Review Article - (2022) Volume 10, Issue 12
Guided Tissue Regeneration Membrane
Shivani Thakare*, Bhairavi Kale, Khushboo Durge and Pavan Bajaj
*Correspondence: Dr. Shivani Thakare, Department of Periodontics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi (Meghe), Wardha, Maharashtra, India, Email:
Abstract
For repairing periodontal tissues lost as a result of periodontal disease, the biological principle of "Guided tissue Regeneration" (GTR) was created. This theory was based on the idea that by using a membrane barrier, non-desirable forms of tissue cells can be kept from migrating into a wound while also giving precedence to those cells that can regenerate the desired type of tissue when repopulating the wound. This idea could be used in a variety of surgical procedures aiming at regenerating missing tissues. Osseous surgery, which focuses on bone regeneration, is one such specialty. Biocompatibility, cell occlusiveness, space making tissue integration, and clinical manageability regeneration (GTR) to cure bone abnormalities are all characteristics that must be met by barrier membranes for guided tissue (GTR) to cure bone abnormalities.
https://www.mobafire.com/profile/syachtcharter12-1120796?profilepage http://www.effecthub.com/user/3726164 http://hawkee.com/profile/4964828/ https://www.youmagine.com/syachtcharter12/designs https://www.myminifactory.com/users/Syachtcharter12 http://qooh.me/Syachtcharter12 https://linktr.ee/syachtcharter12 https://pubhtml5.com/homepage/akozv/ https://telegra.ph/Syachtcharter12-09-08 https://www.diggerslist.com/64fad99c0c7d7/about https://allmyfaves.com/Syachtcharter12 https://www.metal-archives.com/users/Syachtcharter12 https://www.catchafire.org/profiles/2492674/ https://www.fimfiction.net/user/634620/Syachtcharter12 https://www.hebergementweb.org/members/syachtcharter12.550840/ https://www.sqlservercentral.com/forums/user/syachtcharter12 https://www.twitch.tv/syachtcharter12/about https://www.roleplaygateway.com/member/Syachtcharter12/ https://www.provenexpert.com/syachtcharter12/ https://www.intensedebate.com/people/Syachtcharter12 https://www.indiegogo.com/individuals/35177157 https://visual.ly/users/syachtcharter/portfolio https://slides.com/syachtcharter12 https://letterboxd.com/Syachtcharter12/ https://micro.blog/Syachtcharter12 https://fliphtml5.com/dashboard/public-profile/mevsh https://community.windy.com/user/syachtcharter12 https://speakerdeck.com/syachtcharter12 https://trello.com/u/syachtcharter https://www.redbubble.com/people/Syachtcharter12/shop?asc=u https://myanimelist.net/profile/Syachtcharter12 https://3dwarehouse.sketchup.com/user/c29939b1-698b-41d5-a0a7-d77194c632b2/Syachtcharter12-S https://www.wattpad.com/user/Syachtcharter12 https://www.goodreads.com/user/show/169712876-syachtcharter12 https://en.gravatar.com/syachtcharter https://tr.pinterest.com/syachtcharter/ https://www.mapleprimes.com/users/Syachtcharter12 https://medium.com/@syachtcharter https://www.ted.com/profiles/44978926 https://www.infragistics.com/community/members/9ad69333f0de5c2dd3f85ce08768d3716996ee65 https://www.metooo.io/u/64fb153634cbec3769e88e54 https://app.roll20.net/users/12391035/syachtcharter12-s https://list.ly/syachtcharter/activity https://giphy.com/channel/Syachtcharter12 https://www.tumblr.com/blog/syachtcharter12 https://dzone.com/users/4989513/syachtcharter12.html https://www.creativelive.com/student/syachtcharter12-v?via=accounts-freeform_2 https://gab.com/Syachtcharter12 https://sketchfab.com/Syachtcharter12 https://www.flickr.com/people/199128394@N06/ https://hub.docker.com/u/syachtcharter12 https://profiles.wordpress.org/syachtcharter12/ https://wefunder.com/syachtcharter12 https://seedandspark.com/user/syachtcharter12-01h9tgpxyps2f2vkaemrh75t6b https://calis.delfi.lv/blogs/posts/209937-httpssyachtchartercom/lietotajs/313437-syachtcharter12/ https://os.mbed.com/users/syachtcharter12/ https://notionpress.com/author/922959# https://my.desktopnexus.com/Syachtcharter12 https://guides.co/a/syachtcharter12-syachtcharter12/ https://www.bahamaslocal.com/userprofile/1/240620/Syachtcharter12.html http://molbiol.ru/forums/index.php?showuser=1297205 https://www.credly.com/users/syachtcharter12-syachtcharter12/badges https://www.facer.io/user/0uges7xB2n