Research - (2021) Volume 9, Issue 6
Incidence of Hypocalcaemia Following Total Thyroidectomy
*Correspondence: PK Baskaran, Department of General Surgery, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, India, Email:
Abstract
Incidence of hypocalcaemia following Total and Near-Total thyroidectomy Follow up of patients up to a period of 6 months. Broad overview of literature about the merits and demerits of surgical procedures used early detection and prediction of post-operative hypocalcaemia Treatment of hypocalcaemia and measures to prevent its occurrence. This study was done in 120 patients who underwent Near Total thyroid ectomy and Total thyroidectomy in the Department of General surgery, Sree Balaji Medical College and Hospital, Chennai, during the period from June 2017 to September 2019. This study which was undertaken was a prospective case series study and was started after getting due clearance from Ethical committee (EC). Patients were included in this study after getting their informed written consent. Proper post-operative monitoring and early detection by per- forming a serum calcium assay and even an intact-iPTH assay is mandatory to prevent postoperative distress to patients. Adequate and timely calcium and /or vitamin D3 supplementation is ad- vised in patients at risk for developing post-operative hypocalcaemia and for treatment of all symptomatic patients.
Keywords
Hypocalcemia, Goitre, Hypothyroidism, Oesophagus, Parathyroidism
Introduction
The thyroid gland lies in the anterior aspect of the neck and gives rise to goitres, which are often large and unsightly, sometimes obstruct the trachea and oesophagus, and may threaten life. For these reasons surgeons have long attempted to provide relief, and operations on the thyroid gland have evolved through the centuries as part and parcel of surgery. Until about 100 years ago operations were undertaken with trepidation under primitive conditions and often themselves proved fatal. Today they are routine, safe procedures with little morbidity. Goitres (derived from latin word ‘guttur’=throat) were noticed long before the thyroid itself owing to its common occurrence. Thomas Wharton, in his Adenographia in the year 1656 coined the term “thyroid gland”, meaning “shield shaped” in Greek. He also added to it by finding out that one specimen of thyroid weighed 26 grams [1-7].
In the year 1170, one of the first to attempt thyroid surgery in the treatment of goitre [8]. The first welldocumented partial thyroidectomy was undertaken in 1791 [9]. Malo was the first successful total thyroidectomy for a midline goiter, the size of an ostrich egg, with little bleeding. The most notable thyroid surgeon was Emil. They went on to perform thousands of successful operations until the latter half of the 19th century [9-10]. New problems began to spring up which made scientists discover more about the anatomy and blood supply of the thyroid gland and surrounding structures. One of Billroth's forty-eight patients reported in 1881 died from Hypocalcemictetany. The surgical anatomy and blood supply of the parathyroids were studied and described [11]. Hypocalcemia was presumed to be due to inadvertent removal of parathyroid tissue at operation [12]. Hypoparathyroidism could not be accounted for entirely by in- advertent removal of parathyroid tissue, and it was proposed that damage to the vascular pedicle of the gland was a common cause [13]. Another suggestion was that in thyrotoxic patient’s postoperative hypocalcemia was due to the hunger of osteoporotic bones for calcium, so called ‘Hungry bone syndrome’ [14]. Despite the advances that have been made in thyroid surgery with the use of latest equipment and techniques, the danger of Hypocalcemictetany is still real and every surgeon should be thorough about the anatomy of thyroid and parathyroid and be ready to deal with its complications. The great Italian Renaissance anatomist, Andreas Vesalius of Padua, gave the first description of thyroid in 1543. The thyroid gland is the big- gest gland in the neck [3]. Thomas Wharton, in his Adenographia in the year 1656 coined the term “thyroid gland”, meaning “shield shaped” in Greek. He believed that it served its purpose to the larynx by being an organ of lubrication. In 1600 BC, the Chinese had tried various remedies in the treatment of goitre. At the 3rd week of intrauterine life, the thyroid gland arises as an outpouching of the primitive foregut. Foramen caecum that is present at the base of the tongue serves as the site of origin for the gland. Medial anlage is formed by the thickening of endodermal cells present at the phar- yngeal anlage. This medial anlage thus formed descends in the neck. At the time of this descent, the anlage remains to be in continuity with the foramen caecum. This connection between the anlage and foramen caecum is through an epithelial lined tube, called the thyroglossal duct [14].
