Research Article - (2022) Volume 10, Issue 10
Histopathological Study of Endometrium among Pre and Post-Menopausal Women with Abnormal Uterine Bleeding (AUB)
Geethalaxmi, Faisal and Jayalakshmi G*
*Correspondence: Dr. Jayalakshmi G, Department of Pathology, Sri Lakshmi Narayana Institute of Medical Sciences Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email:
Abstract
Carcinosarcoma shares risk factors with endometrial carcinoma, but the influence of these factors is weaker. Some carcinosarcomas have also been known to possess estrogen and progesterone receptors. The most important entities this prospective study was conducted in the Department of Pathology, Sri Lakshmi Narayana Institute of Medical Sciences, Puduchery. The present study aimed to analyse and to determine the causes of (Abnormal Uterine Bleeding) AUB among pre and post-menopausal women. 83 cases were pre-menopausal and 22 cases were post-menopausal bleeding. Patients were evaluated according to the age, clinical features and endometrial histopathology. The age group of 40 to 45 years old to be with higher AUB incidence.
Keywords
Simple hyperplasia without atypia, Postmenopausal uterine bleeding, Secretory disorders, Abnormal uterine bleeding
Introduction
The innermost layer, the myometrium, is made up of smooth muscles. The thickened functional zone in adenomyosis is termed as the functional zone. The loose connective tissue that surrounds the uterus is known as perimetrium. The uterine artery branches that emerge from the anterior trunk of the internal iliac artery provide the main blood supply to the endometrium. It reaches the uterus at the level of the internal OS, where it turns upwards at a right angle and follows a spiral route along the uterus's lateral edge. Branches that run transversely pass into the myometrium during the vertical portion of their path. These are accurate arteries, which give rise to a sequence of right-angled radial arteries. Spiral and straight at the end [1].
Uterine carcinosarcomas, also known as malignant mixed mullerian tumours, are aggressive neoplasms made up of epithelial and mesenchymal parts, both of which are malignant histologically. It's possible that the sarcomatous component is made up of homologous or heterologous tissue. Carcinosarcoma accounts for 2-5% of all malignancies of the uterine corpus. It is most common in post-menopausal women (median age 66 years) but has also been reported in younger women and children. Abnormal vaginal bleeding is the most common symptom [2].
Carcinosarcoma shares risk factors with endometrial carcinoma, but the influence of these factors is weaker. Some carcinosarcomas have also been known to possess estrogen and progesterone receptors. Mullerian adenosarcoma with stromal overgrowth, endometrioid adenocarcinoma with conspicuous spindle cells, carcinomas with undifferentiated component, and monophasic pleomorphic tumours are the most important entities in the differential diagnosis of carcinosarcoma. The purpose of this study was to investigate and determine the aetiology of AUB in premenopausal and postmenopausal women [3].
Materials and Methods
Between August 2011 and July 2013, the current prospective study was done in the Department of Pathology at Bharath Institute of Higher Education and Research in Chennai. During this study period, 105 specimens received from Obstetrics and Gynaecology department of SBMCH, Chennai, from patients with pre and post-menopausal abnormal uterine bleeding. Specimens from patients with AUB among pre and postmenopausal women, who underwent hysterectomy,endometrial biopsy or dilatation and curettage, were included. Patients with non-endometrial and nongynecological causes of pre and post-menopausal bleeding Hysterectomy specimens and endometrial biopsies from patients without complaints of pre and postmenopausal bleeding were excluded. The specimen was analysed using histoimmuno chemical methods [4].
