Research - (2021) Volume 9, Issue 1
Evaluation of the Difficulties Faced in Stage-2 Implant Procedure by Dental Practitioners
*Correspondence: Suresh V, Department of Prosthodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, India, Email:
Abstract
Oral implantology is a well-established subspecialty of restorative dental and oral surgery. Implant-supported restorations are considered as the main treatment of choice from the perspective of occlusal support, preservation of adjacent teeth, and avoidance of a removable partial denture. Even as major advances have occurred over the last few decades in the clinical use of implants making it a relatively simpler and chairside procedure, various complications have led to implant failure. The aim of this study is to evaluate the difficulties faced in stage-2 implant procedure by dental practitioners. A cross sectional questionnaire based study was carried out among dental practitioners in Chennai. A self-administered questionnaire was designed. The questionnaire consisted of questions regarding the difficulties dental practitioners faced during stage-2 implant procedure. The questionnaire was distributed through an online link to 50 dental practitioners. The data were collected and statistically analyzed using SPSS software. From the results, it is observed that the majority (72%) of the dental practitioners preferred to call an implant specialist for stage-2 procedure and various challenges the practitioners faced in stage-2 procedure were difficulty in locating cover screw (54%), bone loss (62%), implant stability (52%), achieving path of insertion (40%), and abutment screw loosening (46%) and over contoured crowns (54%). Thus it was observed that dental practitioners faced various difficulties in stage-2 implant procedure. These challenges can be overcome by correct selection of cases, knowledge on the risks and methods to avoid them with necessary information.
Keywords
Implant placement, Dental practitioners, Difficulties, Stage-2 implant procedure
Introduction
Dental implant is a surgical component that interfaces with the bone of the jaw or skull to support a dental prosthesis such as a crown, bridge, denture, facial prosthesis or to act as an orthodontic anchor [1]. The use of dental implants to provide support for replacement of missing teeth has a long and multifaceted history [2,3]. Oral implantology is a well-established subspecialty of restorative dental and oral surgery.
Tooth loss is very common and it can happen as a result of disease and trauma [4]. Loss of natural teeth is a health problem that is associated with functional, cosmetic, and psychological morbidities [5]. Various attempts have been made to replace the lost dentition with artificial teeth (prosthesis) that resemble the natural teeth in function and appearance. This solution is often achieved with dentures and fixed bridges. Today, implant-supported restorations can be considered the treatment of choice from the perspective of occlusal support, preservation of adjacent teeth, and avoidance of a removable partial denture [6]. Currently, dental implants are widely accepted as a prosthetic treatment of completely or partially edentulous patients. This led to widespread acceptance and popularity of dental implants within the dental professional community [7].
Implants may be placed penetrating the oral mucosa (1‐stage procedure) or can be completely buried under the oral mucosa (2‐ stage procedure) during the healing phase of the bone at the implant surface. A two-stage surgical protocol for implant placement has been the standard surgical technique for insertion of dental implants [8]. With a 2‐stage procedure the risk of having unwanted loading onto the implants is minimized, but a second minor surgical intervention is needed to connect the healing abutments and more time is needed prior to start the prosthetic phase because of the wound‐healing period required in relation to the second surgical intervention [9]. Many factors have been recognized as critical for the successful performance of the implants. One of the most important factors is degree of osseointegration [10,11]. In order to improve Osseo integration; Therefore long-term success of the implants, the following variables are critical and should be considered in the design of dental implants which includes biomaterials composition, implant width length and geometry, biomechanical factors, surface characteristics, medical status of the patient, bone quality and surgical technique [12,13].
Even as major advances have occurred over the last few decades in the clinical use of implants making it a relatively simpler and chairside procedure, various complications have led to implant failure. Implant complications can be broadly classified into surgical and prosthetic complications. These complications can mainly arise due to difficulties in implant placement, pre-operative and post-operative conditions of an individual [14]. Understanding the various difficulties in implant placement will help practitioners to develop better techniques to overcome these difficulties. Thus the aim of this study is to evaluate the difficulties faced in stage-2 implant procedure by dental practitioners.
