Research Article - (2023) Volume 11, Issue 1
Flexural Strength, Hardness and Surface Roughness of 3D Printed Denture Base Resin Reinforced by Zinc Oxide Nanoparticles
Mostafa Ehsan Al-Douri* and Mohammed Mouyad Sadoon
*Correspondence: Mostafa Ehsan Al-Douri, Department of Prosthetics Dentistry, College of Dentistry, Mosul University, Mosul, Iraq, Email:
Abstract
Aim: Examine the influence of Zinc Oxide (ZnO) nanoparticles on the flexural strength hardness and surface roughness of 3D printed denture base resin.
Materials and methods: The study was conducted by adding ZnO nanoparticles in concentrations of 2%, 3% and 4% to 3D printed denture base resin and assessing the influence of the addition on some mechanical and physical characteristics of the resin, including flexural strength, hardness and surface roughness. The findings were evaluated using descriptive
statistics (standard deviations and means), Analysis of Variance (ANOVA) and duncan's multiple range tests using the SPSS software.
Results: The results showed statistically significant increases in flexural strength values for nanoparticles employed at all concentrations, with the highest flexural strength seen at the 3% concentration. The findings also showed that the shore hardness was not affected by the nanoparticle’s additions. All concentrations employed in the investigation resulted in a
statistically significant reduction in surface roughness.
Conclusion: ZnO appeared to be a viable material for addition to the 3D printed denture base resin, as it boosted flexural strength while lowering surface roughness, although the hardness appeared to be unaffected.
Keywords
3D, Printer, Resin, Denture base, Acrylic, Nanoparticles
Introduction
Acrylic resin is one of the most well-known materials used to manufacture partial and complete dentures. It was developed for dental use after its invention in 1937. Acrylic resins contain numerous types of activators that initiate polymerization and material hardening; heat cure acrylic is the most often used material in denture manufacture [1,2].
Low mechanical qualities of heat cure acrylic led to polymerization shrinkage and flaws in the final prosthesis, necessitating a new fabrication procedure and a new replacement. Another major drawback of heat cured acrylic is that it takes lengthy processing processes and extended fabrication time with a trained technician who can create a fine wax model to be replaced by acrylic resin. Increasing the number of processes and materials utilized in the process increases manufacturing mistakes and reduces the quality of the finished prosthesis [3-5].
As technology advances, new computerized processes for the manufacture of dental prostheses emerge. The development of 3D printers (also known as additive manufacturing technology) is one of these technologies [6]. In the 1980’s 3D printing technology was suggested [7]. The first 3D printing technology is photo curable printing. The technology is based on photo polymerization and photosensitive liquid resin is utilized as the material [8].
Three dimensional printing has a high printing resolution that can print objects as small as 50 m. Therefore, it has the benefit of printing smaller objects with high precision [9]. Due to the excellent accuracy and rapid polymerization rate of photo curing, models may be swiftly produced due to the technique's polymerization rate. A further advantage of 3D printers is that they eliminate the requirement for several laboratory procedures of molding and lengthy steps of conventional heat cured acrylic resin prostheses [10,11].
Despite the numerous advantages described for 3D printers, the resin substance has weaker characteristics compared to traditional materials such as heat cure acrylic and CAD-CAM resin [12,13].
Nanoparticles are being utilized in material science for their resistance to wear and tear and anti-corrosion properties. The modification of filler size enhances the material's characteristics [14].
In recent years, ZnO nanoparticles have garnered more interest as one of the multipurpose inorganic nanoparticles due to their unique optical, biochemical, electrical, biological, biocompatibility, cheap cost, nontoxic and long term environmental stability [15].
Salahuddin, et al. and Vikram and Chander reported that the inclusion of ZnO nanoparticles at various concentrations raised the flexural strength of acrylic resin while also enhancing some physical and mechanical aspects of denture base acrylics [16,17].
Materials and Methods
Samples preparation
To produce a homogeneous combination of the nanoparticles with the resin, the weighted nanoparticles were added to the resin and combined in a mechanical mixer for 60 minutes at 500 revolutions per minute before being put in an ultrasonic vibrator with 40 watts of power for another 60 minutes to guarantee the nanoparticles were evenly distributed in the resin [18].
