Research - (2022) Volume 10, Issue 9
Evaluation of Sustainability of Mechanical Properties of Various Suture Materials Used in Periodontal Surgeries-An In Vivo Study
Bhavana Garapati* and Thamaraiselvan Murugan
*Correspondence: Bhavana Garapati, Department of Periodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical sciences (SIMATS), Saveetha University, Chennai, India, Email:
Abstract
Background: Mechanical properties of suture materials play an important role in clinical outcomes of periodontal surgery, thus any changes in these properties might influence the surgical wound healing. As there are various factors that can alter the physical and mechanical properties of suture materials when present in the oral cavity, sustainability of the properties is of much importance. Aim: The aim of this study is to compare the sustainability of tensile strength of Polytetrafluoroethylene (PTFE) and Polyamide suture materials in patients undergoing periodontal flap surgery. Material and methods: A total of fourteen subjects who were indicated for surgical periodontal pocket management were included in this study. After Random allocation, Group1- Polyamide, Group 2- PTFE sutures were used. The Tensile strength of suture material was evaluated before and after surgery. Result: The baseline tensile strength was 2.10 ± 1.72 kgf.cm² and 5.70 ±1.76gf.cm² for polyamide and PTFE respectively. One week post-surgery it got reduced to 9.723 kgf.cm² and 7.036 kgf.cm² which were statistically significant within the group. However there was no statistically significant difference when compared between the groups. Conclusion: From our results it is wise to conclude that both PTFE and Polyamide have not retained their tensile strength and thus did not sustain throughout the healing period. Since the reduction in tensile strength of PTFE was minimal, it can be the material of choice for periodontal surgeries involving longer healing periods.
Keywords
Tensile strength, Sustainability, Suture material
Introduction
Primary wound healing is the ultimate expected outcome of any surgical procedure. To achieve primary wound healing in surgical Traumatised areas sutures to play a role. The goals of suturing include obliteration of dead space, even distribution of tension along deep suture lines, and maintenance of tensile strength across the wound until tissue tensile strength is adequate [1].
Conventional periodontal surgery aimed at reduction of periodontal pockets results in repair of periodontal tissues that no longer mimic the normal architecture of the healthy periodontium. Periodontal regeneration is, however, a wound healing process that reproduces all the lost structure of the periodontium, namely alveolar bone, cementum, periodontal ligament and gingiva. Although wound healing at the tooth-gingiva interface follows the same principles as in the skin or palatal mucosa, In periodontal healing, the fibrin-fibronectin clot needs to be stabilized on a mechanically debrided root surface. This stabilization often fails leading to migration of the epithelium along the root surface, leading to formation of long junctional epithelium instead of regeneration [2]. Thus, Adequate wound care, perfect flap approximation and more importantly, stabilization of the flaps during the postoperative healing are extremely important for achieving good results following periodontal surgeries. This stabilization can be influenced by suture materials.
Use of suture materials for wound closure is an ancient art where Hippocrates of ancient Greece in 460- 370 BCE used wool boiled in water or wine as a bandage [3]. Use of animal hair, vegetable fibers, silk, leather, and gut have all been shown to be successfully used in wound closure [4]. 1600 BC: Linen strips soaked in oil or grease and covered with plaster used to occlude wounds.–“Closed wounds heal more quickly than open wounds”–Edwin Smith.–1891: First woven absorbent cotton gauze. A suture material can be either natural or synthetic which is used to ligate blood vessels and approximate tissues together.
A range of sutures are available that are classified by several criteria: 1. Composition—natural and synthetic; 2. structure—monofilament and multifilament; and 3. spontaneous degradation—absorbable and non- absorbable [5]. The suture materials currently in application for oral and periodontal procedures are Silk, prolene, polyamide, catgut, chromic gut, vicryl, polyglyconate, polyglecaprone etc. For various procedures such as periodontal plastic, cosmetic and reconstructive procedures, selection of appropriate suture techniques, thread type, thread diameter and surgical needle is of paramount importance. From the numerous materials available the choice of suture material for a particular procedure is dependent on the various mechanical properties of the material, like tensile strength, modulus of elasticity, knot stability etc. [6]. These physical & mechanical properties of a suture material play a significant role in influencing the surgical wound healing outcomes. There is no best suture material of choice satisfying all mechanical and physical properties for a surgeon. Deficiency in the strength of the suture material can result in untimely suture breakage, leading to poor adaptation of the surgical flaps and inducing the healing of tissues by secondary intention [7-9].
Apart from various other properties mentioned above, there are factors that influence the suturing in the oral cavity. The suturing differs from other areas of the body due to the type of tissues involved, the permanent presence of saliva, high tissue vascularization, speech- related functions, mastication, and swallowing. There is need for proper suture material which has greater tensile strength to approximate the flaps for a longer time with tensile strengths sustained till the complete wound closure and healing occur. As there are various factors which can alter the physical and mechanical properties of suture materials when present in the oral cavity, sustainability of the properties is of much importance. The null hypothesis of this study is that there would not be much difference between both the groups at 1 week post op. The alternative hypothesis is that there might be some difference in the mechanical properties between both the groups at 1 week.
