorporating rhPDGF. Compend Contin Educ Dent 2006; 27:672-678.
- Maroo S, Murthy KRV. Treatment of periodontal intrabony defects using β-TCP alone or in combination with rhPDGF-BB: a randomized controlled clinical and radiographic study. Int J Periodont Rest Dent 2014; 34:840-847.
- Curtis JW, Jr., McLain JB, Hutchinson RA. The incidence and severity of complications and pain following periodontal surgery. J Periodontol 1985; 56:597-601.
- Harrel SK.A minimally invasive surgical approach for periodontal bone grafting. Int J Periodont Rest Dent 1998; 18:161-169.
- Dannan A. Minimally invasive periodontal therapy. J Indian Soc Periodontol 2011; 15:338-343.
- Harrel SK, Wilson TG, Rivera-Hidalgo F. A videoscope for use in minimally invasive periodontal surgery. J Clin Diagn Res 2013; 40:868-874.
- Cortellini P, Tonetti MS. Minimally invasive surgical technique and enamel matrix derivative in intra-bony defects. I: Clinical outcomes and morbidity. J Clin Periodontol 2007; 34:1082-1088.
- Cortellini P, Prato GP, Tonetti MS. The simplified papilla preservation flap. A novel surgical approach for the management of soft tissues in regenerative procedures. Intl J Periodont Rest Dent 1999; 19:589–599.
- Armitage GC. Development of a classification system for periodontal diseases and conditions. Ann Periodontol 1999; 4:1-6.
- Tonetti MS, Greenwell H, Kornman KS. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J Periodontol 2018; 89:159-172.
- Ramjford SP.( 1967). The periodontal disease index (pdi). J periodontol;38(6):602-610.
- Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J 1975; 25:229-235.
- Cortellini P, Prato GP, Tonetti MS. Periodontal regeneration of human infrabony defects. II. Re-entry procedures and bone measures. J Periodontol 1993; 64:261-268.
- Cortellini P, Tonetti MS. A minimally invasive surgical technique with an enamel matrix derivative in the regenerative treatment of intra-bony defects: A novel approach to limit morbidity. J Clin Periodontol 2007; 34:87-93 .
- Cortellini P, Prato GP, Tonetti MS. The modified papilla preservation technique. A new surgical approach for interproximal regenerative procedures. J Periodontol 1995; 66:261-266 .
- Nevins M, Giannobile WV, McGuire MK, et al. Platelet-derived growth factor stimulates bone fill and rate of attachment level gain: Results of a large multicenter randomized controlled trial. J Periodontol 2005; 76:2205-2215 .
- Maroo S, Murthy KRV. Treatment of periodontal intrabony defects using β-TCP alone or in combination with rhPDGF-BB: a randomized controlled clinical and radiographic study. Int J Periodont Rest Dent 2014; 34:840-847.
- Choukroun J, Diss A, Simonpieri A, et al. Platelet-rich fibrin (PRF): a second-generation platelet concentrate. Part IV: clinical effects on tissue healing. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101:56-60.
- Barbato L, Selvaggi F, Kalemaj Z, et al. Clinical efficacy of minimally invasive surgical (MIS) and non-surgical (MINST) treatments of periodontal intra-bony defect. A systematic review and network meta-analysis of RCT’s. Clin Oral Investig 2020; 24:1125-1135 .
- Reddy S, Abdelmagyd H, Shetty S, et al. Minimal invasive periodontal surgery: a review. J Dentomaxillofac Sci 2017; 2:81-85.
- Liu S, Hu B, Zhang Y, et al. Minimally invasive surgery combined with regenerative biomaterials in treating intra-bony defects: a meta-analysis. PLoS One 2016; 11:e0147001-14.
- Perumal MPB, Ramegowda AD, Lingaraju AJ, et al. Comparison of microsurgical and conventional open flap debridement: A randomized controlled trial. J Indian Soc Periodontol 2015; 19:406-410 .