The computer application Lychee Slicer® is used to construct 3D modules, which are then saved as STL files and utilized to conduct various tests on the study material. Samples designed in 3D are given a base and support and their slicing and printing settings are adjusted before they are exported to the printer.
The commercial 3D printer Anycubic photon mono® (Shenzhen, China) is utilized [19]. According to the manufacturer's instructions, the Z axis thickness of the employed slices is 50 microns and the curing time is 7 seconds per slice. Each batch of samples of the same material had been printed on the same plate, using the same printing cycle, at the same settings and in the same room temperature environment, in order to eliminate any variance in conditions and standardize the samples.
Upon completion of the printing process, the group of samples is sent to the Anycubic® washing and curing machine (Shenzhen, China) and according material manufacturer's instructions. The samples were cleaned for four minutes in a spinning machine with 99 percent isopropyl alcohol to remove uncured resin and minimize the amount of residual monomer on the samples' surface. The base and support access materials are carefully removed with a sharp blade and the samples are examined for flaws.
The samples were then taken from the spinning washing machine and dried with moderate air pressure for thirty seconds before being reintroduced to the curing machine to finish the curing cycle using blue light with a wavelength of 405 nm and a spinning curing table for forty five minutes [20].
Experimental tests of the study
Flexural strength: According to ISO (20795-1:2013) requirements, (64 × 10 × 3.3 ± 0.2) mm specimens were made for each of five groups, totaling twenty specimens [21]. Before testing, all specimens were stored for (48 ± 2) hours at 37°C in deionized distilled water [22,23].
This test utilized three points loading using universal testing machine (Gester, total testing solution). In accordance with ISO (20795-1:2013) requirements, the test machine is equipped with a central loading plunger, two supports with a 3.2 mm radius polished cylindrical surface and a 50 mm spacing. The supports are parallel to one another and perpendicular to the center line. The loading plunger is positioned midway between the two supports. The force velocity was 5 mm/min. The test was conducted at a constant rate of 5 mm/min [24]. The specimen was deflected while the loading plunger force steadily increased from zero until fracture and the fracture load was documented in Neutin. The following formula was used to calculate the flexural strength in mega pascal [25].
σ=3FL/2bh2
Where, F:Maximum load before fracture; L:Distance between the supports; b:Width of the specimen; h:Height of the specimen.
Surface roughness: Twenty samples were manufactured, five for each group and measuring 12 mm by 12 mm by 3 mm. The samples were conditioned in deionized distilled water at room temperature 37°C for (48 ± 2) hours (ISO, 20795-1:2013).
The test was conducted with a portable roughness tester (TR 220, beijing, time high technology Ltd, China). Three measurements are conducted in various directions for each sample and the average result is determined as the mean roughness reading. The device's optical lens rotates along a length of 11 mm to capture the micro irregularities of the surface and produce a chart for the surface with the average reading for each individual test [26,27].
Hardness: Five specimens were prepared for each group, each measuring 12 mm by 12 mm by 3 mm in accordance with ISO (20795-1:2013). The samples were conditioned in deionized distilled water at room temperature for (48 ± 2) hours 37°C. The test was conducted with a digital durometer hardness tester (shore D) (TH 210, Beijing, time high technology Ltd, China). For each specimen, five readings were collected and the mean value was determined. The instrument comprises of a blunt indenter (0.8 mm in diameter) that is housed in a cylinder (1.6 mm in diameter) that is connected to a digital screen that displays values from zero to one hundred units. The specimen was placed on the solid plane of the device and the indenter was held near to the specimen's center. On the sample, a fixed minor load of 44.5 N was applied. The durometer tester automatically translates the relative movement of the indenter immediately after each indentation to a scale of 0 to 100 units [28].
Results
Flexural strength
The means and standard deviation for flexural strength values for all experimental groups shown in the Table 1.
| Descriptive statistics | |||
|---|---|---|---|
| N | Mean | Std. deviation | |
| Control | 5 | 111.4394 | 4.78622 |
| ZnO 2% | 5 | 119.3213 | 4.57692 |
| ZnO 3% | 5 | 126.1168 | 5.25242 |
| ZnO 4% | 5 | 106.3335 | 5.42946 |
Table 1: Means and standard deviation of flexural strength for control and nanoparticles modified resin groups.