Previously our department has published extensive research on various aspects of prosthetic dentistry [15-25], this vast research experience has inspired us to research about difficulties faced in stage-2 implant procedure by dental practitioners.
Materials and Methods
A cross sectional questionnaire based study was carried out among dental practitioners in Chennai. A self-administered questionnaire was designed. The first part of the questionnaire consisted of participants' details such as name, age and gender. The second portion consisted of questions regarding the difficulties they faced during stage-2 implant procedure. The questionnaire was distributed through an online link. The study population included 50 dental practitioners. Simple random sampling methodology was employed. The participants were explained about the purpose of the study. The questions were carefully studied and the corresponding answers were marked by them. The data were collected and statistically analyzed using SPSS software.
Results and Discussion
Out of 50 dental practitioners, 6 of them belonged to the age group of below 30 years, 19 belonged to the age group of 30-40 years, 17 belonged to the age group of 41-50 years and 8 belonged to the age group of above 50 years (Figure 1). 54% of the study population was males and 46% were females (Figure 2). Majority (72%) of the dental practitioners responded that they would call a specialist for stage-2 implant placement (Figure 3). 54% of the practitioners faced difficulty in locating cover screw (Figure 4) during stage-2 procedure while 70% of them did not face difficulty in placing healing abutments after retrieving healing screw (Figure 5). Only 18% of the practitioners did not find the size of healing abutment and collar of implant matching while majority (82%) found the size to be matching (Figure 6). 36% of the practitioners responded that they would wait for 2 weeks post placement of healing abutment for impression procedure, while 24% waited for 3 weeks and 28% waited for 4 weeks (Figure 7). Majority (62%) of the practitioners found bone loss during stage-2 procedure (Figure 8) and 52% of them responded that they would re-verify implant stability during stage-2 while 48% responded they did not re-verify implant stability (Figure 9). 50% of the practitioners used straight abutment with snappy, 22% used straight abutment only, 20% used open tray impression coping and 8% used closed tray impression coping for implant impression procedure (Figure 10). Majority (68%) of the dental practitioners did jig verification in stage-2 procedure (Figure 11). 40% of the practitioners often faced difficulty in achieving a path of insertion for implant prosthesis (Figure 12) and 46% of them often experienced abutment screw loosening (Figure 13). Majority (54%) of the dental practitioners found over contoured crowns at gingival contour region (Figure 14).
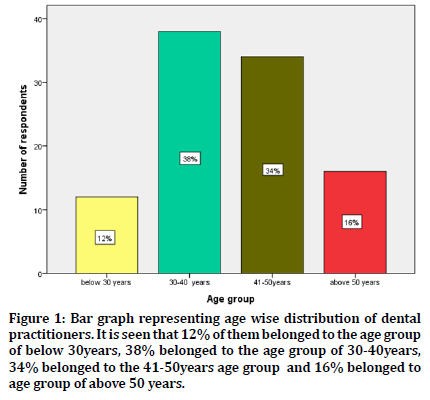
Figure 1. Bar graph representing age wise distribution of dental practitioners. It is seen that 12% of them belonged to the age group of below 30years, 38% belonged to the age group of 30-40years, 34% belonged to the 41-50years age group and 16% belonged to age group of above 50 years.
Figure 2. Bar graph representing gender distribution of dental practitioners. It is seen that 54% of them were males and 46% were females.
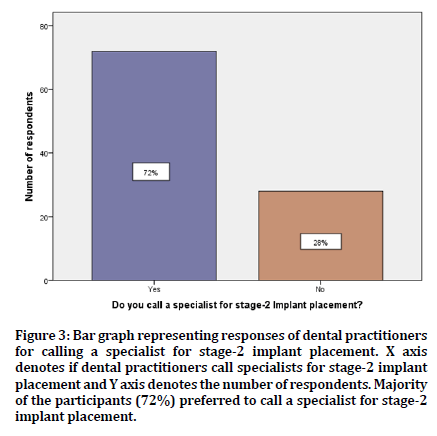
Figure 3. Bar graph representing responses of dental practitioners for calling a specialist for stage-2 implant placement. X axis denotes if dental practitioners call specialists for stage-2 implant placement and Y axis denotes the number of respondents. Majority of the participants (72%) preferred to call a specialist for stage-2 implant placement.