The thyroid follicular cells are formed from the epithelial cells of the anlage, which happens at around the 8th week of gestation. At the 5th week of intrauterine life, the lateral anlages fuse with the medial anlages. At the 11th week of intrauterine life, colloid formation begins. The lateral anlages give rise to parafollicular C cells, which produce calcitonin. These lateral anlages are found to be neuroectodermal in origin. The thyroid gland in an adult, is brown in colour and is bounded anteriorly by the strap muscles. The thyroid gland rests on the anterolateral aspect of the cricothyroid and trachea. The normal gland is firm and weights 20 grams. It is a bilobed structure with both lobes adjacent to the thyroid cartilage. The bilateral lobes are connected in the midline by an isthmus [15].
The isthmus is located inferior to the cricoid cartilage. In about half of the individuals, thyroglossal duct may remain as a fibrous band, called as the pyramidal lobe. In a few individuals, the right lobe may be smaller than the other (7 percent) or may even be completely absent (1.7 percent). The isthmus is absent in about 10 percent of individuals [16]. Laterally, the thyroid lobes are bound by the carotid sheath and sternocleidomastoid muscle. The strap muscles located anteriorly are sternothyroid, sternohyoid, and superior belly of omohyoid. The strap muscles are innervated by a loop of nerves from the cervical plexus, called the ansa cervicalis/ansahypoglossi. The deep cervical fascia splits into anterior and posterior division, which form a loose connecting fascia that envelops the gland.
This dire complication represents a major concern for thyroid surgeons as the consequences of chronic hypocalcaemia are often insidious and potentially severe. Permanent hypocalcaemia is a common cause of medicolegal issue after endocrine surgery.
Materials and Methods
This study was done in 120 patients who underwent Near Total thyroidectomy and Total thyroidectomy in the Department of General surgery, Sree Balaji Medical College and Hospital, Chennai, during the period from June 2017 to September 2019. This study which was undertaken was a prospective case series study and was started after getting due clearance from Ethical committee (EC). Patients were included in this study after getting their informed written consent. Inclusion criteria Patients of both sex and any age presenting with enlargement of both lobes of thyroid (includes both benign and malignant enlargement) proved by ultrasound (US) to be nodular & by laboratory investigations (Thyroid function test) to be euthyroid.
Patients excluded were those with contra-indications for surgery and general anaesthesia and those who were not in a euthyroid state. Data on patient’s demographics, operative aspects, postoperative recovery, complications (post thyroidectomy hypocalcemia) and results were collected. Patients in this study underwent a preoperative assessment to confirm the diagnosis which included, (1) Full clinical History (2) Clinical examination (3) Fine Needle Aspiration Cytology (4) Thyroid function test (TFT) (5) Ultrasound Neck (6) Indirect laryngoscopy to assess vocal cord status.
All patients included in this study were to be followed up for period of 6 months. Postoperative assessment will include the following: Immediate post-op period: in the hospital looking for numbness and other manifestations of hypocalcaemia along with serum calcium* on the second post-op day, after one month and after six months. Total Thyroidectomy is complete removal of all thyroid tissue with- out leaving behind any remnant. In our hospital, we currently use total thyroidectomy only in cases suspicious of malignancy and proven cases of Carcinoma Thyroid. The only real argument against total thyroidectomy is the potential for an increased risk of complications. However, there is good evidence to show that with increasing experiences, the use of appropriate surgical technique, and, most important, the quality training of residents, complications can be avoided. The main drawback of total thyroidectomy is the development of hypocalcemia post operatively.