https://ko-fi.com/syachtcharter12#paypalModal https://mastodon.online/@Syachtcharter12 https://devpost.com/linayachting?ref_content=user-portfolio&ref_feature=portfolio&ref_medium=global-nav http://onlineboxing.net/jforum/user/editDone/250555.page https://www.mobafire.com/profile/bodrumteknekirala12-1121091?profilepage http://www.effecthub.com/user/3726536 http://hawkee.com/profile/4981334/ https://www.youmagine.com/bodrumteknekirala12/designs https://www.myminifactory.com/users/Bodrumteknekirala12 http://qooh.me/Bodrumtekne https://linktr.ee/bodrumteknekirala12 https://pubhtml5.com/homepage/ymrxp/ https://telegra.ph/Bodrumteknekirala12-09-11 https://www.diggerslist.com/64fed8ad8a215/about https://allmyfaves.com/Bodrumteknekirala12 https://www.metal-archives.com/users/Bodrumteknekirala12 https://www.catchafire.org/profiles/2495596/ https://www.fimfiction.net/user/635464/Bodrumteknekirala12 https://www.hebergementweb.org/members/bodrumteknekirala12.551744/ https://www.sqlservercentral.com/forums/user/bodrumteknekirala12 https://www.twitch.tv/bodrumteknekirala12/about https://www.roleplaygateway.com/member/Bodrumteknekirala12/ https://app.provenexpert.com/Bodrumteknekirala12 https://www.intensedebate.com/people/Bodrumtekne https://www.indiegogo.com/individuals/35201624 https://visual.ly/users/bodrumteknekirala/portfolio https://slides.com/bodrumteknekirala12 https://letterboxd.com/Bodrumteknekira/ https://micro.blog/Bodrumteknekirala12 https://fliphtml5.com/dashboard/public-profile/oqzeg https://community.windy.com/user/bodrumtekne https://speakerdeck.com/bodrumteknekirala12 https://trello.com/u/bodrumteknekirala https://myanimelist.net/profile/Bodrumtekne https://3dwarehouse.sketchup.com/user/841cd75b-72f4-4e78-b87c-6195cbbcc4bd/Bodrumteknekirala12-B https://www.wattpad.com/user/Bodrumteknekirala12 https://www.goodreads.com/user/show/169798357-bodrumteknekirala12 https://en.gravatar.com/bodrumteknekirala https://tr.pinterest.com/bodrumteknekirala/ https://www.mapleprimes.com/users/Bodrumteknekirala12 https://medium.com/@bodrumteknekirala https://www.ted.com/profiles/45004353 https://www.infragistics.com/community/members/c0a255b30589a84ab15f004bb52f9202f9059086?_ga=2.236965953.1172362923.1694431247-2032935766.1694431247 https://www.metooo.io/u/64fef90563f25c796f91de3f https://app.roll20.net/users/12404159/bodrumteknekirala12-b https://list.ly/bodrumteknekirala/activity https://giphy.com/channel/Bodrumteknekirala12 https://www.tumblr.com/bodrumteknekirala12 https://dzone.com/users/4991833/bodrumteknekirala12.html https://www.creativelive.com/student/bodrumteknekirala12?via=accounts-freeform_2 https://gab.com/Bodrumteknekirala12 https://sketchfab.com/Bodrumteknekirala12 https://www.flickr.com/people/199097125@N05/ https://hub.docker.com/u/bodrumteknekirala12 https://profiles.wordpress.org/bodrumteknekirala12/ https://wefunder.com/bodrumteknekirala12 https://seedandspark.com/user/bodrumteknekirala12-01ha25xw5xpdrkba62jrje1c7g https://calis.delfi.lv/blogs/posts/210715-httpsbodrumteknekiralacomtr/lietotajs/314033-bodrumteknekirala12/ https://os.mbed.com/users/bodrumteknekirala12/ https://notionpress.com/author/924454 https://my.desktopnexus.com/Tekneturumarmaris12/ https://guides.co/a/bodrumteknekirala12-bodrumteknekirala12/ https://www.bahamaslocal.com/userprofile/1/241882/Bodrumteknekirala12.html http://molbiol.ru/forums/index.php?showuser=1297859 https://www.credly.com/users/bodrumteknekirala12-bodrumteknekirala12/badges https://www.facer.io/user/NoWOFS0vbP https://ko-fi.com/bodrumteknekirala12#paypalModal https://mastodon.online/@Bodrumteknekirala12 https://devpost.com/bodrumteknekirala http://onlineboxing.net/jforum/user/editDone/251120.page https://www.redbubble.com/people/Tekneturu/shop?asc=u https://linktr.ee/marmaris1 https://www.divephotoguide.com/user/marmaris1/ https://artmight.com/user/profile/2408931 https://allmyfaves.com/marmaris1 https://www.fimfiction.net/user/628252/marmaris https://www.drupalgovcon.org/user/568666 https://www.roleplaygateway.com/member/marmaris1/ https://www.kickstarter.com/profile/825997479/about https://tapas.io/sam659667 https://seedandspark.com/user/marmaris1 https://starity.hu/profil/386591-marmaris1/ https://www.informationweek.com/profile.asp [profil açık içerik kabul