Highest flexural strength seen in resin modified with 3% ZnO nanoparticles (126.11 ± 5.25) and the lowest flexural strength value for resin modified with 4% ZnO (106.33 ± 5.42).
Analysis of variance of ZnO groups demonstrated in Table 2. The flexural strength value of different concentration nanoparticles added had statistically significant differences between experimental and control group.
| ANOVA | |||||
|---|---|---|---|---|---|
| Sum of squares | df | Mean square | F | Sig. | |
| Between groups | 1137.332 | 3 | 379.111 | 15.026 | 0.000 |
| Within groups | 403.692 | 16 | 25.231 | ||
| Total | 1541.024 | 19 | |||
Table 2: ANOVA for flexural strength of modified resin with ZnO nanoparticles.
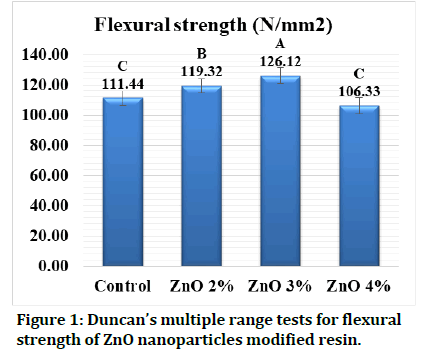
Duncan’s multiple range tests revealed that there is an increase in flexural strength with increasing ZnO nanoparticle concentration and the peak strength with the 3% ZnO nanoparticles concentration (Figure 1). Drop of the strength is seen in concentration 4% ZnO nanoparticles but in this concentration, there is statistically no significant difference with the control group.
Figure 1: Duncan’s multiple range tests for flexural strength of ZnO nanoparticles modified resin.
Hardness
Descriptive statistics of hardness values for all groups demonstrated in Table 3.
| Descriptive statistics | |||
|---|---|---|---|
| N | Mean | Std. deviation | |
| Control | 5 | 87.6367 | 1.14918 |
| ZnO 2% | 5 | 87.195 | 0.47183 |
| ZnO 3% | 5 | 87.08 | 1.49618 |
| ZnO 4% | 5 | 86.005 | 1.7825 |
Table 3: Means and standard deviation of hardness for control and nanoparticles modified resin groups.
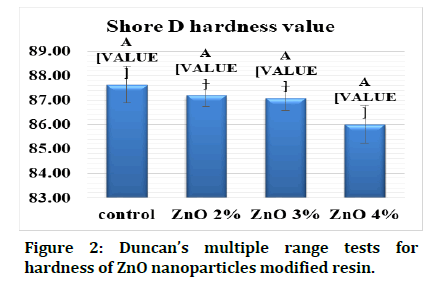
The shore D hardness of control group had the highest between all groups (87.63 ± 1.14) and the 4% ZnO concentration had the lowest hardness among other variances (86 ±1.78).
For the hardness of ZnO nanoparticles groups, ANOVA test viewed in the Table 4 found that there is no statistically significant in hardness from addition of different concentrations of the nanoparticles.
| ANOVA | |||||
|---|---|---|---|---|---|
| Sum of squares | df | Mean square | F | Sig. | |
| Between groups | 7.19 | 3 | 2.397 | 1.378 | 0.286 |
| Within groups | 27.836 | 16 | 1.74 | ||
| Total | 35.027 | 19 | |||
Table 4: ANOVA for hardness of modified resin with ZnO nanoparticles.
With Duncan’s multiple range tests in the Figure 2, it is noticed that the values of shore D hardness are decreasing in linear manner with increasing concentration of the ZnO nanoparticles but there are no statistically significant differences.
Figure 2: Duncan’s multiple range tests for hardness of ZnO nanoparticles modified resin.