Results
The following observations were made with regards to, (Table 1)
| Endometrial Lesions | No: of Pre-menopausal cases | % | No: of Post-menopausal cases | % | Total no of Cases | % |
|---|---|---|---|---|---|---|
| Polyp | 24 | 28.92 | 8 | 36.36 | 32 | 30.48 |
| Simple Hyperplasia | 13 | 15.67 | 1 | 4.55 | 14 | 13.33 |
| Simple Hyperplasia with atypia | 3 | 3.61 | 0 | 0 | 3 | 2.85 |
| Complex Hyperplasia | 13 | 15.67 | 1 | 4.55 | 14 | 13.33 |
| Complex Hyperplasia with atypia | 9 | 10.84 | 5 | 22.73 | 14 | 13.33 |
| Endometritis | 6 | 7.23 | 0 | 0 | 6 | 5.71 |
| Secretory Endometrium | 6 | 7.23 | 0 | 0 | 6 | 5.71 |
| Proliferative Endometrium | 6 | 7.23 | 0 | 0 | 6 | 5.71 |
| Atrophic endometrium | 2 | 2.41 | 4 | 18.18 | 6 | 5.71 |
| Squamous Metaplasia | 1 | 1.2 | 0 | 0 | 1 | 0.95 |
| Adenocarcinoma | 0 | 0 | 3 | 13.64 | 3 | 2.86 |
| Total | 83 | 100% | 22 | 100% | 105 | 100% |
Table 1: Percentage of endometrial lesions in relation to pre and post-menopausal women.
Among the endometrial causes of pre and postmenopausal bleeding, polyp was the commonest finding, constitute 30.48% of cases, followed by cases of simple hyperplasia, complex hyperplasia and complex hyperplasia with atypia constitutes 13.33% each. Secretory endometrium, Proliferative endometrium and Atrophic endometrium-evident cause not found (Table 2) [5].
| Endometrial lesions | Age (Years) and Percentage details | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 36-40 | % | 41-45 | % | 46-50 | % | 51-55 | % | >55 | % | |
| Polyp | 2 | 16.67 | 8 | 28.57. | 14 | 32.56 | 5 | 38.46 | 3 | 33.3 |
| Simple Hyperplasia | 3 | 25 | 4 | 14.29 | 6 | 13.95 | 1 | 7.69 | 0 | 0 |
| Simple Hyperplasia with atypia | 1 | 8.33 | 1 | 3.57 | 1 | 2.33 | 0 | 0 | 0 | 0 |
| Complex Hyperplasia | 0 | 0 | 4 | 14.29 | 9 | 20.93 | 0 | 0 | 1 | 11.11 |
| Complex Hyperplasia with atypia | 0 | 0 | 3 | 10.71 | 6 | 13.95 | 4 | 30.77 | 1 | 11.11 |
| Endometritis | 1 | 8.33 | 2 | 7.14 | 3 | 6.98 | 0 | 0 | 0 | 0 |
| Secretory Endometrium | 1 | 8.33 | 2 | 7.14. | 3 | 6.98 | 0 | 0 | 0 | 0 |
| Proliferative Endometrium | 4 | 33.33 | 2 | 7.14 | 0 | 0 | 0 | 0 | 0 | 0 |
| Atrophic endometrium | 0 | 0 | 1 | 3.57 | 1 | 2.33 | 0 | 0 | 4 | 44.44 |
| Squamous Metaplasia | 0 | 0 | 1 | 3.57 | 0 | 0 | 0 | 0 | 0 | 0 |
| Adenocarcinoma | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 23.08 | 0 | 0 |
| Total | 12 | 100% | 28 | 100% | 43 | 100% | 13 | 100% | 9 | 100% |
Table 2: Endometrial lesions in pre-and postmenopausal women are distributed by age.
Percentage distribution of endometrial lesions in different age groups
The most common endometrial lesions observed in the age group (Figure 1) between 36 to 40 years were proliferative endometrium in 4 cases (33.33%) and simple hyperplasia in 3 cases (25%). In the age range between 41 and 45 years (Figure 2), the most prevalent endometrial lesions were polyp in 8 instances (28.57%), followed by simple and complex hyperplasia in similar numbers of cases (14.29%). One case (3.57%) of squamous metaplasia was noted in the age group between 4l-45 years. In the age range 46 to 50 years, the most prevalent lesions were 14 cases (32.56%) of polyp and 9 instances (20.93%) of complicated hyperplasia (Figure 3). Similarly, polyps were prevalent in the 51-55 year old age group, with 5 cases (38.46%) and 4 cases (30.77%) of complicated hyperplasia with atypia (Figure 4). Adenocarcinoma was diagnosed in 3 cases (23.08%). All the 3 cases were seen in the age group above 50 Years (Figure 5). The age group above 55 years has the highest frequency of atrophic endometrium. In other words, 4 out of 9 cases accounted for 44.44% of the total (Table 3 and Figure 6)[6-10].
