Research - (2020) Advances in Dental Surgery
Incidence of Wound Infection after Open Reduction and Internal Fixation of Fracture of Angle of Mandible
Ramvihari Thota, Senthilnathan Periasamy* and Mahathi N
*Correspondence: Senthilnathan Periasamy, Department of Oral and Maxillofacial Surgery, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, India, Email:
Abstract
The objective of the study is to report the complication, wound infection at operative site associated with mandibular angle fracture after open reduction and internal fixation and incidence of their occurrence. A total of 86000 patient’s data between June 2019 and March 2020 were collected and analysed from patient records, out of which a total of 19 cases of mandibular angle fracture were identified and included in the present study. All these were checked for postoperative wound infection at the operative site after open reduction and internal fixation of the fracture segments. Results of this study shows that there were only 2 cases (10.5%) out of 19 which showed postoperative wound infection after open reduction and internal fixation. In this study it is observed that there was significant male predilection for mandibular angle fractures of and 10% of the cases shows postoperative infections after open reduction and internal fixation of mandible angle. Within the limitation of the study, there was significant male predilection and 10% incidence in infection post-operatively. Keywords: Maxillofacial trauma, Angle of mandible, Mandibular
Keywords
Maxillofacial trauma, Angle of mandible, Mandibular fractures, Postoperative complications, Infection
Introduction
Mandibular fractures account for most maxillofacial traumatic injuries [1-3]. A particular interest is given to mandibular fractures pertaining to the diversity of locations, severity of fractures and the availability of different treatment modalities [4]. Mandibular angle fractures are some of the most common maxillofacial injuries and are associated with the highest complications rates of all mandible fractures [5]. These fractures are frequently associated with facial lacerations, cervical spine injuries, orthopedic injuries, neurologic injury, as well as thoracic and/or abdominal injuries [6].
The mandibular angle fracture consists of fracture line that begins where the anterior border of the mandible ramus meets the body of mandible, extending inferiorly through the inferior border or posteriorly towards the gonial angle [7]. Management of such fractures is rendered difficult because of the complex biomechanics of the mandibular angle, such as the attachment of the masticatory muscles exerting their forces in different vectors, having thin cross sectional area; abrupt change in curvature, and presence of third molars [8].
Several factors may influence the perception of pain as it is a complex process. Dental pain needs to be considered more often for a possible diagnosis in the orofacial region [9- 12]. Infection of jaw fractures represents the most encountered postoperative complications, and the mandibular fractures are reported to be associated with the highest rate of infections among the maxillofacial fractures. This may be attributed to its increased cortical structure and its location in a contaminated environment [13,14].
The post-operative infection is perhaps difficult to determine whether it arises from the injury itself or from the treatment. The incidence of postoperative infection encountered with mandibular fractures varies widely among studies and ranges from 0% to 25% [15]. Such discrepancy suggests the involvement of multiple contributing variables or risk factors. This article is aimed to present and highlight the incidence of infected mandibular angle fractures post operatively after open reduction and internal fixation based on the reports from the databases.
Materials and Methods
Case records of a total of 86000 patients between June 2019 and March 2020 were collected and analysed from patient records, out of which a total of 19 cases of mandibular angle fracture were identified and included in the present study. Out of all these 18 cases were operated/treated with open reduction and internal fixation whereas one case was treated with closed reduction. All the required data were transferred to SPSS software and statistically analysed to calculate the incidence of the post-operative infection after open reduction and internal fixation.
All the necessary data were collected such as patient details, radiography, operative notes.
Inclusion criteria
Patients with angle fracture of mandible.
Patients treated with open reduction and internal fixation.
Exclusion criteria
Patients with maxillofacial trauma other than angle of mandible.
Patients treated with closed reduction.