etmiyor] https://nootheme.com/forums/users/marmaris1/ https://app.zintro.com/profile/zieb2b6446[eklenecek yer buylamadım] https://app.zintro.com/myaccount?ref=Zieb2b6446[eklenecek yer yok] https://app.roll20.net/users/12308972/marmaris1-m https://www.360cities.net/profile/sam659667 https://fileforum.com/profile/marmaris1 https://wordpress.org/support/users/marmaris1/ https://www.hebergementweb.org/members/marmaris1.539143/ https://forum.cs-cart.com/u/marmaris1/ https://www.tntxtruck.com/User-Profile/UserId/12208 https://calis.delfi.lv/blogs/posts/205779-linkler/lietotajs/310821-marmaris1/ https://profile.ameba.jp/ameba/marmaris1/ https://www.avianwaves.com/User-Profile/userId/184770 https://engine.eatsleepride.com/rider/marmaris1 https://keymander.iogear.com/profile/53051/marmaris1 https://www.mifare.net/support/forum/users/marmaris1/ https://inkbunny.net/marmaris1?&success=Profile+settings+saved. https://www.diggerslist.com/64e0c4fad170b/about https://research.openhumans.org/member/me/ http://bluerevolutioncrowdfunding.crowdfundhq.com/users/marmaris1 https://www.cakeresume.com/me/marmaris1 https://educatorpages.com/site/marrmaris1/pages/about-me? https://gotartwork.com/Profile/marmaris1-marmaris1/253385/ https://www.facer.io/user/OGfo7VWrhR https://able2know.org/user/marmaris1/ https://www.techrum.vn/members/marmaris1.230749/#about http://foxsheets.statfoxsports.com/UserProfile/tabid/57/userId/145739/Default.aspx http://riosabeloco.com/User-Profile/userId/196075 http://phillipsservices.net/UserProfile/tabid/43/userId/245691/Default.aspx http://www.ramsa.ma/UserProfile/tabid/42/userId/962725/Default.aspx http://krachelart.com/UserProfile/tabid/43/userId/1242308/Default.aspx http://kedcorp.org/UserProfile/tabid/42/userId/72907/Default.aspx http://atlantabackflowtesting.com/UserProfile/tabid/43/userId/561626/Default.aspx https://www.intensedebate.com/people/marmaris12 https://rosalind.info/users/marmaris1/ https://wordpress.com/me https://photozou.jp/user/top/3342211
Keywords
Guided tissue regeneration, Periodontal ligament, Guided bone regeneration
Introduction
The utilisation of an occlusive membrane that interfaces with gingival connective tissue/epithelium on one side and PDL/alveolar bone tissues on the other is what GTR is all about. Most tissue will repair itself within biological constraints. Regeneration, on the other hand, is a different story; in the vast majority of cases when tissue loss has occurred, the tissue is unable to return to its prior state. Birth defects, disease, trauma, malignancies, atrophy, or surgical excision can all cause tissue loss at both the patient and the practitioner have always been concerned about the replacement of lost bodily parts [1]. The goal of tissue replacement is to reconstruct or regenerate the structure that has been lost or destroyed as closely as feasible to its original form and function. GBR refers to the notion of guided regeneration, which entails augmenting and restoring inadequate alveolar ridges and extracting sites. GBR (guided bone regeneration) and GTR (Guided Tissue Regeneration) are two types of regeneration (GTR). The term "guided bone regeneration" refers to the process of regenerating bones with the help [2]. Tri-Calcium Phosphate (TCP) is an alloplastic substance that can be used to replace autogenously or other bonn. The concept Guided Tissue Regeneration (GTR) refers to procedures that try to replace damaged periodontal tissues by excluding epithelial and connective gingival tissues out from root and bone surfaces while guided tissue regeneration refers to periodontal attachme nt regeneration. Barrier techniques involving expanded po lytetrafluoroethylene, polyglactin, polylactic acid, calcium sulphate, and collagen are used in the hopes of keeping epithelium and gingival corium away from the root or existing bone surface [3].
Several materials have been utilised and explored in both clinical and experimental contexts. A research study and contextual, on the other hand, found that the strategy to guided tissue regeneration was very diverse between and between experiments [4].
Membrane alterations are being researched intensively in attempt to improve periodontal tissue capacity to heal. In this regard, a stimulant agent containing barrier has also been developed.