Subtotal thyroidectomy was found to be a better procedure. This was so because lifelong supplementary dose would not be required. With long follow-up of these cases, however, it was observed that nodular goitre often recurs after surgery, and the recurrence rate increases with time. Another study noted a 42% recurrence rate after 30 years of follow-up in a group of 43 patients with multinodular goitre on whom subtotal thyroidectomy had been performed. Postoperative thyroxine suppression is advocated to prevent goitre recurrence. There is another issue of under diagnosed malignancy in cases of multinodular goitre and Graves’ disease Subtotal thyroidectomy in this case represents inadequate surgery.
Several studies have shown that total thyroidectomy can be performed with a morbidity rate comparable to that of less radical resections. Reeve et al. considered it a preferred option, as re-operation for recurrent goitre is associated with increased morbidity. There are several other studies that have rein- stated this. Thus, considering all the facts, total thyroidectomy represents the most logical and effective means of treating this disorder, provided the operation is performed by experienced surgeons in endocrine surgery. Currently in our department, both near-total thyroidectomy and total thyroidectomy are done, while the latter is done for cases suspicious and proven for malignancy and is usually combined with a modified radical neck dissection depending on the nodal status. The role of exciting the entire gland for treating benign disorders is gaining popular city. In near total thyroidectomy, there is two gram of remnant gland, which makes post-operative I131 scan easier. Hence, completion thyroidectomy can be planned if there is remnant tissue. Permanent or temporary hypoparathyroidism is a well-known complication of total thyroidectomy. There are two main reasons for complications. Parathyroid gland removal is the main cause followed by loss or insufficient vascular supply. Watchful surgical technique combined with spotting of the gland plays a key role. This was done by consultants or under their guidance in my study. So currently in our department we prefer to use near- total thyroid- ectomy over total thyroidectomy for treatment of benign enlargement of both lobes of thyroid.
Results
Results are mentioned in the form of Figures (Figure 1 to Figure 3).
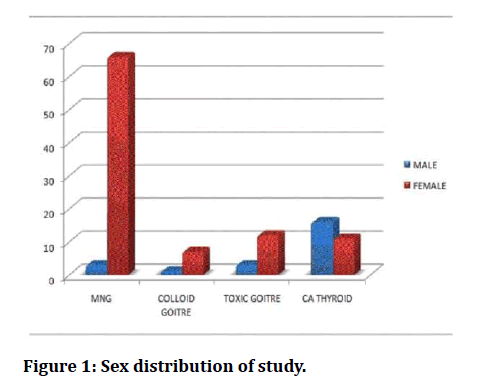
Figure 1: Sex distribution of study.
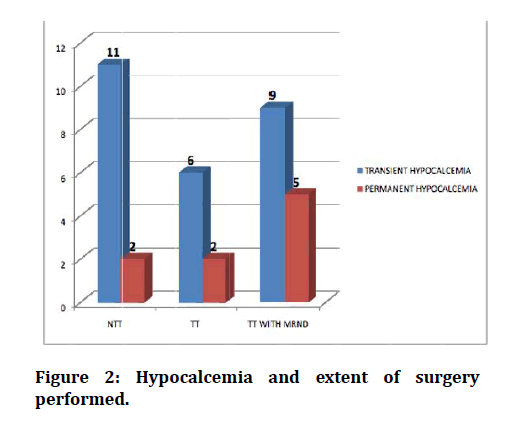
Figure 2: Hypocalcemia and extent of surgery performed.
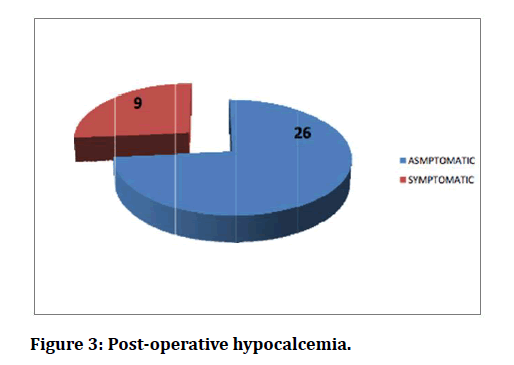
Figure 3: Post-operative hypocalcemia.