Results and Discussion
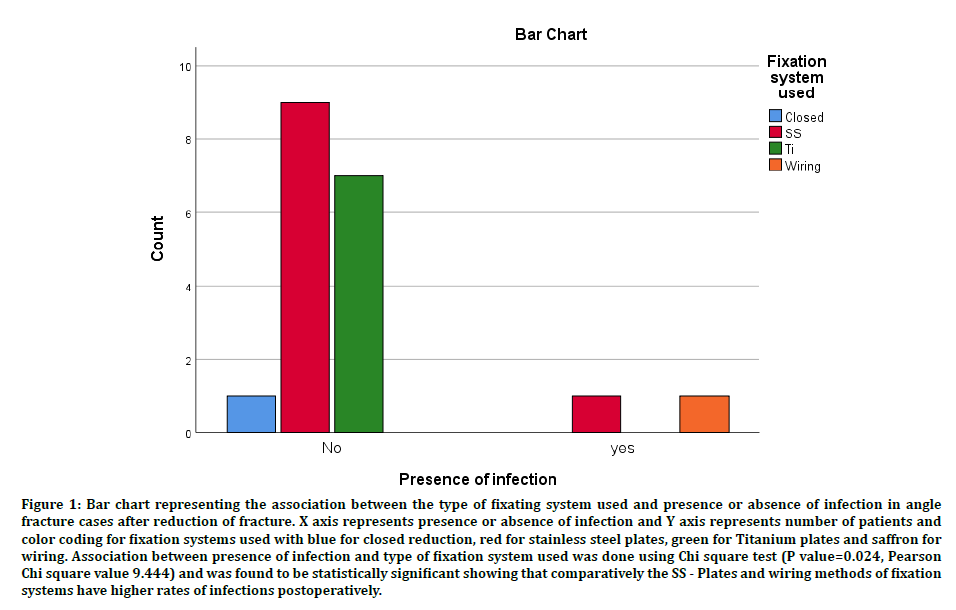
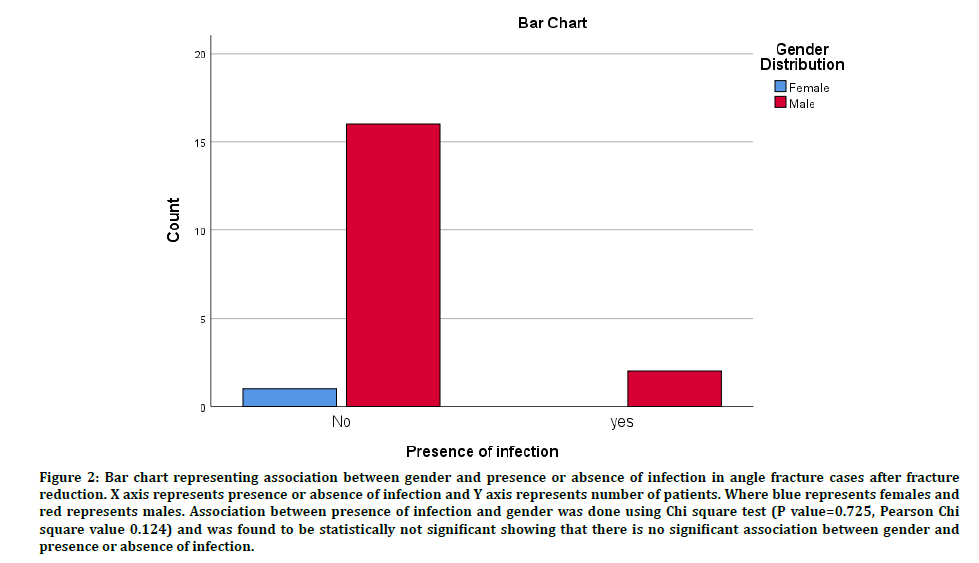
The results showed that there were 19 patients who were treated for angle fracture of mandible, out of which 18 cases were treated by open reduction and internal fixation and one by closed reduction. Results showed that the mean age at which angle fracture of mandible reported was 38± 11 years with a male predilection of 94.7%. Out of 18, 10 cases were treated with stainless steel plates, 7 cases with titanium mini plates, and one is fixed using stainless steel wiring. Postoperative infection near the operated site was seen with 10% of cases (Figures 1 and 2).
Figure 1: Bar chart representing the association between the type of fixating system used and presence or absence of infection in angle fracture cases after reduction of fracture. X axis represents presence or absence of infection and Y axis represents number of patients and color coding for fixation systems used with blue for closed reduction, red for stainless steel plates, green for Titanium plates and saffron for wiring. Association between presence of infection and type of fixation system used was done using Chi square test (P value=0.024, Pearson Chi square value 9.444) and was found to be statistically significant showing that comparatively the SS - Plates and wiring methods of fixation systems have higher rates of infections postoperatively.
Figure 2: Bar chart representing association between gender and presence or absence of infection in angle fracture cases after fracture reduction. X axis represents presence or absence of infection and Y axis represents number of patients. Where blue represents females and red represents males. Association between presence of infection and gender was done using Chi square test (P value=0.725, Pearson Chi square value 0.124) and was found to be statistically not significant showing that there is no significant association between gender and presence or absence of infection.
Dentistry comprises practices related to oral cavity. Oral diseases are a major problem among the general population and there are various procedures carried out to prevent and treat them. Oral health has a direct impact on general health patterns as it helps to talk, eat, and feel confident [16]. The postoperative infection is perhaps difficult to determine whether it arises from the injury itself or from the treatment. The incidence of postoperative infection encountered with mandibular fractures varies among studies and such discrepancy suggests the involvement of multiple contributing risk factors [17].
Risk factors
Trauma related factor
Contamination, gross displacement, and compound fractures are all factors that can contribute to the development of infections in mandibular fractures. In a study by Ellis et al. shows fractures having 2 to 4 fragments encountered with infection suggesting association between severity of trauma and infection.