Various substances, such as bio ceramics, antiseptics, growth regulators, and small molecules, have been introduced to the membranes with the purpose of aiding and/or promoting periodontal tissue regeneration. Numerous studies have established the enhancing effect imparted by the integration of these drugs with typical directed tissue regeneration procedures. Polycaprolactone (PCL) has been proposed as a potential tissue regeneration biomaterial. Biomaterials are mostly utilised in medicine to replace or enhance natural functions. Metal, composites, polymers, and resins are four types of biomaterials that are commonly utilised in dentistry.
Furthermore, physical properties (such as strength and degradability) could be easily altered. Furthermore, accurate membrane architectural control may be easily created. PCL also has a lower chance of infecting others PRF is a fibrin matrix supplemented with platelets and growth factors. As a result, it's an effective tissue regeneration bio scaffold. Tri-Calcium Phosphate (TCP) is an alloplastic substance that can be used to replace autogenously or other bone replacements. PRF's ability to regenerate is improved when it is mixed with bone replacements.
Literature Review
Classification
Non-resorbable membranes: Millipore (cellulose acetate) filters were utilised to make the first nonresorbable membranes employed in experiments. Commercial teflon membranes were developed because this technology became increasingly popular (PTFE). Non-resorbable materials was utilised in the initial few investigations. Those documents were created using not made specifically to be used in dental procedures. As barrier materials, cellulose filters and EPTFE have been used. Liquid and nutritious goods could travel through them. Their micro porosity, however, prevented cell passage across the barrier (Figure 1) [5,6].
Cellulose filler: Filters composed of cellulose are used to keep connective tissue out. In monkeys was first studied by Nyman and others in primates as well as gingiva cells from the periodontal ligament to pass through the epithelium in order it rejuvenate the injury. The periodontal ligament cementum was removed, as well as the periodontal ligament on the cuspid teeth's side alveolar bone.
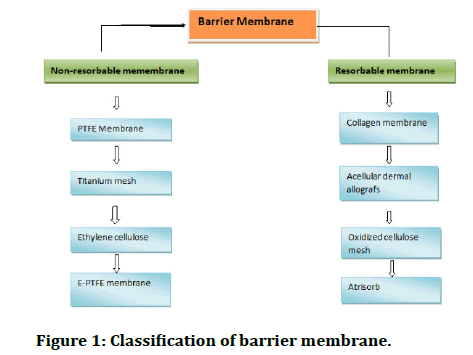
Figure 1: Classification of barrier membrane.
Disadvantages
• Exfoliation
• Premature removal
• The need for a second surgical surgery is all possibilities for their abolition
Expanded poly-tetra fluroethylene membranes
A bacterial filter constructed of cellulose acetate was the first membrane used for GTR in the past. The E-PTFE membrane was developed in response to its poor clinical use, it was utilised for periodontal regeneration in the first published clinical studies. The properties of EPTFE are well known tissue compatibility and inertness.
The porous microstructures make it possible to the formation and connection of connective tissue for the purpose of stabilizing inhibition of epithelial migration and the healing wound complex [7]. There have been two main components to these membrane barriers [8,9].
• The first part is an open microstructure collar (coronal border) that allows for early clot formation and collagen fibre penetration to retain the membrane in place. Through a method known as contact inhibition, the collar may also inhibit epithelial apical development.
• The second component is an occlusive portion that keeps gingival tissues outside the barrier from interfering with the defect site's healing process. Trans-gingival and immersed EPTFE membranes are two different types of EPTFE membranes that can be employed in different scenarios.
• The trans-gingival design is used to treat defects that are associated with structures that extend through the gingiva such as teeth.
• When there is no interaction with the oral environment, such as when there is a skeletal defect, the immersed design has been used.
Titanium reinforced EPTFE membranes: Were created to generate a tent like appearance, which is beneficial when the defect morphology does not allow for enough room. The development and upkeep of a place have long been regarded as essential components of regeneration. Those membranes were developed to be employed in conditions where a defect's anatomy caused non reinforced material to collapse into the defect space, or when there was a need for more. For the desired regeneration, area is required. Titanium reinforced membranes are also available in submerged and transgingival designs [10,11].
Advantage
• Has been that the membrane remains its functional properties for long enough for sufficient healing to occur, within a week of which it can be removed quickly.
• There is no risk of breakdown products interfering with the development of the regenerated tissues after they have been removed.
Resorbable materials and devices
Advantage: Preventing a second surgical treatment, which decreases patient complications and expenditures?
Disadvantage: The disadvantage of utilising bioresorbable membranes is that material exposure or flap haemorrhages might lead to issues with postoperative tissue care. Following surgery, material exposure might result in bacterial development, fibroblast shape changes, and migration, all of which can threaten the regeneration process' effectiveness. Another typical issue is the inability to keep the membrane from collapsing into the defect, which can tead to insufficient space creation [12,13].
