Research - (2020) Volume 8, Issue 3
Fibromyxoma of MaxillaâÂÂA Case Report of Rare Odontogenic Tumor
Praveen Kumar Pandey*, Dipyaman Sen, Manish Kumar, Vikrant Kunwar, Neha Upadhyay and Chandan Kumar
*Correspondence: Praveen Kumar Pandey, Dept of Oral & Maxillofacial Surgery, Chandra Dental College and Hospital, Barabanki, Uttar Pradesh, India, Email:
Abstract
Fibromyxoma is a benign, painless, and locally destructive tumor is quite a rare finding of oral cavity. The etiology of tumor is unknown, but mandible has been found to be more commonly involved than maxilla. Moreover, its limited occurrence to the teeth bearing areas and occasional presence of odontogenic epithelial fragments within the tumor is suggestive of odontogenic origin. It’s histological and radiological features makes a fibromyxoma difficult to differentiate from other odontogenic tumor leading to its misinterpretation as malignant lesion and therefore we here present a rare case of fibromyxoma of maxilla describing its clinical and radiological aspects with its post-operative follow up.
Keywords
Fibromyxoma, Myxoma, Odontogenic, Mesenchymal, Tumor
Introduction
The term myxoma was first used by Virchow in 1863, but the term fibromyxoma was described by Dietrich et al. [1]. Odontogenic fibromyxoma is a benign neoplasm which shows a slow growing pattern, usually occurring in 2nd and 3rd decades of life, rarely in children or adult over 50 year of age [2,3]. Although it is an uncommon lesion accounting for only 1% to 3%. Of all cyst and tumors of the jaw, fibromyxoma are aggressive mesenchymal tumor that are gradually expanding and locally destructive [4]. Mandible is more frequently affected than maxilla and occurring more commonly in female than male. The myxomas of usually appears a solitary growth and they are extremely rare in children under the age of twelve years [4]. Some studies reveal a lack of sex predilection and equal frequency of the maxillary and mandibular involvement [5]. Although the origin of myxoma is still obscure an origination from the dental follicle seems to be the most reasonable explanation [2]. The aim of this case report is to put forth a rare occurrence of fibromyxoma of the maxilla, its differential diagnosis and importance of meticulous enucleation in order to prevent recurrence. Marcove et al. in 1964 further elaborated fibromyxoma reporting its extragnathic location [6,7].
The authors declare that they have no conflict of interest. The work described in our article has been carried out in accordance with the code of ethics of the World Medical Association (Declaration of Helsinki) and the appropriate consent was taken from the patient’s guardians for the excisional biopsy performed. The work conducted was approved by the Ethical Committee of the Institutional Board. Informed consent was taken from the patient and patient’s guardian for being the part of research work. Time period of the study was July 2017 to March 2020.
Case Description
A 42-year-old female came to the department of oral and maxillofacial surgery of Chandra Dental College and Hospital, Barabanki. She gave the history of swelling on the right side of face which initiated around 9 months back. The skin over the swelling was normal without any discoloration. However, the patient complained of the pricking pain which was continuous and radiating up to the ear and neck region. Extra oral examination revealed diffused swelling over the right middle third of the cheek involving lateral part of the nose and infra orbital region. The swelling was roughly oval approximately 5 by 2 cm in size. On palpation mild rise in temperature and tenderness was felt. Surface skin did not show any sign of altered color and texture. The swelling was firm in consistency and motor and sensory nerve function was intact. Intra oral diffused swelling was seen in relation to teeth 13-18. The swelling extending from mesial of 13 to the distal of 18. Swelling was primarily on the buccal side, completely obliterating the buccalsulcus. Mucosa over the swelling was normal without any draining sinuses. On the palatal surface it is 2 cm away from the midline of palate. The swelling was tender, soft to firm in consistency, all visual findings were confirmed, and tooth 16 exhibited grade II mobility. Head and neck examination were negative for any lymphadenopathy. Orthopantomography revealed an ill-defined mixed radiolucency in the right maxilla with displacement of adjacent teeth. Computed tomography (CT) Scan of face revealed a septate, expansile mass in the maxillary portion on the right side measuring approximate 6by 2cm with extending 1cm towards the midline of palate. There were associated area of multilocular radiolucency & incisional biopsy was performed and the mass was diagnosed as fibromyxoma (Figures 1 to 3).