- Ribeiro FV, Casarin RCV, Palma MAG, et al. Clinical and microbiological changes after minimally invasive therapeutic approaches in intrabony defects: a 12-month follow-up. Clin Oral Investig 2013; 17:1635-1644.
- Ribeiro FV, Casarin RC, Júnior FH, et al. The role of enamel matrix derivative protein in minimally invasive surgery in treating intrabony defects in single-rooted teeth: A randomized clinical trial. J Periodontol 2011; 82:522-532.
- Wachtel H, Schenk G, Böhm S, et al. Microsurgical access flap and enamel matrix derivative for the treatment of periodontal intrabony defects: a controlled clinical study. J Clin Periodontol 2003; 30:496-504.
- Dohan DM, Del Corso M, Charrier J. Cytotoxicity analyses of Choukroun’s platelet-rich fibrin (PRF ) on a wide range of human cells: The answer to a commercial controversy. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007; 5:587-593.
- Rastogi P, Saini H, Singhal R, et al. Periodontal regeneration in deep intrabony periodontal defect using hydroxyapatite particles with platelet rich fibrin membrane–a case report. J Oral Biol Craniofac Res 2011; 1:41-43.
- Chang Y, Wu K, Zhao J. Clinical application of platelet-rich fibrin as the sole grafting material in periodontal intrabony defects. J Dent Sci 6:181-188.
- Li A, Yang H, Zhang J, et al. Additive effectiveness of autologous platelet-rich fibrin in the treatment of intrabony defects: A PRISMA-compliant meta-analysis. Medicine 2019; 98:14759-14780.
- Shah M, Patel J, Dave D, et al. Comparative evaluation of platelet-rich fibrin with demineralized freeze-dried bone allograft in periodontal infrabony defects: A randomized controlled clinical study. J Ind Soc Periodontol 2015; 19:56-60.
- Tavelli L, Ravidà A, Barootchi S, et al. Recombinant human platelet–derived growth factor: a systematic review of clinical findings in oral regenerative procedures. JDR Clin Trans Res 2020; 20:1-13.
- McGuire MK, Scheyer ET. Comparison of recombinant human platelet-derived growth factor-BB plus beta tricalcium phosphate and a collagen membrane to subepithelial connective tissue grafting for the treatment of recession defects: A case series. Int J Periodont Rest Dent 2006; 26:127-133.
- Thakare K, Deo V. Randomized controlled clinical study of rhPDGF-BB+ β-TCP versus HA+ β-TCP for the treatment of infrabony periodontal defects: clinical and radiographic results. Int J Periodont Rest Dent 2012; 32:689-696.
- Kobayashi E, Flückiger L, Fujioka-Kobayashi M, et al. Comparative release of growth factors from PRP, PRF, and advanced-PRF. Clin oral investing 2016; 20:2353-2360.
- Young C, Ladd P, Browning C, et al. Release, biological potency, and biochemical integrity of recombinant human platelet-derived growth factor-BB (rhPDGF-BB) combined with AugmentTM Bone Graft or GEM 21S beta-tricalcium phosphate (β-TCP). J Control Release 2009; 140:250-255.
Author Info
Nora Saeed Elsayed Raslan*, Mohammed Mohammed Nassar, Omaima Helmy Afifi and Malak Yousef Mohamed Shoukheba
Department of Oral medicine, Periodontology, Oral Diagnosis and Oral Radiology, Tanta University, EgyptCitation: Nora Saeed Elsayed Raslan, Mohammed Mohammed Nassar , Omaima Helmy Afifi, Malak Yousef Mohamed Shoukheba, Intrabony Defects Management Using Growth Factor Enhanced Matrix versus Platelet Rich Fibrin Utilizing Minimally Invasive Surgical Technique: A Randomized Control Study, J Res Med Dent Sci, 2021, 9(8): 99-108
Received: 19-Jun-2021 Accepted: 09-Aug-2021