Collagen membranes: Collagen has been used as a resorbable membrane for GTR. Whereas collagen membrane has minimal antigenicity, good biocompatibility, and strong cell affinity, pure collagen has the disadvantage of being complex to tackle due to a lack of physical appearances, and it degrades quickly [14,15].
The physical features of the collagen membrane are improved by cross-linking procedures, which successfully extend the absorption duration [12,15,16]. Glutaraldehyde is the most widely used chemical cross linking agent, but it has been reported to be cytotoxic [17-20].
Collagen membranes, like sub epithelial connective tissue grafts and Expanded Polytetrafluoroethylene (E-PTFE) membranes have been employed for root coverage and GBR procedures with good results. Collagenous a periodontal connective tissue macromolecule that has two properties: Chemotactic (for fibroblasts) and haemostatic (for blood vessels). This substance is also a weak immunogenic that could serve as a scaffold for migratory cells. Collagen has various properties that make it an excellent barrier material, including favourable coagulation and wound healing effects. Cross linking in a controlled manner [21]. High tensile strength and fibre orientation, low antigenicity and extensibility. Collagen is also available in a variety of forms (for example, sheets, gels, tubes, powders, and sponges).
Advantage
• Postoperative problems are kept to a minimum.
• A high pace of healing and no signs of material dehiscence.
• Perforation of the tissue.
• Sensitivity is a term that is used to describe how sensitive a person is.
• Immune reaction.
• Sloughing of tissue.
• Postoperative infection or delayed healing.
Polylactic acid: Polylactic acid is a type of biomaterial that is widely used to make cytoskeletons and dressings [22]. The first resorbable barrier to be licenced by the Food and Drug Administration (FDA) for membrane barrier techniques was guider, a bio-resorbable matrix barrier made of a blend of polylactic acid softened with citric acid for malleability and to enable clinical handling. This device is a multi-layered matrix which it encourages soft tissue initiation and progression while inhibiting gingival epithelium apical down growth.
The layer in touch with the bone or tooth (the innermost layer) has circular pattern perforations and multiple space holders to allow for the creation of fresh attachment, whereas the layer in contact with the gingival tissue has no perforations and no space holders. (The outermost layer) includes bigger rectangular pores to allow gingival tissue to quickly grow into the area between the two layers, reducing or limiting epithelial down growth. The material's resorption mechanism is set up to maintain barrier function for at least 6 weeks before slowly resorbing. Resorption is completed after about 12 months [23].
Polyglycolic acid and polylactic acid: Poly (lactic coglycolic acid) PLG is a copolymer with biocompatibility, biodegradability, and process ability that can be manufactured in various forms depending on the ratio of PLA and PGA [24,25].
Bio-resorbable membranes composed of polyglycolic acid and polylactic acid have now been evaluated in experimental animals and shown to be harmless and promote periodontal rejuvenation with minimum inflammatory reaction. The film holds the fibres together while also separating the soft tissue from the flaw. The openness of the fibrous matrix and the random arrangement of the fibres enhance connective tissue regeneration while inhibiting epithelial apical expansion [26-31]. Inflammation, proliferation, repair, and remodelling are all steps in the wound healing process. Platelet degranulation contributes to the start of the inflammatory stage [32].
Equimolar poly glycolic acid: Poly lactide copolymer, and 1 week for polylactide copolymer. When these polymers are present for long durations (4-6 years), they might cause a late localised non-resident reaction, which is defined histologically by the presence of cells, usually frothing macrophages with internal poly lactide fragments.
Synthetic liquid polymer (Atrisorb): Synthetic absorbable barriers are made of organic aliphatic thermoplastic polymers, the most popular of which are poly-hydroxy acids such as polyglycolic acid (-O-CH2- (O)C-)n and polylactic acid (-O-CH(CH3)-(O)C-)n, as well as their copolymer poly glycolidelactide. Through the citric/cycle, Kreb's polyhydroxy acid is hydrolysed into compounds that are metabolised to CO2 and H2O.
A compostable suture fastens the barrier to the tooth in the coronal region of the interspace. In animal experiments, resorption was complete in 6-12 months and the barrier function was maintained for at least 6 weeks. The foreign body reaction, which is characterised by macrophages and multinucleated large cells, is observed three months following surgery [27].
Advantage
• This barrier has the benefit of being hard enough for placement while still being flexible enough to adapt to the flaw.
• Sutures are not required because the barrier clings directly to dental structures. Chemically, the substance is a polymer component that is resorbed via the hydrolysis process.
• The rate of resorption is regulated, and the membrane remains in place during the key healing period, inhibiting epithelial migration and isolating the periodontal defect compartment.