Surface roughness
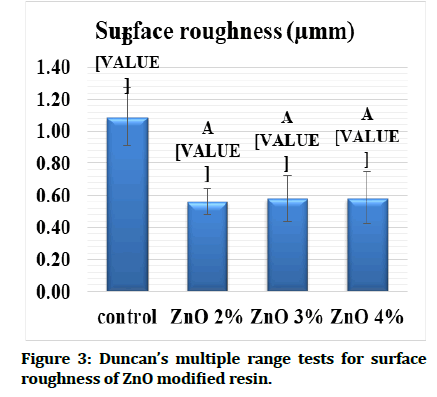
Descriptive statistics for surface roughness demonstrated in Table 5 where the control group had the highest value of surface roughness between other test groups and the 2% addition of ZnO nanoparticles had the lowest roughness.
| Descriptive statistics | |||
|---|---|---|---|
| N | Mean | Std. deviation | |
| Control | 5 | 1.0917 | 0.18328 |
| ZnO 2% | 5 | 0.5615 | 0.07821 |
| ZnO 3% | 5 | 0.5843 | 0.14232 |
| ZnO 4% | 5 | 0.5858 | 0.26401 |
Table 5: Means and standard deviation of surface roughness for control and nanoparticles modified resin groups.
Analysis of variance test for ZnO nanoparticles groups listed in the Table 6. The test gives statistically significant difference between experimental groups and control group.
| ANOVA | |||||
|---|---|---|---|---|---|
| Sum of squares | DF | Mean square | F | Sig. | |
| Between groups | 0.995 | 3 | 0.332 | 10.226 | 0.001 |
| Within groups | 0.519 | 16 | 0.032 | ||
| Total | 1.513 | 19 | |||
Table 6: ANOVA for surface roughness of modified resin with ZnO nanoparticles.
Duncan’s multiple range test in Figure 3 illustrated that all groups decreased in surface roughness of the samples and had statistically significant difference from the control group with lowest value in 2% concentration of ZnO nanoparticles but the roughness is increasing with the concentration of nanoparticle is increasing yet it still lower than the control group.
Figure 3:Duncan’s multiple range tests for surface roughness of ZnO modified resin.
Discussion
Flexural strength
Flexural strength of material has been regarded as the primary mode of clinical failure; therefore, enhancing the flexural strength of dental appliances, particularly denture bases, is a crucial criterion because they are subjected to deforming loads that could cause fractures primarily during use [29].
The results demonstrated an increase in flexural strength with increasing the concentration ZnO nanoparticles. The highest flexural strength seen in 3% ZnO nanoparticles experimental group (126.11 ± 5.25) which is statistically different from control group that has flexural strength (111.43 ± 4.78). The results also showed decrease with ZnO 4% concentration group (106.33 ± 5.42).
This rise in experimental groups may be attributable to the nanoparticle's role as filler that incorporates into the resin matrix, hence reducing gaps and spaces and fractures in the resin material [30]. In addition, the appropriate distribution of nanoparticles enables them to penetrate between the linear chains of the polymer, resulting in a decrease in polymer chain mobility and an increase in flexural strength [31].
The expansion of nanoparticles in response to an applied stress may also increase flexural strength by causing crack compression and cessation of fracture propagation. Thus, the dispersed filler particles are able to prevent a crack from propagating through the resin, a process known as dispersion strengthening [32].
Improvement of flexural strength with addition ZnO agrees with Salahuddin, et al. that concluded the PMMA reinforcement with the filler of ZnO nanoparticles, the flexural strength of the obtained composites was improved in the low concentrations (under 1%).
Addition of ZnO nanoparticles in concentration 4% leads to decrease in flexural strength as opposite to the lower concentrations. This may be explained by a decrease in the cross section of the load bearing area of polymer matrix. It's also possible that too many filler particles are causing stress concentration [33]. One of the possible causes of this decline is incomplete resin wetting of the fillers. Also, the fact of ZnO functions as an interfering component in the polymer matrix's integrity [34].
Flexural strength reduction with addition of high concentrations of ZnO nanoparticles agrees with Khan, et al. who concluded that the addition of different high concentrations (5, 10, 15 and 20%) of ZnO nanoparticles leads to decrease in flexural strength of heat cured PMMA denture base resin [35].