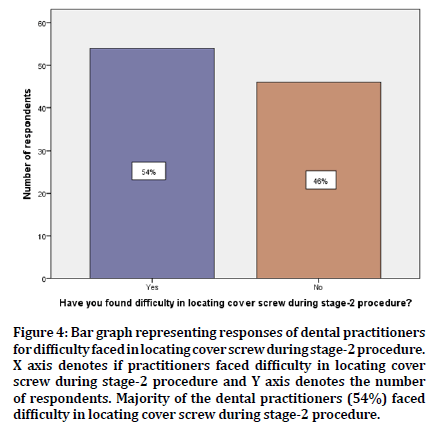
Figure 4. Bar graph representing responses of dental practitioners for difficulty faced in locating cover screw during stage-2 procedure. X axis denotes if practitioners faced difficulty in locating cover screw during stage-2 procedure and Y axis denotes the number of respondents. Majority of the dental practitioners (54%) faced difficulty in locating cover screw during stage-2 procedure.
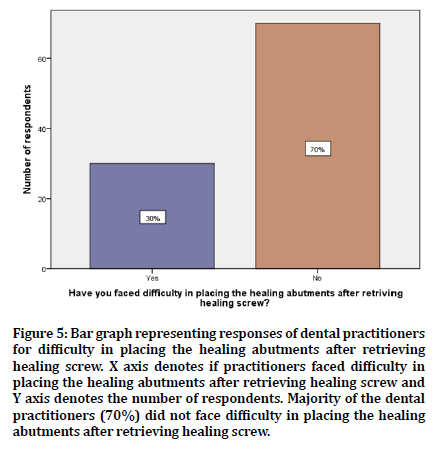
Figure 5. Bar graph representing responses of dental practitioners for difficulty in placing the healing abutments after retrieving healing screw. X axis denotes if practitioners faced difficulty in placing the healing abutments after retrieving healing screw and Y axis denotes the number of respondents. Majority of the dental practitioners (70%) did not face difficulty in placing the healing abutments after retrieving healing screw.
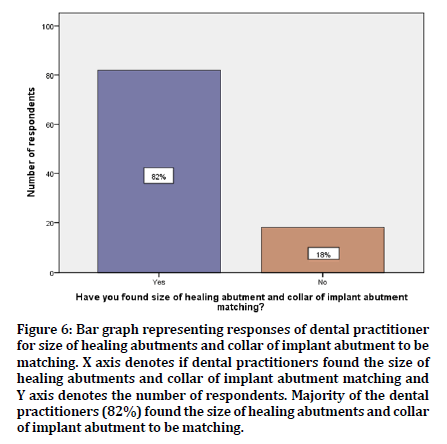
Figure 6. Bar graph representing responses of dental practitioner for size of healing abutments and collar of implant abutment to be matching. X axis denotes if dental practitioners found the size of healing abutments and collar of implant abutment matching and Y axis denotes the number of respondents. Majority of the dental practitioners (82%) found the size of healing abutments and collar of implant abutment to be matching.