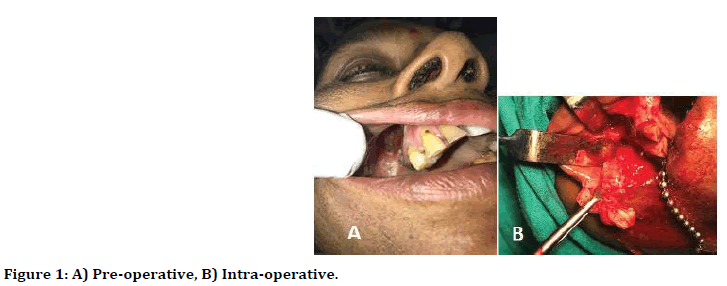
Figure 1. A) Pre-operative, B) Intra-operative.
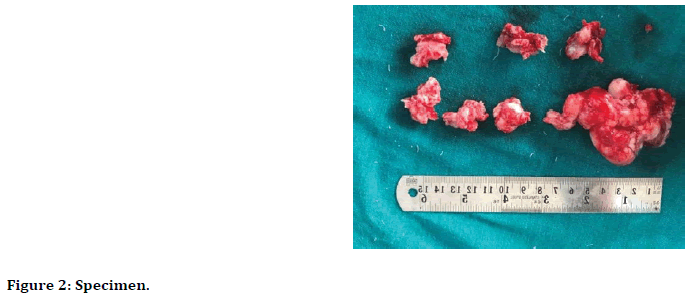
Figure 2. Specimen.
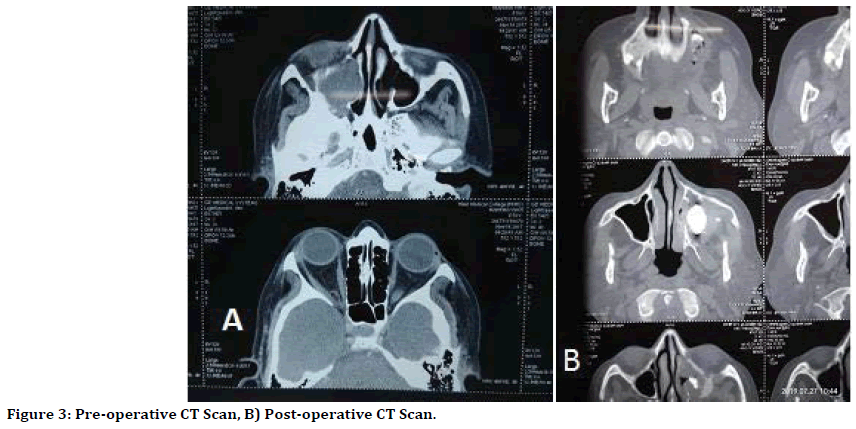
Figure 3. Pre-operative CT Scan, B) Post-operative CT Scan.
Discussion
An incisional biopsy was performed under local anesthesia and histopathological examination revealed the lesion as fibromyxoma, a tumor consist of a proliferation of plumped, spindle, mesenchymal cells with stellate cytoplasm in a background of interspersed collagen fibers admits interstitial basophilic myxoid ground substances. A course of analgesic and antibiotic was given to reduce pain and likelihood of spread infection.
Given the diagnosis and extensive involvement of maxilla, the patient underwent complete enucleation of the lesion and marginal resection with approximately 1 cm of margin by an intra oral approach under general anesthesia. The decision was made to differ definitive reconstruction with any flaps or bone grafts planned as secondary intentional healing by iodoform gauze impregnated with gel foam placed every 5th day consecutively. On resection the tumor appeared as a white-pink multinodular, ill defined, partially encapsulated mass. Patients came for regular follow-ups, and there was no recurrence of the lesion with good intra oral healing.