Hardness
Effectively, the hardness test has been used to measure the degree of polymerization of resin based composite materials and the degree of conversion of various types of acrylics. The degree of polymeric matrix resistance to degradation demonstrated by the hardness of denture base materials, which impacts the longevity of the denture base within the oral cavity. Because higher hardness values are often associated with increased wear resistance.
Zinc oxide nanoparticles that had been added to the resin seemed to have no effect on the hardness of the material. Shore D hardness test for experimental groups showed that the addition of nanoparticles to 3D printed denture base resin leads to decrease in the hardness without any statistically significant difference. This result disagrees with Salahuddin, et al. and Vikram and Chander who used various concentrations of zinc oxide nanoparticles on PMMA denture base material and found that all concentrations increased hardness compared to the control group.
Surface roughness: Surface roughness encourages numerous types of bacteria, such as Candida albicans, to improve adhesion and retention, which is crucial in denture induced stomatitis. Therefore, an appropriate material should have a smooth, polished surface to limit or eliminate plaque formation [36].
This study results showed a statistically significant decrease in surface roughness of 3D printed denture base resin with addition of ZnO nanoparticles in all concentrations.
Zidan, et al. explained that the inclusion of nanoparticles would fill the micro gaps between the particles and matrix of the resin, hence minimizing the irregularities of the surface and voids that may occur on the surface of the samples during the processing of the denture base material [37]. The surface roughness may reduce as a result of these factors.
Findings also agrees Abd Alwahab, et al. who investigated the influence of ZnO nanoparticles addition on roughness properties of PMMA denture base with different concentrations (1, 2, 3, 4 and 5 wt%) [38]. Surface roughness had been noticed to be significantly decreased with the addition of nanoparticles that had been used.
Sadoon also employed ZnO nanoparticles on soft liner and discovered that the surface roughness decreased with the addition of various types and concentrations of nanoparticles utilized in the study [39].
Results disagree with Cierech, et al. that stated the addition of zinc oxide nanoparticles in various concentrations has no effect on the surface roughness of the PMMA denture base resin [40].
Conclusion
The addition of ZnO nanoparticles enhanced the mechanical and physical properties of 3D printed denture base resin especially in higher concentration. The flexural strength seemed to be improved with ZnO nanoparticles addition and the roughness also decreased leading to smoother surface, meanwhile the hardness looks as if it is not affected by these additions.
References
- Peyton FA.History of resins in dentistry. Dent Clin North Am 1975; 19:211-222. [Googlescholar][Indexed]
- Rueggeberg FA. From vulcanite to vinyl, a history of resins in restorative dentistry. J Prosthet Dent 2002; 87:364-379. [Crossref][Googlescholar][Indexed]
- Narva KK, Lassila LV, Vallittu PK. The static strength and modulus of fiber reinforced denture base polymer. Dent Mater J 2005; 21:421-428. [Crossref][Googlescholar][Indexed]
- Takahashi Y, Hamanaka I, Shimizu H.Flexural properties of denture base resins subjected to long term water immersion. Acta Odontol Scand 2013; 71:716-720. [Crossref][Googlescholar][Indexed]
- Sasaki H, Hamanaka I, Takahashi Y, et al. Effect of long term water immersion or thermal shock on mechanical properties of high impact acrylic denture base resins. Dent Mater J 2016; 35:204-209. [Crossref][Googlescholar][Indexed]
- Hull CW. Apparatus for production of three-dimensional objects by stereolithography. United States Patent, Appl., No. 638905, Filed. 1984.