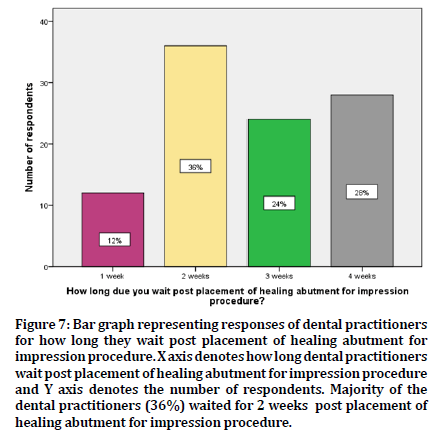
Figure 7. Bar graph representing responses of dental practitioners for how long they wait post placement of healing abutment for impression procedure. X axis denotes how long dental practitioners wait post placement of healing abutment for impression procedure and Y axis denotes the number of respondents. Majority of the dental practitioners (36%) waited for 2 weeks post placement of healing abutment for impression procedure.
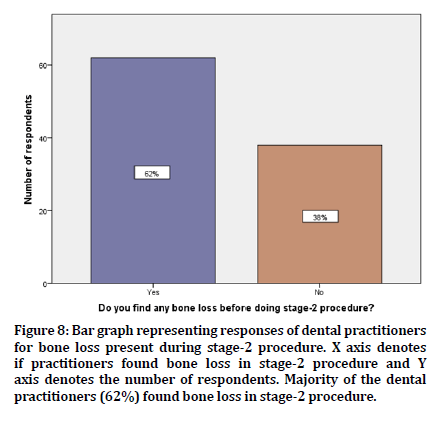
Figure 8. Bar graph representing responses of dental practitioners for bone loss present during stage-2 procedure. X axis denotes if practitioners found bone loss in stage-2 procedure and Y axis denotes the number of respondents. Majority of the dental practitioners (62%) found bone loss in stage-2 procedure.
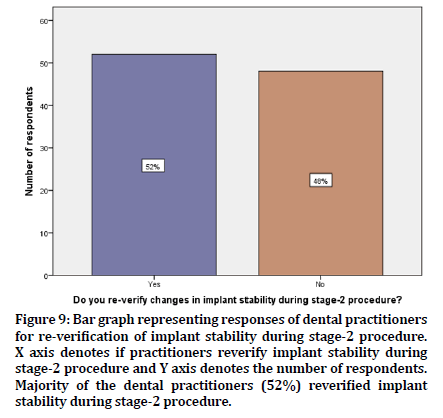
Figure 9. Bar graph representing responses of dental practitioners for re-verification of implant stability during stage-2 procedure. X axis denotes if practitioners reverify implant stability during stage-2 procedure and Y axis denotes the number of respondents. Majority of the dental practitioners (52%) reverified implant stability during stage-2 procedure.
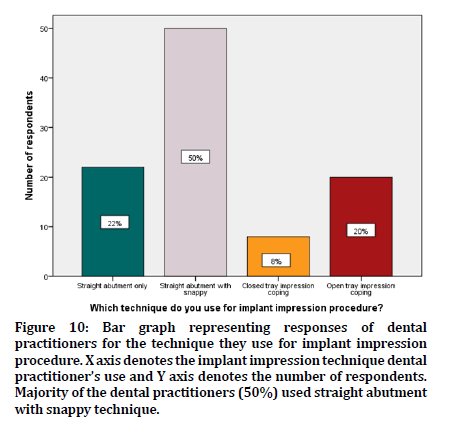
Figure 10. Bar graph representing responses of dental practitioners for the technique they use for implant impression procedure. X axis denotes the implant impression technique dental practitioner’s use and Y axis denotes the number of respondents. Majority of the dental practitioners (50%) used straight abutment with snappy technique.
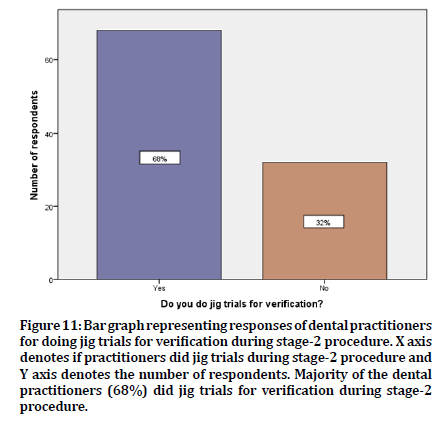
Figure 11. Bar graph representing responses of dental practitioners for doing jig trials for verification during stage-2 procedure. X axis denotes if practitioners did jig trials during stage-2 procedure and Y axis denotes the number of respondents. Majority of the dental practitioners (68%) did jig trials for verification during stage-2 procedure.