Discussion
In our study which is a prospective type 120 patients were included over a period of 2 years from June 2017 to December 2019. Regarding the sex distribution in this study, as per Table-II there were 23 males (19.2%) and 117 females (81.8%), thus we can infer those thyroid disorders are overwhelmingly more common in females. But malignancy of thyroid gland was more common in male (60%), probably male gender being in a greater risk for malignancy as per the AGES/AMES Criteria for thyroid malignancies [17]. But the benign disorders of thyroid were more common among females in age group of 20-50 yrs. (60%) as per Table-I. Malignant disorders of thyroid were more common after 50 years of age. The incidence of hypocalcemia in our study was 26 cases out of 120 operated (21.6%). Out of the 26 cases that developed hypocalcemia in our study 9 patients (34.6%) went in for permanent hypocalcemia or hypoparathyroidism which is defined as hypocalcemia persisting after 6 months of surgery, which meant, 35% of 72 patients with transient hypocalcemia went in for permanent hypoparathyroidism requiring lifelong calcium and/or vitamin D3 supplementation [18].
Regarding the distribution of hypocalcemia in our study (Table-III), there is a greater risk of developing hypocalcemia after malignant disorders of thyroid (58% of hypocalcemic patients). Also the rate of conversion to permanent hypocalcemia is 40% in malignancy of thyroid (6 out of 15 patients went in for permanent hypocalcemia after surgery),while the incidence of permanent hypocalcemia is 3% in benign thyroid disorders, out of which 2 cases developed permanent hypocalcemia , which was due to a Near-total thyroidectomy being performed for Toxic goitre and may be as a result of “Hungry bone syndrome” causing the post-operative hypocalcemia where serum calcium is sequestered in bone after the underlying pathology is removed [19-21]. This can be explained by figure-II which shows the extent of surgery performed and the occurrence of hypocalcemia which is more after more extensive procedures like Total thyroidectomy with/ without modified radical neck dissection. Though the incidence of hypocalcemia after Near Total Thyroidectomy is 11.5% (11 out of 96 operated cases), this was only a transient post- operative hypocalcemia and only two of these patients went in for a permanent hypocalcemic/hypoparathyroid state which was after surgery for toxic goitre for the reasons mentioned earlier [22].
In addition, the incidence of hypocalcemia following malignant thyroid disorders is more than 50% (62.5%; 15 out of 24 cases.) and out of which 6 patients (25%) went in for permanent hypocalcemia. Finally, as we can see from figure-III out of 26 cases of hypocalcemia recorded in our study only 9 patients (35%) were symptomatic. Among these 9 symptomatic patients we infer from Table-V that the most common symptom occurring in Hypocalcemic patients is paraesthesia’s, numbness and myalgia (5 cases) followed by FACIAL SPASMS(4 cases) and CHVOSTEKS SIGN and TROUSSEAU’S SIGN (3 cases each). The re- ported incidence of post-thyroidectomy hypocalcemia varies from 1.6% to 50% when we review literature (90, 91), estimates of the incidence of post- thyroidectomy hypoparathyroidism vary widely, ranging from 6.9% to 46% for transient and 0.4% to 33% for permanent hypoparathyroidism. In a study it is reported that 16% permanent hypocalcaemia after total thyroidectomy, an incidence, which reached to 30% when patients had 74 thyroid cancers [23-25].
In 310 patients with total thyroidectomy in the Chaudhary series, 17 patients (5.48%) had hypocalcaemia, 12 patient’s transients, and 5 had permanent hypocalcaemia. A multicenter prospective trial shows 5846 patients undergoing total thyroidectomy revealed an incidence of transient hypo- Parathyroidism of 7. 3% and permanent hypoparathyroidism of 1.5% [26,27]. When we compare the statistics of these authors with ours (transient hypocalcemia-21.6%; permanent hypocalcemia-7.5%), our rates are on the slightly higher side which probably could be due to more extensive surgery performed in our series for a greater number of malignant disorders of thyroid in our study. As regard the underlying thyroid pathology, higher incidence of hypocalcaemia with malignant (25%) and Toxic goitre (11.4%) than that in simple nodular goiter (3.6%) the high incidence of hypocalcaemia in thyrotoxicosis was noted also by Wingert et al reported an incidence of 59% for hypocalcaemia after thyroidectomy for thyrotoxicosis versus 3% incidence after thyroidectomy for simple nontoxic goitre [9]. Many theories developed to explain this high incidence of hypocalcaemia after thyroidectomy for thyrotoxicosis, Golding and Krane noted that in thyrotoxicosis there is increased bone catabolism and it has been demonstrated that the degree of thyrotoxic osteodystrophy increases proportionally with the severity of thyrotoxicosis. Michie et al postulated that the presence of osteodystrophy that excisted after surgery that was called “Hungry bone syndrome” is a possible explanation [28].