Severe traumatic injuries such as gunshot wounds are often associated with increased bone fragmentation and soft tissue disruption which could be easily linked to wound contamination and subsequent infection. Tranexamic acid has been shown to be an effective method of reducing blood loss during surgical procedures [18].
Patient related factors
Virulence of organisms and host resistance are important patient related factors linked to development of infection. Aging is also suggested to be a potential risk factor for postoperative infection.
The immature immune system of children may contribute to decreased resistance to infection in pediatric trauma. Aging is usually associated with systemic diseases and both can contribute to increased risk of infection. Also,cancer cells exhibit a wide range of genetic alterations that include gene rearrangements, point mutations, and gene amplifications, leading to disturbances in molecular pathways modifying cell growth, survival, and metastasis [19,20].
Also, most patients are not aware of the complications of surgery [20,21]. Substance abuse such as smoking, alcohol and drugs has been linked to increased postoperative complication rate. The function of cellular and humoral immune system is affected by smoking and reportedly retard bone healing, adversely affect bone mineral density and even increase the risk of osteomyelitis.
Time between fracture and treatment
Early treatment after trauma is said to be associated with fewer rates of postoperative infections. Delayed treatment is said to be accompanied with increased risk of infection. And most of the human pathogens have been isolated from oral secretions [22].
Tooth in line of fracture
Although teeth in the line of fracture may interfere with reduction and/or occlusion, the greatest concern is usually directed towards the possibility of inducing infection. Even with clinically sound teeth, contamination is a possibility through the periodontal ligament, which renders all fractures in the tooth bearing area open or compound [23]. It can be recommended that the choice of investigation can depend on the size of the lesion [24].
Yet, removal of erupted or partially bony impacted teeth during treatment of mandibular fractures was to contribute to wound dehiscence even when care is taken to minimize tension during flap closure [25]. Therefore, ideal handling of teeth in fracture lines has always been a controversial issue.
Rigidity of fixation
While fracture instability is known to retard bone healing through interfering with proliferation of capillaries across the gap, the relationship between rigidity of fixation and infection remains less defined. However, inadequate stability and interfragmentary mobility is reported to be associated with greater tendency of infection [26]. Surgical alterations in the position of the bony facial skeleton will inevitably affect the soft tissues [27].
The question of postoperative infection has been long debated and represents a major complication of mandibular angle fractures. The differences in rates of infection among various studies can possibly be attributed to inherent differences in patient population being studied, variations in socioeconomic status, differences in tobacco and alcohol use or abuse and levels of nutritional status, the teeth on line of fractures can complicate management [26]. It is important for dentists to improve their knowledge to enable diagnosis and management of patients to have a more positive attitude toward these patients [28-30].
Conclusion
In the present retrospective study, it was seen that different factors were associated with increased levels of postoperative infection. This study had inherent drawbacks. Particularly use of retrospective study design. Within limitations of the study, there is significant male predilection and incidence of 10% for postoperative wound infection in angle fracture cases treated with open reduction and internal fixation. To further investigate this topic, a large postoperative clinical trial would be ideal. It is important for dentists to improve their knowledge to enable diagnosis and management of patients to have a more positive attitude toward these patients.
References
- Erol B, Tanrikulu R, Görgün B. Maxillofacial fractures. Analysis of demographic distribution and treatment in 2901patients (25-year experience). J Cranio-Maxillofac Surg 2004; 32:308–313.
- Adebayo ET, Ajike OS, Adekeye EO. Analysis of the pattern of maxillofacial fractures in Kaduna, Nigeria. Br J Oral Maxillofac Surg 2003; 41:396–400.
- Maliska MC de S, de Souza Maliska MC, Júnior SML, et al. Analysis of 185 maxillofacial fractures in the state of Santa Catarina, Brazil. Br Oral Res 2009; 23:268-274.
- Gear AJL, Apasova E, Schmitz JP, et al. Treatment modalities for mandibular angle fractures. J Oral Maxillofac Surg 2005; 63:655–663.
- Iizuka T, Lindqvist C, Hallikainen D, et al. Infection after rigid internal fixation of mandibular fractures: a clinical and radiologic study. J Oral Maxillofac Surg 1991; 49:585–593.
- Baker AB, Mackenzie W. Facial and cervical injuries. Med J Australia 1976; 1:236–237.
- Ellis E. Management of fractures through the angle of the mandible. Oral Maxillofac Surg Clin North Am 2009; 21:163–174.
- Al-Moraissi EA, Ellis E. What method for management of unilateral mandibular angle fractures has the lowest rate of postoperative complications? A systematic review and meta-analysis. J Oral Maxillofac Surg 2014; 72:2197–211.