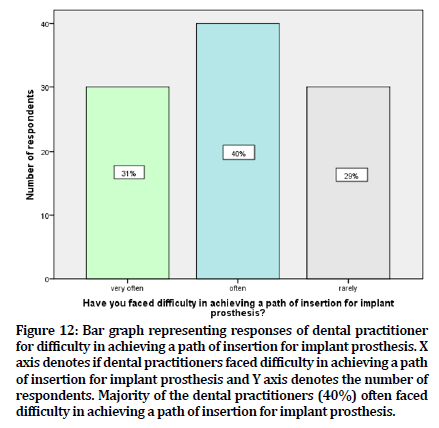
Figure 12. Bar graph representing responses of dental practitioner for difficulty in achieving a path of insertion for implant prosthesis. X axis denotes if dental practitioners faced difficulty in achieving a path of insertion for implant prosthesis and Y axis denotes the number of respondents. Majority of the dental practitioners (40%) often faced difficulty in achieving a path of insertion for implant prosthesis.
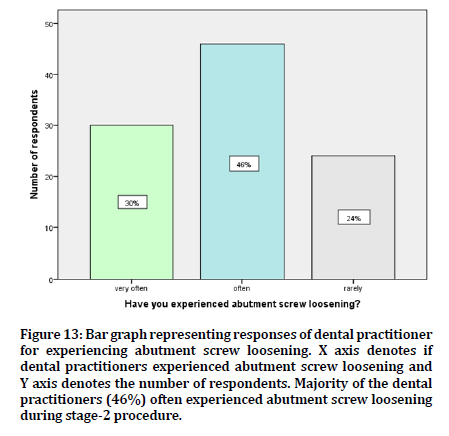
Figure 13. Bar graph representing responses of dental practitioner for experiencing abutment screw loosening. X axis denotes if dental practitioners experienced abutment screw loosening and Y axis denotes the number of respondents. Majority of the dental practitioners (46%) often experienced abutment screw loosening during stage-2 procedure.
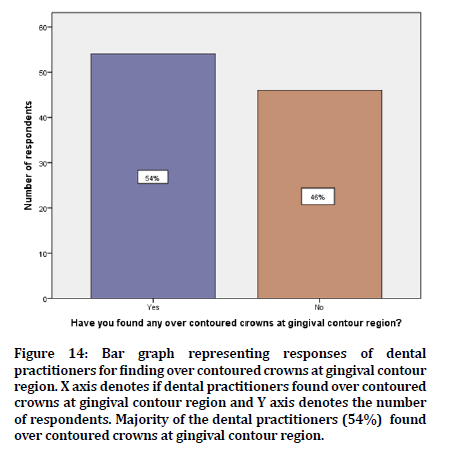
Figure 14. Bar graph representing responses of dental practitioners for finding over contoured crowns at gingival contour region. X axis denotes if dental practitioners found over contoured crowns at gingival contour region and Y axis denotes the number of respondents. Majority of the dental practitioners (54%) found over contoured crowns at gingival contour region.
From the results, it is observed that the majority of the dental practitioners preferred to call an implant specialist for stage-2 procedure. Various challenges the practitioners faced in stage-2 procedure was difficulty in locating cover screw, bone loss, implant stability, achieving path of insertion, abutment screw loosening and over contoured crowns.
Majority of the dental practitioners in this study faced difficulty in location of the cover screw and managed to find it by flap elevation. Tarnow et al stated is his study that full or partial thickness flap is raised to establish access to cover screw [26]. Osseous recontouring followed by placement of healing abutments will be done. But the technique included some disadvantages like it caused more tissue manipulation leading to trauma involved and exposure of a large area of the bone. Worthington et al reported that bleeding as a result of improper flap elevation made locating the cover screw more difficult [27].