- Crump SS. Apparatus and method for creating three dimensional objects (US Patent US5121329A). 1992. [Googlescholar][Indexed]
- Revilla‐Leon M, Meyers MJ, Zandinejad A, et al.A review on chemical composition, mechanical properties and manufacturing work flow of additively manufactured current polymers for interim dental restorations. J Esthet Restor Dent 2019; 31:51-57. [Crossref][Googlescholar][Indexed]
- Wang J, Stanic S, Altun AA, et al. A highly efficient waterborne photo initiator for visible-light-induced three dimensional printing of hydrogels. Chem Commun 2018; 54:920-923. [Crossref][Googlescholar][Indexed]
- Quan H, Zhang T, Xu H, et al. Photo curing 3D printing technique and its challenges. Bioact Mater 2020; 5:110-115. [Crossref][Googlescholar][Indexed]
- Wu L, Zhao L, Jian M, et al.EHMP-DLP: Multi projector DLP with energy homogenization for large size 3D printing. Rapid Prototyp J 2018. [Crossref][Googlescholar][Indexed]
- Zaharia C, Gabor AG, Gavrilovici A, et al. Digital dentistry 3D printing applications. J Interdiscip Med 2017; 2:50-53. [Crossref][Googlescholar][Indexed]
- Al-Qarni FD, Gad MM. Printing accuracy and flexural properties of different 3D printed denture base resins. Materials 2022; 15:2410. [Crossref][Googlescholar][Indexed]
- Ali Sabri B, Satgunam M, Abreeza NM, et al.A review on enhancements of PMMA denture base material with different nano fillers. Cogent Eng 2021; 8:1875968. [Crossref][Googlescholar][Indexed]
- Xiong HM. ZnO nanoparticles applied to bio-imaging and drug delivery. Adv Mater 2013; 25:5329-5335. [Crossref][Googlescholar][Indexed]
- Salahuddin N, El‐Kemary M, Ibrahim E. Reinforcement of polymethyl methacrylate denture base resin with ZnO nanostructures. Int J Appl Ceram Technol 2018; 15:448-459. [Crossref]
- Vikram S, Chander NG. Effect of zinc oxide nanoparticles on the flexural strength of polymethyl methacrylate denture base resin. Eur Oral Res 2020; 54:31-35. [Crossref][Googlescholar][Indexed]
- Chen S, Yang J, Jia YG, et al. A study of 3D printable reinforced composite resin: PMMA modified with silver nanoparticles loaded cellulose nanocrystal. Materials 2018; 11:2444. [Crossref][Googlescholar][Indexed]
- Herpel C, Tasaka A, Higuchi S, et al. Accuracy of 3D printing compared with milling: A multi-center analysis of try in dentures. J Dent 2021; 110:103681. [Crossref][Googlescholar][Indexed]
- Zeidan AA, Sherif AF, Baraka Y, et al. Evaluation of the effect of different construction techniques of CAD‐CAM Milled, 3D printed, and polyamide denture base resins on flexural strength: An in vitro comparative study. J Prosthodont 2023; 32:77-82. [Crossref][Googlescholar][Indexed]
- International Standards Organization (ISO). Dentistry base polymers part 1: Denture base polymers. ISO, 20795-1, Standardization, 2nd Edition, Geneva, Switzerland. 35.
- Prpic V, Schauperl Z, Catic A, et al. Comparison of mechanical properties of 3D printed, CAD/CAM, and conventional denture base materials. J Prosthodont 2020; 29:524-528. [Crossref][Googlescholar][Indexed]
- Chhabra M, Kumar MN, Raghavendra Swamy KN, et al. Flexural strength and impact strength of heat cured acrylic and 3D printed denture base resins: A comparative in vitro study. J Oral Biol Craniofacial Res 2022; 12:1-3. [Crossref][Googlescholar][Indexed]
- Al-Nema LM (2005). Evaluation of Fatigue Fracture of an Acrylic Resin Denture Base Material (an in Vitro Study). M.Sc. Thesis, University of Mosul, College of Dentistry. Mosul, Iraq.
- Altaee NW, Al-Ali AA. The effects of magnesium oxide nanoparticles addition on flexural strength of cold cured acrylic resin material. R Dent J 2022; 22:101-112. [Crossref][Googlescholar][Indexed]
- Al-Hiloh SA, Ismail IJ.A study the effect of addition of silanized zirconium oxide nanoparticles on some properties of high impact heat cured acrylic resin. J Baghdad Coll Dent 2016; 325:1-7. [Crossref][Googlescholar]
- Sattar Salman IA, Shukur BN. The influence of bio-surfactant on hardness and roughness of heat cured acrylic resin. Indian J Public Health 2020; 11:1381. [Googlescholar]
- Basima MA, Aljafery AM. Effect of addition ZrO2-Al2O3 nanoparticles mixture on some properties and denture base adaptation of heat cured acrylic resin denture base material. J Baghdad Coll Dent 2015; 27:15-21. [Crossref][Googlescholar][Indexed]
- Shen C, Rawls HR, Esquivel-Upshaw JF. Phillips' science of dental materials e-book. Elsevier Health Science, 13th Edition, United State, 2022.