Fibromyxoma is aggressive but rare intraosseous lesion. It seems to occur more frequently in the second and third decade of life. Myxoma and fibromyxoma are usually located intra orally most often in the posterior region of mandible, its angle and ramus and rarely extra oral [8,9]. Some literatures refer to myxoma as quite common in the mandible, usually associated with the missing teeth [10,11]. However, the maxilla and the anterior region of mandible are the region of rare occurrence.
Coming to it development, there are two schools of thought related to the origin of fibromyxoma. Some believe it to be of odontogenic ectomesenchyme origin because it bears resemblance to the stellate reticulum, associated with missing or unerupted teeth, and it has occasional presence of odontogenic epithelium [10]. Other believe it to be an odontogenic fibroma that has under gone myxomatous changes, suggesting that the connective tissues cells are actively secreting an abundance of intercellular myxoid substance containing hyaluronic acid, chondroitin sulphate and varying amount of collagen fiber [10,12].
Evidence that may support the odontogenic origin of fibromyxoma of the jaw contributed by Abios, et al. [10]. Goldblatt did an ultrastructural study of myxomas cells shows many characteristics of fibroblast of the odontogenic apparatus thus, tumor origin from nonodontogenic mesenchyme cannot be ruled out by existing utrastructural studies [13]. Although maxilla is rare site of occurrence of fibromyxoma but when found in maxilla it usually behaves more aggressively than that of the mandible. It involves the zygoma, maxillary sinus and even the orbit. Most Myxoma are asymptomatic, although some patients present with progressive pain in lesion involving the maxilla and maxillary nerve with eventually leading to neurological disturbance.
Sign and symptoms
Fibromyxoma is greyish yellow multinodular tissues some portion of the tumor may be sticky, gelatinous, or semisolid and other may be firm. The surface of the tumour is shiny and glistening. When coming to symptoms most myxomas are asymptomatic, however some cases shows progressive pain especially when the lesion involves maxilla and maxillary sinus eventually leading to neurological disturbances. Fibromyxoma is however associated with extensive bone destruction, invasion in the surrounding structures and relatively high recurrence rate, but metastasis is rare [14].
Radiological presentations are multilocular or unilocular radiolucency with well-defined borders. Maximum number of them are multilocular. Radiological investigations reveal homogenous radiolucency with well-defined borders which may appear differently like honeycomb, soap bubble, or tennis racket [10,15]. Radiological examination helps a lot in differential diagnosis of myxoma/fibromyxoma and between benign myxomas and malignant neoplasm with myxomatous tissue. In Magnetic Resonance Imaging (MRI), the lesion shows low - signal intensity in T1 and high signal is intensity in T2, in contrast, others advocate that the signal is shown in T1 and not in T2. These discrepancies may be related to the ratio of fibrous/myxoid tissue, the viscosity, the concentration of proteins, the presence of hemorrhage and hypocellularity. Immunochemical examination uses antibodies against specific biological substance of neuronal, muscular, epithelial, and mesenchymal tissue. The evaluation of the presence of the vimentin, and intermediate filament of the cyto skeleton characterizes, mesenchymal tissues, thus myxoma. Fibromyxoma also contain a high amount of hyaluronic acid. Coming to its histopathological aspect, the fusiform or stellate cells are elongated, having cytoplasmic process stretching in various directions. It contains few cells that lie in myxoid ground substance.
The tumor was not radiosensitive, and hence surgery was the only treatment of choice. The surgical treatment of fibromyxoma involves enucleation and curettage, radical excision, en bloc resection. Thoma has stated that recurrence of fibromyxoma is uncommon if enucleation is complete. Myxoma or fibromyxoma shows a recurrence rate between 25% and 43%. Harder et al. stated that rate of recurrence varies widely as does the choice of treatment. Their study support conservative surgery as the appropriate treatment of odontogenic myxoma, as they have found no evidence of malignant change or increasingly aggressive behavior in any of the recurrences [16].