Ericsson et al noted in his study that bone loss was more in 2stage implant technique [28] while few authors stated that no bone loss was observed in stage-2 procedure which could be due to the careful selection of the patients, good quality of bone, and performing the surgery under standard conditions [29,30]. Jeong et al. and Block et al. stated that bone loss is a common problem observed during implant procedure which occurs mainly due to direct trauma to the bone reducing vascularity, decreased bone density, improper inclination of the implant, excessive torque during insertion, presence of a bone dehiscence not treated at phase I surgery and postoperative infection [31,32].
Majority of the practitioners in the present study did reverify implant stability in stage-2 procedure. Implant stability is of utmost importance for Osseo integration. Without it, long-term success cannot be achieved. Continuous monitoring in a quantitative and objective manner is important to determine the status of implant stability [33]. Meenakshi et al. stated that implant stability measurements can be used to document the clinical outcome of implant treatments, which can be useful at a later stage if a problem arises [34].
Another difficulty faced by practitioners in this study is abutment screw loosening while only few of them found the size of healing abutment and collar of implant not matching. Jemt et al. and Binon et al. reported that abutment screw loosening is the second most common cause of failure of implant supported restoration, next to loss of osseointegration seen commonly in single implant supported restoration [35,36]. Reasons for screw loosening include inadequate preload, inappropriate implant position, variations in hex dimension and abutment counterparts, differences in fit and accuracy, improper screw design and excessive occlusal forces [37-39].
Dental practitioners also faced difficulties in achieving proper path of insertion for the implant prosthesis. Authors state that increase in angulation of implants is the main reason causing difficulty in achieving path of insertion and this is commonly encountered when multiple implants are placed in a patient [40,41]. In order to overcome this, parallelism of implants must be maintained and jig verification must be done. In this study population, majority of the practitioners did perform jig verification in stage2 procedure. Also proper impression technique must be followed for implant impression procedure to ensure proper fit of final restoration to prevent over contoured crowns at gingival margin which is also one of the difficulties practitioners faced. Straight abutment with snappy impression technique and open impression techniques were most preferred among the dental practitioners in this study. Studies observed that open tray technique exhibited more accuracy compared to the closed tray technique [42,43]. Since the impression coping remains in the impression, the open tray technique reduces the effect of implant angulation, deforming the impression material upon recovery from mouth, and removes the concern of replacing the copings into the impression [44].
Implant treatment is regarded as a safe technique with high rates of success. Nevertheless, the procedures possess various challenges to practitioners and knowledge on the difficulties is essential to prevent and manage the same. This study could pave way for further research to be done on the challenges faced and methods to overcome these challenges in order to improve the success of implant treatment. The limitation of this study is limited study sample.
Conclusion
Various challenges faced by practitioners in stage-2 procedure were difficulty in locating cover screw, bone loss, implant stability, achieving path of insertion, abutment screw loosening and over contoured crowns. These challenges can be overcome by correct selection of cases, knowledge on the risks and methods to avoid them with necessary information. Detailed case evaluation and treatment planning are desirable for a successful implant supported prosthesis.
Acknowledgment
I sincerely thank Saveetha Dental College for extending full support for this study.
Conflict of Interest
Nil.
References
- Misch CE. Rationale for dental implants. Text book on dental implant prosthetics; Misch, CE, Ed.; Elsevier Publ.: Amsterdam, The Netherlands. 2014; 3:1-7.
- Elias CN. Factors affecting the success of dental implants. Implant dentistry: A rapidly evolving practice. Rijeka: In Tech 2011; 29:319-364.
- Hupp JR. Oral Facial jaw mouth cosmetic implant surgeons—What's in a name? J Oral Maxillofac Surg 2014; 72:1437-1440.
- Kademani D, Bell RB, Schmidt BL, et al. Oral and maxillofacial surgeons treating oral cancer: A preliminary report from the American association of oral and maxillofacial surgeons task force on oral cancer. J Oral Maxillofac Surg 2008; 66:2151-2157.