- Salih SE, Oleiwi JK, Alaa Mohammed T. Investigation of hardness and flexural properties of PMMA nano composites and PMMA hybrids nano composites reinforced by different nano particles materials used in dental applications. Eng Technol J 2016; 34:2838 ̶ 2853. [Crossref][Googlescholar][Indexed]
- Ihab NS, Moudhaffar M. Evaluation the effect of modified nanofillers addition on some properties of heat cured acrylic denture base material. J Baghdad Coll Dent 2011; 23:23-29. [Googlescholar][Indexed]
- McCabe JF, Walls A. Applied dental materials. John Wiley and Sons, 9th Edition, UK, 2013. [Googlescholar][Indexed]
- Jagger DC, Harrison A, Jandt KD. The reinforcement of dentures. J Oral Rehabil 1999; 26:185-194. [Crossref][Googlescholar][Indexed]
- Schulze KA, Zaman AA, Soderholm KJ. Effect of filler fraction on strength, viscosity and porosity of experimental compomer materials. J Dent 2003; 31:373-382. [Crossref][Googlescholar][Indexed]
- Khan H, Raza M, Khan TA. Comparison of flexural strength of zinc nanoparticles reinforced resin with conventional heat cured acrylic resin. Pak Oral Dental J 2020; 40:51-54. [Googlescholar][Indexed]
- Rao DC, Kalavathy N, Mohammad HS, et al. Evaluation of the surface roughness of three heat-cured acrylic denture base resins with different conventional lathe polishing techniques: A comparative study. J Indian Prosthodont Soc 2015; 15:374-380. [Crossref][Googlescholar][Indexed]
- Zidan S, Silikas N, Alhotan A, et al. Investigating the mechanical properties of ZrO2 impregnated PMMA nanocomposite for denture based applications. Materials 2019; 12:1344-1358. [Crossref][Googlescholar][Indexed]
- Abd Alwahab S, Moosa JM, Muafaq S. Studying the influence of nano ZnO and nano ZrO2 additives on properties of PMMA denture base. Indian J Public Health Res Dev 2020; 11:2047-2051. [Crossref][Googlescholar][Indexed]
- Sadoon MM. The Effect of different nanoparticles incorporation on some properties of acrylic based soft liner. Ph.D. dissertation. Mosul university, College of Dentistry. Mosul. Iraq. Al-Rafidain Dent J 2021; 22:158-169. [Crossref]
- Cierech M, Osica I, Kolenda A, et al. Mechanical and physicochemical properties of newly formed ZnO-PMMA nanocomposites for denture bases. Nanomaterials 2018; 8:305. [Crossref][Googlescholar][Indexed]
Author Info
Mostafa Ehsan Al-Douri* and Mohammed Mouyad Sadoon
Department of Prosthetics Dentistry, College of Dentistry, Mosul University, Mosul, IraqCitation: Mostafa Ehsan Al-Douri, Mohammed Mouyad Sadoon, Flexural Strength, Hardness and Surface Roughness of 3D Printed Denture Base Resin Reinforced by Zinc Oxide Nanoparticles, J Res Med Dent Sci, 2023, 11 (01): 194-200.
Received: 25-Oct-2022, Manuscript No. JRMDS-22-67559; , Pre QC No. JRMDS-22-67559 (PQ); Editor assigned: 28-Oct-2022, Pre QC No. JRMDS-22-67559 (PQ); Reviewed: 11-Nov-2022, QC No. JRMDS-22-67559; Revised: 27-Dec-2022, Manuscript No. JRMDS-22-67559 (R); Published: 25-Jan-2023