Conclusion
At the end it can be concluded, that although maxilla is a rare location of fibromyxoma, various diagnostic regimen like C.T. and M.R.I along with the incisional biopsy plays a pivotal role in establishing the proper diagnosis as well as the differential diagnosis from other pathologies of the oral cavity like ameloblastoma. It is management, as described above involves mainly surgical approach which may include eneucleation and curettage to complete resection and peripheral ostectomy depending upon the size of pathology and the condition of the patients. In this young female as the extent of lesion is confined to the maxillary sinus, we have opted for an intraoral conservative surgical approach. Moreover, the patient should be kept under the follow up for about two years to check any recurrence of the lesion. Fibromyoma of the maxilla can be completely cured if correct diagnosis is made in right time followed by the proper treatment.
References
- Dietricsh EM, Papaemmanouil S, Koloutsos G, et al. Odontogenic fibromyxoma of the maxilla: A case report and review of the literature. Case Rep Med 2011; 2011:238712.
- L Lo Muzio, Nocini P, Favia G, et al. Odontogenic myxoma of the jaws: A clinical, radiologic, immunohistochemical, and ultrastructural study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996; 82:426-433.
- Aquilino RN, Tuji FM, Eid NL, et al. Odontogenic myxoma in the maxilla: a case report and characteristics on CT and MR. Oral Oncol Extra 2006; 42:133–136.
- James DR, Lucas VS. Maxillarymyxoma in a child of 11months-A case report. J Cranio Maxillofacial Surg 1987; 15:42-44.
- Berry S, Puri R. Fibromyxoma of the maxilla. Otolaryngology 2006; 135:330-331.
- Dutz W, Stout AP. The myxoma in childhood. Cancer 1961; 14:629-635.
- Marcove RC, Kambolis C, Bullough PG, et al. Fibromyoma of bone-A Report of 3 cases. Cancer 1964; 17:1209-1213.
- Simon ENM, Merkx MAW, Vuhahula E, et al. Odontogenicmyxoma: A clinicopathological study of 33 cases. Int J Oral Maxillofcial Surg 2004; 33:333-337.
- Kuhne CA, Engelhorn T, Homann M, et al. Fibromyxoma of the iliac wing, skeleton. Radiol 2003; 32:170-173.
- Abios BO, Ajagbe HA, Thomas O. Fibromyxoma of jaw bones-A study of ten cases. Br J Oral Maxillofacial Surg 1987; 25:415-421.
- Adamo AK, Locricchino RC, Freedman P. Myxoma of the mandible treated by peripheral osteotomy and immediate reconstruction-Report of a case. J Oral Surg 1980; 38:530-533.
- Shafer WG, Hine MK, Levy BM. Cysts and the tumors of odontogenic Origin. A textbook of oral pathology. 4th Edn, W.B. Saunders 1983; 295-297.
- Goldblatt LI. Ultrastructural Study of an odontogenic myxoma. Oral Surg 1976; 42:206-220.
- Adekeye EO, Avery BS, Edward MB, et al. Advanced central myxoma of the jaws of Nigeria. Int J Oral Surg 1984; 13:177-186.
- Shah A, Lone P, Latoo S, et al. Odontogenic myxoma of the maxilla of the maxilla: A report of a rare case and the review on histogenetic and diagnostic concepts. National J Maxillofacial Surg 2011; 2:189-195.
- Harder F. Myxomas of the jaws. Int J Oral Surg 1978; 7:148–155.
Author Info
Praveen Kumar Pandey*, Dipyaman Sen, Manish Kumar, Vikrant Kunwar, Neha Upadhyay and Chandan Kumar
Dept of Oral & Maxillofacial Surgery, Chandra Dental College and Hospital, IndiaCitation: Praveen Kumar Pandey, Dr Dipyaman Sen, Manish Kumar, Vikrant Kunwar, Neha Upadhyay, Chandan Kumar, Fibromyxoma of Maxilla–A Case Report of Rare Odontogenic Tumor, J Res Med Dent Sci, 2020, 8 (3):244-247.
Received: 20-Apr-2020 Accepted: 11-Jun-2020