- Mgbeokwere U, Okoye L, Ekwueme O. A survey of the knowledge of dental implants as a choice in treatment of edentulous jaws among health workers in government dental clinics in Enugu. Ann Med Health Sci Res 2011; 1:91-96.
- Mukatash GN, Al-Rousan M, Al-Sakarna B. Needs and demands of prosthetic treatment among two groups of individuals. Indian J Dent Res 2010; 21:564.
- Faegh S, Chou HY, Müftu S. Load transfer along the bone-implant interface and its effects on bone maintenance. Dental implants: A rapidly evolving practice. Rijeka Croatia: In Tech Publishing 2011; 29:163-190.
- Liddell R, Ajami E, Davies JE. Tau (τ): A new parameter to assess the osseointegration potential of an implant surface. Int J Oral Maxillofac Implants 2017; 32.
- Ghadiri M, Shafiei N, Salekdeh SH, et al. Investigation of the dental implant geometry effect on stress distribution at dental implant–bone interface. J Braz Soc Mech Sci Eng 2016; 38:335-343.
- Bahat O, Sullivan RM. Parameters for successful implant integration revisited part I: Immediate loading considered in light of the original prerequisites for osseointegration. Clin Implant Dent Relat Res 2010; 12:e2-e12.
- Triplett RG, Frohberg U, Sykaras N, et al. Implant materials, design, and surface topographies: Their influence on osseointegration of dental implants. J Long Term Eff Med Implants 2003; 13.
- Le Guéhennec L, Soueidan A, Layrolle P, et al. Surface treatments of titanium dental implants for rapid osseointegration. Dent Mater J 2007; 23:844-854.
- Javed F, Ahmed HB, Crespi R, et al. Role of primary stability for successful osseointegration of dental implants: Factors of influence and evaluation. Interv Med Appl Sci 2013; 5:162-167.
- Spear FM, Kokich VG, Mathews DP. Interdisciplinary management of anterior dental esthetics. J Am Dent Assoc 2006; 137:160-169.
- Begum R, Ariga P, Jain AR. Evaluation of corrosive behavior of four nickel–chromium alloys in artificial saliva by cyclic polarization test: An in vitro study. World J Dent 2017; 8:477-482.
- Kannan A. Effect of coated surfaces influencing screw loosening in implants: A systematic review and meta-analysis. World 2017; 8:496-502.
- Ariga P, Narayanan V, Jain AR, et al. Clinical and functional outcomes of implant prostheses in fibula free flaps. World J Dent 2017; 8:171-176.
- Ashraf J, Jain AR, Ariga P, et al. Prevalence of partial edentulousness and treatment needs in rural population of South India. World J Dent 2017; 8:213-217.
- Ranganathan H, Ganapathy DM, Jain AR. Cervical and incisal marginal discrepancy in ceramic laminate veneering materials: A SEM analysis. Contemp Clin Dent 2017; 8:272.
- Jain AR, Nallaswamy D, Ariga P, et al. Determination of correlation of width of maxillary anterior teeth using extraoral and intraoral factors in Indian population: A systematic review. World J Dent 2018; 9:68-75.
- Gupta P, Ariga P, Deogade SC. Effect of monopoly-coating agent on the surface roughness of a tissue conditioner subjected to cleansing and disinfection: A contact profilometric In vitro study. Contemp Clin Dent 2018; 9:S122.
- Anbu RT, Suresh V, Gounder R, et al. Comparison of the efficacy of three different bone regeneration materials: An animal study. Eur J Dent 2019; 13:22.
- Ashok V, Ganapathy D. A geometrical method to classify face forms. J Oral Biol Craniofac Res 2019; 9:232-235.
- Duraisamy R, Krishnan CS, Ramasubramanian H, et al. Compatibility of nonoriginal abutments with implants: Evaluation of microgap at the implant: Abutment interface, with original and nonoriginal abutments. Implant Dent 2019; 28:289-295.