Calcium sulfate: After immediate implant implantation, clinical calcium sulphate, often known as plaster of Paris, was employed as part of an allograft surrounding the implants. Barriers made of clinical calcium sulphate can be placed above bone transplants to keep clots from forming and to keep unwanted tissue out. This substance has several benefits, including supplying a calcium source during the early stages of calcification and helping particle stability.
Calcium sulphate dissipates in around 1 month and it does not attract germs or create infection. Within 3 to 4 weeks, degradation is complete. Bioavailability is an important factor to consider (causes no increase in inflammation) [28].
Advantages
• Flexibility (does not need to be cut before placement).
• Postoperative pain is minimal.
• Porosity (allows fluid exchange but prevents epithelium and connective tissue from passing through).
• During the early phases of healing, clot prevention is essential.
Allografts: Today's clinicians have access to a variety of bone grafting materials that have been employed to produce periodontal regeneration or alveolar ridge repairs. There is about 150 distinct types of bone transplants available a result of material exposure in the United States alone. Periodontal hard tissue replacement materials can be classified into one of four categories: Allogeneic bone replacements, such as Freeze Dried Bone Allograft (FDBA) and Demineralized Freeze Dried Bone Allograft (DFDBA); autogenic; xenogeneic; and alloplastic. These materials are utilised in the clinic to keep soft tissues from collapsing into the defect, as well as to stabilise the clot and aid bone growth [29]. Acellular dermal allografts have numerous benefits over biological dermal allografts.
This material is an excellent choice for membrane barrier approaches because of its colour match and width, as well as the lack of deterioration if initial closure is not accomplished and the creation of extra connected gingiva.
Oxidized cellulose mesh: These barrier membranes are constructed of a resorbable haemostatic barrier material that has shown to be beneficial in GTR treatments. However, it appears to give limited incision space, which could lead to a high rate of cell exclusion. The material's acidic composition could possibly be to blame for the delayed repair of bone tissue after it was used prior to its use as a barrier membrane in GTR operations; more and well-designed clinical investigations of this material are required.
The oxidised material is a resorbable haemostatic treatment that transforms into a viscous mass and absorbs the hematoma to form a membrane. At one week after surgery, the majority of the mesh had reabsorbed into the blood. In this example, the flaws showed signs of normal repair [30].
Clinical indication
• Vertical, multi walled, or narrow defects with vertical bone loss or class II furcation defects should be treated with guided tissue regeneration.
• Periodontal and peri implant abnormalities are the most common indications for guided tissue regeneration operations (dependent upon group contract).
• Because bone grows by secondary intention, guided tissue regeneration operations linked with endodontic therapies or mild periradicular surgery are often not covered benefits. Radiographic pictures revealing vertical bone deficiencies must be included in all connected diagnostic, recently dated, properly oriented, and recognised the documentation of the need for directed tissue regeneration for periodontal purposes.
• Post-operative treatment for the first three months after surgery, as well as any surgical re-entry for three years, is included in guided tissue regeneration procedures (group contract dependent).
Contraindication of GTR
• And medical condition that precludes surgery
• Poor dental hygiene
• Frequent\smoking
• Infection at the defect site
• Horizontal bone loss
• Severe lesions with minimal residual support
• Tooth mobility
• furcation with short root trunk
• Multiple defects
Discussion
The dentally conscious patient with a good degree of oral hygiene may have significant concerns about gingival recession. Who consults the dentist about hygiene treatment for a condition that is deemed unacceptable? Or her principal causes could be a clear indication of old age, an unattractive appearance, or hypersensitive teeth. Recent epidemiologic studies have found evidence suggests gingival recession actually a problem in populations that are industrialised. However, whereas it appears that prevalence is huge even in children and largely limited to buccal surfaces, in terms of both intensity and area maybe rather little, especially in older age ranges [18]. In a research by Loe, et al. [17], it was found noticed that, if true, would mean depth of recession at buccal locations is only about 1.5 mm in total [34]. For biomedical applications, periodontitis, a chronic infectious illness, requires effective treatments. GTR is a useful method to encourage the challenging regeneration of the tissues that support teeth. The current generation of commercial GTR membranes have major limitations, including insufficient mechanical strength and a limited capacity to stimulate the hierarchical the ineffective periodontal regeneration process rate of degradation, etc. Three new GTR membranes are needed. Primary aspirations to interact with clinical properties
• Correct mechanical strength, biocompatibility, and degradation.
• Coordinated and improved PDL regeneration activity bone in the alveoli.
• Antimicrobial activity.
Appropriate biopolymers and additives ought to be assigned to pledge they have excellent biocompatibility. Additionally, additives with biopolymers in the right proportions, it appears promising to control the membrane's rate of deterioration [35].