| Clinical Features | No: of Pre- menopausal Cases | % | No: of Post-menopausal Cases | % |
|---|---|---|---|---|
| Menorrhagia, Dysmenorrhoea | 29 | 34.94 | 4 | 18.18 |
| Menorrhagia, Dysmenorrhoea, Irregular cycles | 17 | 20.48 | 3 | 13.64 |
| Dysmenorrhoea, Irregular cycles, Polymenorrhagia | 18 | 21.69 | 5 | 22.73 |
| Dysmenorrhoea, Polymenorrhagia | 19 | 22.89 | 10 | 45.45 |
| Total | 83 | 100 | 22 | 100 |
Table 3: Clinical features of endometrial lesions in pre and post-menopausal women.
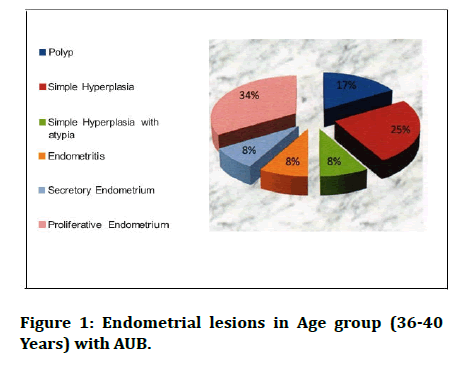
Figure 1: Endometrial lesions in Age group (36-40 Years) with AUB.
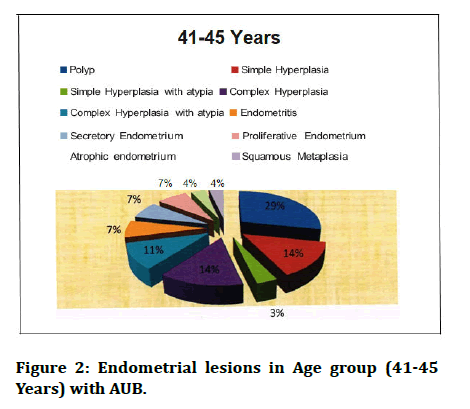
Figure 2: Endometrial lesions in Age group (41-45 Years) with AUB.
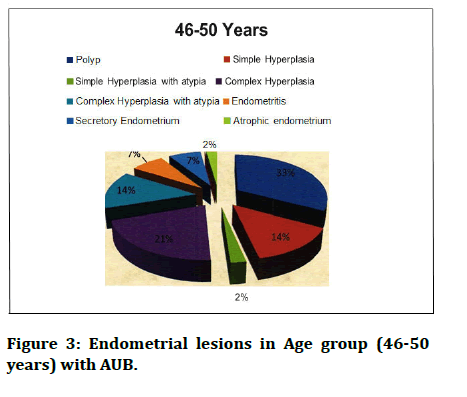
Figure 3: Endometrial lesions in Age group (46-50 years) with AUB.
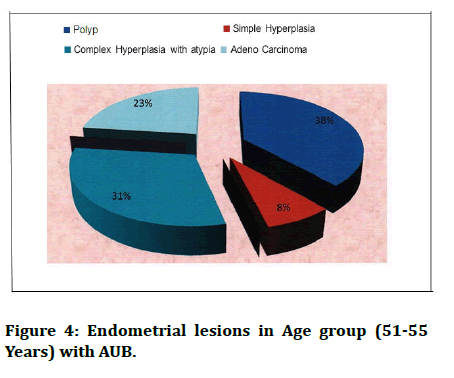
Figure 4: Endometrial lesions in Age group (51-55 Years) with AUB.
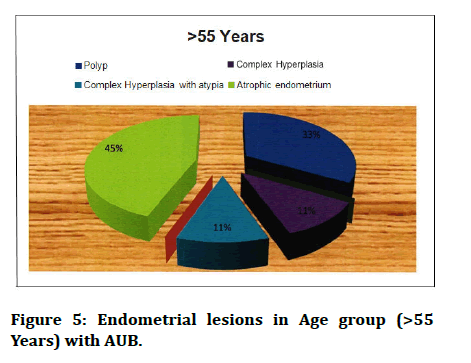
Figure 5: Endometrial lesions in Age group (>55 Years) with AUB.