- Varghese SS, Ramesh A, Veeraiyan DN. Blended module‐based teaching in biostatistics and research methodology: A retrospective study with postgraduate dental students. J Dent Educ 2019; 83:445-450.
- Tarnow DP, Eskow RN, Zamzok J. Aesthetics and implant dentistry. J Periodontol 1996; 11:85-94.
- Worthington P. Osseointegration in dentistry. An Overview 2003.
- Ericsson L, Randow K, Nilner K, et al. Some clinical and radiographical features of submerged and non‐submerged titanium implants. A 5‐year follow‐up study. Clin Oral Implants Res 1997; 8:422-426.
- Siadat H, Panjnoosh M, Alikhasi M, et al. Does implant staging choice affect crestal bone loss? J Oral Maxillofac Surg 2012; 70:307-313.
- Engquist B, Åstrand P, Anzén B, et al. Simplified methods of implant treatment in the edentulous lower jaw. A controlled prospective study. Part I: One‐stage versus two‐stage surgery. Clin Implant Dent Relat Res 2002; 4:93-103.
- Jeong SM, Choi BH, Li J, et al. Bone healing around implants following flap and mini-flap surgeries: a radiographic evaluation between stage I and stage II surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 105:293-296.
- Block MS, Kent JN. Factors associated with soft-and hard-tissue compromise of endosseous implants. J Oral Maxillofac Surg 1990; 48:1153-1160.
- O'Sullivan D, Sennerby L, Jagger D, et al. A comparison of two methods of enhancing implant primary stability. Clin Implant Dent Relat Res 2004; 6:48-57.
- Meenakshi S, Raghunath N, Gujjari AK. Implant hygiene and soft tissue management: Dentist's perspective. Int J Allied Health Sci 2013; 2:159.
- Jemt T, Lindén B, Lekholm U. Failures and complications in 127 consecutively placed fixed partial prostheses supported by brånemark implants: From prosthetic treatment to first annual checkup. Int J Oral Maxillofac Implants 1992; 7.
- Michalakis KX, Calvani PL, Muftu S, et al. The effect of different implant-abutment connections on screw joint stability. J Oral Implantol 2014; 40:146-152.
- Artzi Z, Dreiangel A. A screw lock for single-tooth implant superstructures. J Am Dent Assoc 1999; 130:677-802.
- Schwarz MS. Mechanical complications of dental implants. Clin Oral Implants Res 2000; 11:156-158.
- Cavazos E, Bell FA. Preventing loosening of implant abutment screws. J Prosthet Dent 1996; 75:566-569.
- Scherer MD, McGlumphy EA, Seghi RR, et al. Comparison of retention and stability of implant-retained overdentures based upon implant number and distribution. Int J Oral Maxillofac Implants 2013; 28:1619-1628.
- Stephens GJ, di Vitale N, O'Sullivan E, et al. The influence of interimplant divergence on the retention characteristics of locator attachments, a laboratory study. J Prosthodont 2014; 23:467-475.
- Mpikos P, Tortopidis D, Galanis C, et al. The effect of impression technique and implant angulation on the impression accuracy of external-and internal-connection implants. Int J Oral Maxillofac Implants 2012; 27.
- Shankar YR, Sahoo S, Krishna MH, et al. Accuracy of implant impressions using various impression techniques and impression materials. Implant Dent 2016; 6:29.
- Howell KJ. Comparison of the accuracy of biomet 3i encode robocast technology and conventional implant impression techniques. Int J Oral Maxillofac Implants 2011; 28:228–240.
Author Info
Department of Prosthodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, Tamilnadu, IndiaCitation: Faazila Fathima, Suresh V, Evaluation of the Difficulties Faced in Stage-2 Implant Procedure by Dental Practitioners, J Res Med Dent Sci, 2021, 9 (1): 358-365.
Received: 23-Sep-2020 Accepted: 11-Jan-2021