The regeneration of the periodontal system is crucial to the survival of natural teeth that have been transplanted. A crucial stage in the treatment for periodontal regeneration to modify the root surface in order to hospitable to sustain and promote phenotypic diversity, attachment, proliferation, and migration periodontal connective tissue progenitor cell expression. Among the 11 materials for bone inductive grafts used most frequently in periodontal procedures for regeneration. The can encourage the regeneration of the gums and/or the regrowth of bone nearby depending on the tooth surface on the ability to induce bone formation and the state of the tooth. Materials used for bone grafts don't just both assist the surgical procedure and serve as a scaffold for blood clot formation the flap itself to avoid an early collapse into the healing wounded area [36]. A more recent technique involves using membranes that have been treated with antibacterial substances. The concept of applying antibiotics to membranes for GTR/GBR was inspired by findings that infections have a negative impact on periodontal healing in barrier membrane assisted periodontal therapy, particularly in the initial stages of recovery. At the moment, systemic antibiotics are frequently utilised for following GBR, pathogen growth. Local antibiotic use may be a useful strategy for avoiding infections. Reducing the negative systemic reactions that are caused by periodontal bacteria' detrimental effects connected to this type of therapy. The initial goal of adding antibiotics to the membrane surface was to, attempting to lower the number of pathogens. But it's been demonstrated that antibiotics can offer additional advantages, like postponed collagen deterioration [36].
Conclusion
Several practitioners use guided tissue regeneration as a surgical technique. Despite the word "regeneration" in the phrase, our histological findings is frequently those of a type of repair known as "new bonding." With further periodontal research and business partnerships, we as a profession expect to be able to "regenerate" the periodontal mechanism, including a functional periodontal ligament, one day.
References
- Nyman S. Bone regeneration using the principle of guided tissue regeneration. J Clin Periodontol 1991; 18:494-498.
- Milella E, Ramires PA, Brescia E, et al. Physicochemical, mechanical, and biological properties of commercial membranes for GTR. J Biomed Mater Res 2001; 58:427-435.
- Spector M. Anorganic bovine bone and ceramic analogs of bone mineral as implants to facilitate bone regeneration. Clin Plast Surg 1994; 21:437–444.
- Polson AM, Caton J. Factors influencing periodontal repair and regeneration. J Periodontol 1982; 53:617-629.
- Schmitt JM, Buck DC, John SP, et al. Comparison of porous bone mineral and biologically active glass in critical sized defects. J Periodontol 1997; 68:1043–1053.
- Johnson MW, Sullivan SM, Rohrer M, et al. Regeneration of peri-implant infra bony defects using perioglass: A pilot study in rabbits. Int J Oral Maxillofac Implants. 1997; 12:835–839.
- Zamet JS, Darbar UR, Griffiths GS, et al. Particulate Bio-glass as a grafting material in the treatment of periodontal infra bony defects. J Clin Periodontal 1997; 24:410–418.
- Shepers EJG, Ducheyne P. Bioactive glass particles of narrow size range for the treatment of oral bone defects: A 1-24 months experiment with several materials and particle sizes and size ranges. J Oral Rehab 1997; 24:171–181.
- Furusawa T, Mizunuma K. Osteoconductive properties and efficacy of resorbable bioactive glass as a bone grafting material. Implant Dent 1997; 6:93–101.
- Lekholm U, Wannfors K, Isaksson S, et al. Oral implants in combination with bone grafts. A 3-year retrospective multi-centre study using the brane mark implants system. Int J Oral Maxillofac Surg 1999; 28:181-187.
- Keller EE, Tolman DE, Eckert S. Surgical prosthodontic reconstruction of advanced maxillary bone compromise with autogenously on lay block bone grafts and Osseo integrated endosseous implants: a 12-year study of 32 consecutive patients. Int J Oral Maxillofac Implants 1999; 14:197–209.
- Olson JW, Dent CD, Morris HF, et al. Long term assessment (5 to 71 months) of endosseous dental implants placed in the augmented maxillary sinus. Ann Periodontol 2000; 5:152–156.
- Lee SW, Kim SG. Membranes for the guided bone regeneration. Maxillofac Plast Reconstr Surg 2014; 36:239-246.
- Chu C, Deng J, Sun X, et al. Collagen membrane and immune response in guided bone regeneration: Recent progress and perspectives. Tissue Eng Part B Rev 2017; 23:421-435.
- Lee SW, Kim SG. Membranes for the guided bone regeneration. Maxillofac Plast Reconstr Surg 2014; 36:239-246.
- Tal H, Kozlovsky A, Artzi Z, et al. Long term bio-degradation of cross linked and non-cross linked collagen barriers in human guided bone regeneration. Clin Oral Implants Res 2008; 19:295-302.
- Bunyaratavej P, Wang HL. Collagen membranes: A review. J Periodontol 2001; 72:215-229.