On comparison with our series our values are higher (transient hypocalcemia-62.5%; permanent hypocalcemia - 25 %%) again probably due to more frequency of concomitant radical neck dissections performed along with a total thyroidectomy in our series. According to a study skill and experience of surgeons in performing total thyroidectomies were evaluated and hypocalcaemia was observed in 6.3% of the patients, the incidence being inversely proportional to skill and experience of surgeon [29]. However, a survey by the American College of Surgeons reported an incidence of hypoparathyroidism following total thyroidectomy as 8% [30-33]. In our study the reported incidence following total thyroidectomy is 28% again due to the more extensive procedures performed (neck dissections combined with total thyroidectomy) and due to the absence of utilization auto transplantation of parathyroids in our study. Finally permanent hypoparathyroidism is slightly more frequent in cases of thyroidectomy for hyperthyroidism, thyroid carcinoma, or after previous neck surgery.
Conclusion
Postoperative hypocalcemia is the most common and sometimes the most severe and potentially debilitating complication observed after Near total thyroidectomy and Total thyroidectomy. The incidence of hypocalcemia (transient) in our study is 21% and permanent hypocalcemia requiring lifelong calcium and/or vitamin D3 supplementation is 7.5%. So proper planning and meticulous surgical technique with special emphasis in localization and preserving the vascularity of at least one parathyroid gland will go a long way in reducing this complication. We should employ newer techniques like auto-transplantation of parathyroids, use of Ultra sonic shears and enhanced bipolar diathermy which may help in bringing down the incidence of post-operative hypocalcemia.
We can avoid Transient/Permanent hypocalcemia or hyperparathyroidism by trying to look for parathyroid glands in the post-operative specimen, if detected immediate auto-transplantation of parathyroids will reduce the incidence of transient/permanent hypocalcemia following thyroidectomies. Proper postoperative monitoring and early detection by per- forming a serum calcium assay and even an intact-iPTH assay is mandatory to prevent post-operative distress to patients. Adequate and timely calcium and /or vitamin D3 supplementation is ad- vised in patients at risk for developing post-operative hypocalcemia and for treatment of all symptomatic patients. Finally, a proper follow-up schedule is mandatory in all patients undergoing Near-Total Thyroidectomy and Total Thyroidectomy.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.Conflict of Interest
The authors declare no conflict of interest.
Acknowledegements
The encouragement and support from Bharath University, Chennai, is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Welbourn RB, Friesen SR, Johnston ID, et al. The history of endocrine surgery. Greenwood Publishing Group 1990.
- Schwartz's Principles Of Surgery: Absite and board review. New York : McGraw-Hill Medical, 2011.
- Erdogan G, Erdogan MF, Emral R, et al. Iodine status and goiter prevalence in Turkey before mandatory iodization. J Endocrinol Invest 2002; 25:224-228.
- Pastor VJF, Gil VJA, De Paz Fernández FJ, et al. Agenesis of the thyroid isthmus. Eur J Anat 2006; 10:83–84.
- Skandalakis, John Elias,Colborn, Gene L. Skandalakis surgical anatomy: The embryologic and anatomic basis of modern surgery. Athens, Greece: PMP, 2004.
- Zimmermann LM, Veith I. Great ideas in the history of surgery. Baltimore: Williams & Wilkins, 1961; 98-518.
- Halsted WS. The operative story of goitre. Johns Hopkins Hosp Rep 1920; 19:71-257.