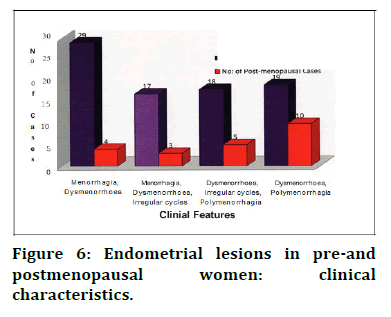
Figure 6: Endometrial lesions in pre-and postmenopausal women: clinical characteristics.
Clinical features of various endometrial lesions in pre and post-menopausal women were studied. The most common clinical features (bleeding patterns) in premenopausal women were menorrhagia and dysmenorrhoea (34.94%), followed by polymenorrhagia and dysmenorrhoea (45.45%) in post-menopausal women (Table 4 and Figure 7).
| Microscopic Features | No: of pre- menopausal cases |
% | No: of post- menopausal cases |
% |
|---|---|---|---|---|
| Atrophic Glands | 0 | 0 | 1 | 4.54 |
| Cystic Dilation | 18 | 21.69 | 7 | 31.82 |
| Crowding of Glands | 8 | 9.64. | 1 | 4.55 |
| Hyaline Degeneration | 2 | 2.41 | 2 | 9.09 |
| Hyaline Degeneration & | 5 | 6.02 | 3 | 13.64 |
| Calcification | ||||
| Proliferative Phase | 22 | 26.51 | 6 | 27.27 |
| Secretory Phase | 28 | 33.73 | 2 | 9.09 |
| Total | 83 | 100 | 22 | 100 |
Table 4: Microscopic features of endometrial glands in pre and post-menopausal women.
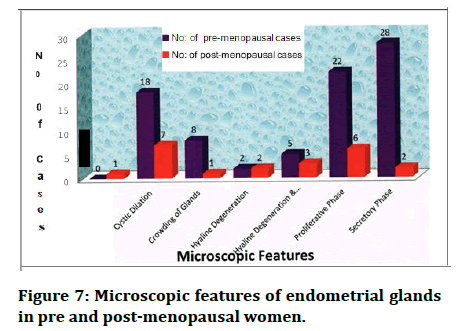
Figure 7: Microscopic features of endometrial glands in pre and post-menopausal women.
Microscopic features of endometrial glands in pre and post-menopausal women were studied. The most prevalent pattern of endometrial glands in premenopausal women were secretory glands (33.73%) and proliferative glands (26.51%) followed by cystic dilation of glands (31.82%) m post-menopausal women (Figure 8) [10-12].
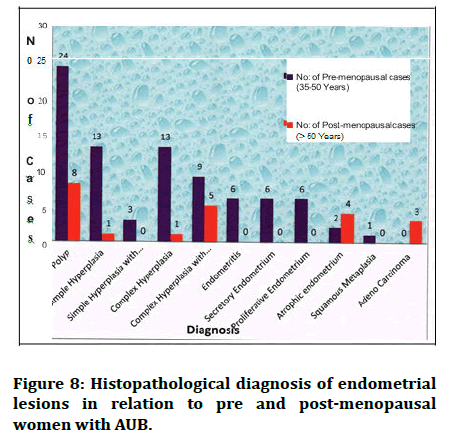
Figure 8: Histopathological diagnosis of endometrial lesions in relation to pre and post-menopausal women with AUB.
Discussion
Endometrial lesions often present as a diagnostic challenge to pathologists due to venous modes of presentation and simulating histologic picture produced by several causes. Microscopic examination of the endometrial specimen is required for accurate identification and treatment of benign and malignant diseases. During a 24 months period, women who had abnormal uterine bleeding due to an endometrial aetiology were included in this study. Out of 105 cases studied, 83 cases were premenopausal and 22 cases were post-menopausal bleeding. The common endometrial lesions in pre-menopausal age group in the present study were polyp 28.92%, followed by 15.67% of simple and complex hyperplasia each. Present study correlated with the study done by Saraswathi, et al. where polyp was 28.4%. But cases presented as simple hyperplasia and complex hyperplasia was less in the present study as compared to other studies. The common endometrial lesion in post-menopausal age group in the present study was polyp 36.36%. This was similar to the study done by Densie, et al. so accounted for 35.7%. The commonest bleeding patterns in pre-menopausal women in the present study were menorrhagia and dysmenorrhea accounted for 34.94% of cases, followed by 22.89% cases of polymenorrhagia and dysmenorrhoea. Present study correlated with the study done by Mehrotra, et al. where menorrhagia and dysmenorrhoea was 32%. But cases presented as polymenorrhagia and dysmenorrhoea was less in the present study as compared to other studies. The commonest bleeding patterns in post-menopausal women in the present study were polymenorrhagia and dysmenorrhoea accounted for 45.45% of cases. Present study correlated with the study done by Tahira rasheed, et al. where polymenorrhagia and dysmenorrhoea was 43.3%.