- Speer DP, Chvapil M, Eskelson CD, et al. Biological effects of residual glutaraldehyde in glutaraldehyde tanned collagen biomaterials. J Biomed Mater Res 1980; 14:753–764.
- Simmons DM, Kearney JN. Evaluation of collagen cross linking techniques for the stabilization of tissue matrices. Biotechnol Appl Biochem 1993; 17:23–29.
- Ruhaimi Al. Bone graft substitutes: A comparative quantitative histologic review of current osteoconductive grafting materials. Int J Oral Maxillofac Implants 2001; 16:105–113.
- Rodriguez IA, GS S, Fetz AE, et al. "Barrier membranes for dental applications: A review and sweet advancement in membrane developments". Mouth Teeth 2018; 2:1-9.
- Ashok Sethi, Thomas Kaus. Ridge augmentation using mandibular block bone grafts: Preliminary results of an on-going prospective study. Int J tral Maxillofac Implants 2001; 16:378-388.
- Hua N, Ti VL, Xu Y. Biodegradable effect of PLGA membrane in alveolar bone regeneration on beagle dog. Cell Biochem Biophys 2014; 70:1051-1055.
- Gentile P, Chiono V, Carmagnola I, et al. An overview of Poly (Lactic-Co-Glycolic) Acid (PLGA) based biomaterials tor bone tissue engineering. Int J Mol Sci 2014; 15:3640-3659.
- Tawil G, Mawla M. Sinus floor elevation using a bovine bone mineral (bio-OSS) with or without the concomitant use of a bilayer collagen barrier (bio-Gide): A clinical report of immediate and delayed implant placement. Int J Oral Maxillofac Implants 2001; 16:713-721.
- Tatakis DN, Teughels W, Trombelli L, et al. Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 world workshop on the classification of periodontal and peri-implant diseases and conditions. J Clin Periodontol
- Sjostrom M, Lundgren S, Nilson H, et al. Monitoring of implant stability in grafted bone using resonance frequency analysis. A clinical study from implant placement to 6 months of loading. Int J Oral Maxillofac Surg 2005; 34:45–51.
- Avila Ortiz G, Elengovan S, Karimbux N. Bone grafting substitutes for periodontal use available in the Unites States. Clin Adv Periodontics 2013; 3:187–190.
- Scarano A, Orsini G, Pecora G, et al. Peri-implant bone regeneration with calcium sulfate: A light and transmission electron microscopy case report. Implant Dent 2007; 16:195–203.
- Durge KJ, Baliga VS, Sridhar SB, et al. Extraction socket grafting using recombinant human bone morphogenetic protein 2 clinical implications and histological observations. BMC Res Notes 2021; 14.
- Gawri JA, Shrivastav DS, Agrawal M, et al. Autologous Platelet Rich Plasma (PRP) regeneration to repair in post operated caesarean wounds. J Evo Med Dent Sci 2022; 9:3261–3264.
- Godbole SD, Chandak AV, Balwani TR. Poly Ether Ether Ketone (PEEK) applications in prosthodontics a review “peek into peek at peak.” J Evo Med Dent Sci 2020; 9:3242–3246.
- Loe H, Anerud A, Boysen H. The natural history of periodontal disease in man: Prevalence, severity, extent of gingival recession. J Periodontol 1992; 63:489–495.
- Hassan SU, Bilal B, Nazir MS. Recent progress in materials development and biological properties of GTR membranes for periodontal regeneration. Chem Biol Drug Des 2021; 98:1007-1024.
- Narayanan AS, Bartold PM. Biology of the periodontal connective tissue. Connect Tissue Res 1996; 34:191-201.
- Zohar R, Nemcovsky CE, Kebudi E, et al. Tetracycline impregnation delays collagen membrane degradation in vivo. J Periodontol 2004; 75:1096-1101.
Author Info
Shivani Thakare*, Bhairavi Kale, Khushboo Durge and Pavan Bajaj
Department of Periodontics, Sharad Pawar Dental College and Hospital, Datta Meghe Institute of Medical Sciences (Deemed to be University), Sawangi (Meghe), Wardha, Maharashtra, IndiaCitation: Shivani Thakare, Bhairavi Kale, Khushboo Durge, Pavan Bajaj, Guided Tissue Regeneration Membrane, J Res Med Dent Sci, 2022, 10 (12): 020-025.
Received: 30-Sep-2022, Manuscript No. JRMDS-22-49469; , Pre QC No. JRMDS-22-49469(PQ); Editor assigned: 03-Oct-2022, Pre QC No. JRMDS-22-49469(PQ); Reviewed: 17-Oct-2022, QC No. JRMDS-22-49469; Revised: 19-Dec-2022, Manuscript No. JRMDS-22-49469(R); Published: 26-Dec-2022