- Kumar S. Relationship between dental anxiety and pain experience during dental extractions. J Pharma Clin Res 2017; 10:458.
- Rao TD, Santhosh Kumar MP. Analgesic efficacy of paracetamol vs ketorolac after dental extractions. Res J Pharma Technol 2018; 3375.
- Kumar S. The emerging role of botulinum toxin in the treatment of orofacial disorders: Literature update. Asian J Pharma Clin Res 2017; 10:21.
- Sweta VR, Abhinav RP, Ramesh A. Role of virtual reality in pain perception of patients following the administration of local anesthesia. Ann Maxillofac Surg 2019; 9:110–113.
- Lamphier J, Ziccardi V, Ruvo A, et al. Complications of mandibular fractures in an urban teaching center. J Oral Maxillofac Surg 2003; 61:745–749.
- Czerwinski M, Parker WL, Correa JA, et al. Effect of treatment delay on mandibular fracture infection rate. Plastic Reconstructive Surg 2008; 122:881–885.
- Marsh DR, Li G. The biology of fracture healing: optimising outcome. Br Med Bulletin 1999; 55:856–869.
- Patturaja K, Pradeep D. Awareness of basic dental procedure among general population. Res J Pharma Technol 2016; 9:1349.
- Natu SS, Pradhan H, Gupta H, et al. An epidemiological study on pattern and incidence of mandibular fractures. Plast Surg Int 2012; 8: 834364.
- Christabel A, Anantanarayanan P, Subash P, et al. Comparison of pterygomaxillary dysjunction with tuberosity separation in isolated Le Fort I osteotomies: A prospective, multi-centre, triple-blind, randomized controlled trial. Int J Oral Maxillofac Surg 2016; 45:180–185.
- Marimuthu M, Andiappan M, Wahab A, et al. Canonical Wnt pathway gene expression and their clinical correlation in oral squamous cell carcinoma. Indian J Dent Res 2018; 29:291–297.
- Patil SB, Durairaj D, Suresh Kumar G, et al. Comparison of extended nasolabial flap versus buccal fat pad graft in the surgical management of oral submucous fibrosis: A prospective pilot study. J Maxillofac Oral Surg 2017; 16:312–321.
- Jesudasan JS, Abdul Wahab PU, Muthu Sekhar MR. Effectiveness of 0.2% chlorhexidine gel and a eugenol-based paste on postoperative alveolar osteitis in patients having third molars extracted: A randomised controlled clinical trial. Br J Oral Maxillofac Surg 2015; 53:826–830.
- Kumar S, Rahman R. Knowledge, awareness, and practices regarding biomedical waste management among undergraduate dental students. Asian J Pharma Clin Res 2017; 10:341.
- Finn RA. Treatment of comminuted mandibular fractures by closed reduction. J Oral Maxillofac Surg 1996; 54:320–327.
- Packiri S, Gurunathan D, Selvarasu K. Management of paediatric oral ranula: A systematic review. J Clin Diagn Res 2017; 9:ZE06–9.
- Ulbrich N, Ettl T, Waiss W, et al. The influence of third molars in the line of mandibular angle fractures on wound and bone healing. Clin Oral Investigation 2016; 20:1297-1302.
- Ellis E. A Prospective Study of 3 treatment methods for isolated fractures of the mandibular angle. J Oral Maxillofac Surg 2010; 68: 2743–2754.
- Vijayakumar Jain S, Muthusekhar MR, Baig MF, et al. Evaluation of three-dimensional changes in pharyngeal airway following isolated lefort one osteotomy for the correction of vertical maxillary excess: A prospective study. J Maxillofac Oral Surg 2019; 18:139–146.
- Abhinav RP, Selvarasu K, Maheswari GU, et al. The patterns and etiology of maxillofacial trauma in south India. Ann Maxillofac Surg 2019; 9:114–117.
- Kumar V, Patil K, Munoli K. Knowledge, and attitude toward human immunodeficiency virus/acquired immuno deficiency syndrome among dental and medical undergraduate students. J Pahrma Bio Sci 2015; 7:666.
- Kumar S, Sneha S. Knowledge, and awareness regarding antibiotic prophylaxis for infective endocarditis among undergraduate dental students. Asian J Pharma Clin Res 2016; 9:154-159.
Author Info
Ramvihari Thota, Senthilnathan Periasamy* and Mahathi N
Department of Oral and Maxillofacial Surgery, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, IndiaCitation: Ramvihari Thota, Senthilnathan Periasamy, Mahathi N,Incidence of Wound Infection After Open Reduction and Internal Fixation of Fracture of Angle of Mandible, J Res Med Dent Sci, 2020, 8 (7): 168-172.
Received: 27-Sep-2020 Accepted: 19-Oct-2020 Published: 26-Oct-2020