- Merke F. History and iconography of endemic goitre and cretinism. Lancaster, England: MTP Press, 1984:
- Halsted WS, Evans HM. Parathyroid glandules: Blood supply and preservation in operations. Ann Surg 1907; 46:489-506.
- Taylor S. Treatment of hyperthyroidism. In: Taylor S. Edn. Recent advances in surgery. London: Churchill, 1964; 390-405.
- Michie W, Gunn A. Thyroidectomy and the parathyroids. Br J Surg 1965; 52:503-514.
- Michie W, Duncan T, Hamer-Hodges DW, et al. Mechanism of hypocalcaemia after thyroidectomy for thyrotoxicosis. Lancet 1971; 297:508-14.
- https://www.statpearls.com/ArticleLibrary/viewarticle/36175
- https://www.elsevier.com/books/grays-anatomy/standring/978-0-7020-5230-9
- https://www.ncbi.nlm.nih.gov/books/NBK519038/
- Akerström G, Malmaeus J, Be rgstrom R. Surgical anatomy of human parathyroid glands. Surgery 1984; 95.
- Asari R, Passler C, Kaczirek K, et al. Hypoparathyroidism after total thyroidectomy: A prospective study. Archives Surg 2008; 143:132-7.
- Yamashita H, Murakami T, Noguc hi S, et al. Postoperative tetany in Graves’ disease: Important role of vitamin D metabolites. Ann Surg 1999; 229:237-245.
- Quiros RM, Pesce CE, Wilhelm SM, et al. In- traoperative parathyroid hormone leve ls in thyroid surgery are predictive of postoperative hypoparathyroi dism and need for vitamin D supplementation. Am J Surg 2005; 189:306-309.
- Lombardi CP, Raffaelli M, Princi P, et al. Early prediction of postthyroidectomy hypocalcemia by one single iPTH measurement. Surgery 2004; 136:1236-1241.
- Liu Q, Djuricin G, Prinz R. Total thyroidectomy for benign thyroid disease. Surgery 1998; 123:2
- Khadra M, Delbridge L, Re eve TS, et al. Total thyroidectomy: its role in the manage ment of thyroid disease. Aust N Z J Surg 1992; 62:91-95.
- Geerdsen JP, Frolund L. Recurrence of non-toxic goiter with and without thyroxin medication. Clin. Endocrinol 1984; 21:529.
- Rojmark J, Jarhult J. High long term recurrence rate after subtotal thyroidectomy for nodular goiter. Eur J Surg 1995; 161:725-727.
- Anderson PE, Hurley PR, Rosswick P. Conservative treatment and long term prophylactic thyroxine in the prevention of recurrence of multinodular goiter. Surg Gynecol Obstetr 1990; 171:309-14.
- Bergfeidt G, Risholm L. Postoperative thyroid hormone therapy in non-toxic goiter. Acta Chir Scand 1963; 126:531.
- Persson P, Johansson H, Westermark K, et al. Nodular goiter: Is thyroid medication of any value? World J Surg 1982; 6:391.
- Gardiner KR, Russel CFJ. Thyroidectomy for large multinodular colloid goiter. J Res Coll Surg Edinb 1995; 40:367.
- Reeve TS, Delbridge L, Cohen A. et al. Total thyroid- ectomy: the preferred option for multinodular goiter. Ann Surg 1987; 206:782.
- Perzik SL. The place of tota l thyroidectomy in the management of 909 patients with thyroid disease. Am J Surg 1976; 132:480.
- Wingert DJ, Friesen SR, Iliopoulo s JI, et al. Post-thyroidectomy hypocalcaemia. Incidence and risk factors. Am J Surg 1986; 152:606-610.
- Perzik SL. The place of tota l thyroidectomy in the management of 909 patients with thyroid disease. Am J Surg 1976; 132:480.
- Wingert DJ, Friesen SR, Iliopoulo s JI, et al. Post-thyroidectomy hypocalcaemia. Incidence and risk factors. Am J Surg 1986; 152:606-610.