Conclusion
Abnormal uterine bleeding can occur due to organic causes in the uterus or due to functional disturbances related to ovulation. The histopathological findings of endometrial biopsy is important in the evaluation of these patients with abnormal uterine bleeding to find out any organic pathology, because it is crucial for appropriate therapy, particularly in patients with postmenopausal bleeding and metrorrhagia. Even in cases of malignant tumours, early diagnosis with endometrial sampling and prompt treatment reduces morbidity and mortality of the patients.
Acknowledgments
The encouragement and support from Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India is gratefully acknowledged for providing the laboratory facilities to carry out the research work.
References
- Awwad JT, Toth TL, Schiff I. Abnormal uterine bleeding in the perimenopause. Int I Fertil Menopausal Stud 1993; 38:261-269.
- Todorovic N, Djordjevic V, Antonijevic S. Results of histopathologic findings of endometrial changes in metrorrhagia. Srp Arh Celok Lek 2002; 130:386-388.
- Kumar P, Malhotra N. Jeffcoat’s principles of gynecology. 7th edition, Jaypee Brothers Medical Publishers (P) Ltd. 2008; 862.
- Adams Hil, lard PJ. Benign diseases of the female reproductive tract. Novak’s Gynecology 14th ed. Lippincott Williams and Wilkins. 2007; 2:490-491.
- Sternberg SS, Mills SE, Carter D. Sternberg’s Diagnostic Surgical Pathology. 4th edition Philadelphia: Lipp- incott Williams. 2004; 3:24-53.
- Hellweg GD. The Histopathology of the Endometrium. Springer Link 1981; 89–256.
- Cooke ID. Endocrine changes associated with menopause and post-menopausal years. The Management of Menopause and Post-menopausal years 1976; 49-62.
- Sherman BM. Endocrinologic and menstrual alterations. Menopause: Physiol Pharmacol 1987; 41-51.
- Bentley RC, Mutter GL, Robboy SJ. Robboy’s Pathology of the female reproductive tract. Churchill Livings tone Elsevier. 2009; 314.
- Lums den M, Norman F. Menstruation and menstrual abnormality. Shaw Gynaecology 2nd edition, Churchil Livingstone Newyork. 1997; 421-437.
- Mutter GL, Nucci, MR, Robboy SJ. Endometritis, metaplasias, polyps, and miscellaneous changes. In: Robboy's Pathology of the Female Reproductie Tract, 2nd ed., Robboy SJ, Mutter GL, Prat J, et al. (Eds), Churchill Livingston Elsevier, Oxford 2009. p.343.
- Kempson RL. The Uterine Corpus. Sternberg’s Diagnostic Surgical Pathology. 4th ed, Philadelphia: Lippincott Williams and Wilkins. 2004; 3:2491.
Author Info
Geethalaxmi, Faisal and Jayalakshmi G*
Department of Pathology, Sri Lakshmi Narayana Institute of Medical Sciences Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Geethalaxmi, Faisal, Jayalakshmi G, Histopathological Study of Endometrium among Pre and Post-Menopausal Women with Abnormal Uterine Bleeding (AUB), J Res Med Dent Sci, 2022, 10 (10): 067-072.
Received: 08-Aug-2022, Manuscript No. JRMDS-22-66692; , Pre QC No. JRMDS-22-66692(PQ); Editor assigned: 10-Aug-2022, Pre QC No. JRMDS-22-66692(PQ); Reviewed: 23-Aug-2022, QC No. JRMDS-22-66692; Revised: 10-Oct-2022, Manuscript No. JRMDS-22-66692(R); Published: 20-Oct-2022