To the best of our knowledge, this is the first study focusing on the sustainability of the tensile strengths of two non-absorbable monofilament suture materials in the oral cavity. Hence, the aim of this study was to evaluate the sustainability of mechanical properties of two non-absorbable monofilament sutures.
Material and Methods
Study design
The study design includes a parallelized controlled clinical trial for which the study subjects were recruited from the patients reporting to the Out-patient department of periodontics, with the following inclusion and exclusion criteria.
Inclusion criteria
Age >18 years
• Systematically healthy.
• Subjects willing to give consent form.
• Patients diagnosed with Periodontitis having pockets in at least 1 or more areas who are indicated for periodontal flap surgery for pocket management.
Exclusion criteria
• Smoking more than 10 cigarettes per day.
• Contraindications for periodontal surgery.
• Taking medications known to interfere with periodontal tissue health and healing.
• Previous periodontal surgery.
After clearance from the Institutional Ethical Committee, a total of fourteen subjects satisfied the inclusion and exclusion criteria, who were explained about the purpose, risks, benefits, of the procedures and the study and after obtaining the informed consent the subjects were finally included in the study. The age of the study population ranged from 20 - 45 years, in which 8 were males and 6 were females, indicated for periodontal flap surgery. The study subjects were then allocated to one of the two study groups.
Study group
Group I: Periodontitis with 5-0 Polyamide suture (Ethicon®) (control group).
Group II: Periodontitis with 4-0 PTFE suture [GOLNIT®] (Test group).
Subjects in both the groups were initiated with phase I periodontal therapy which included complete scaling and root planing. Complete oral-hygiene instructions were advised. The periodontal flap surgery was planned 3 weeks after the phase I therapy if adequate oral hygiene was seen during re-evaluation. The tensile strength was measured prior to Surgery (baseline) and during follow- up (7th day).
Assessment of sustainability
Baseline assessment
One inch of the suture material before suturing the site was cut and used as a baseline sample for the assessing tensile strength.
Surgical procedure and postoperative protocol
All surgeries were performed by the same periodontist and the same suturing technique (continuous sling) was used in all the cases, under total asepsis and adequate local anesthesia (Lignocaine-1:200000) at the surgical site. After mechanical debridement, the flap was approximated using continuous sling suturing technique with surgeons knot in both the groups. In the control group were given Polyamide sutures and the test group were given Polytetrafluoroethylene (PTFE) sutures. Postoperatively, patients were instructed to take analgesic (Aceclofenac 100mg, BID, as needed for pain), use antimicrobial rinse (0.12% chlorhexidine, twice daily for 2 weeks) for plaque control, and avoid any mechanical plaque control for 2 weeks. Sutures were removed at 7 days postoperatively. The removed suture material was transported to the lab in Ringers Lactate (RL) solution.
Mechanical testing method
Each sample was prepared with an acrylic knob holding the material in the form of a knot and this is placed around two metal poles installed in the Universal Testing Machine (INSTRON E 3000 UTM at a crosshead speed of 10mm/unit - Instron Industrial Products, 900 Liberty Street, Grove City, PA 16127, USA) with a fixed distance of 15.0 mm between the two poles. The tensile strengths of the suture samples were tested at specific times: baseline and post-treatment suture removal on 7th day. The study was carried out in a heavy duty testing lab in Saveetha dental college that is specialized in evaluating tensile strengths. Tensile strength (TS) was measured on a tensile meter in a unit of Newton (N) in the universal testing machine. TS is the force applied per unit original cross-sectional area, to a test specimen at any given time. Each sample was stretched until the material failed, and the maximum load was recorded in Newtons (N).
Statistical analysis
The statistical analysis was performed with the SPSS 12.0 software. First, the univariate analysis was carried out by measuring the central tendency (arithmetic mean) and the measure of dispersion (standard deviation) of the variable tensile strength of the suture materials (PG, BS, and PTFE). The statistical assumptions of normality and homoscedasticity were then explored using the Shapiro–Wilk test. Finally, the bivariate analysis was performed using the Mann-Whitney and Independent-t tests depending on the values obtained in the previous analysis. Finally, statistical significance achieved was p=0.057.
Results
When analyzing the descriptive statistics, it was found that in relation to both the groups, the average tensile strength was stable between baseline and 1 week post-operative. When making the inference with the Mann-Whitney test, showed that there was statistically significant difference between both groups at 1 week post-operative. Where PTFE had higher sustainability over Polyamide over time (Table 1 and Figures 1 and Figure 2).
| S.no | Mean tensile strength (%) at baseline | Mean tensile strength (%) at 1 week | Standard deviation | Significance (P value) |
|---|---|---|---|---|
| Group 1 | 2.1 | 4.35 | 1.72222 | 0.056 |
| Group 2 | 5.7 | 6.31 | 1.76822 | 0.052 |
| P-value | 0.02 | 0.057 | - | - |
Table 1: Values at 1 week post-OP.
Figure 1: The above picture indicates the measurement of tensile strength of PTFE suture material at 1 week post operatively using Universal Testing Machine.
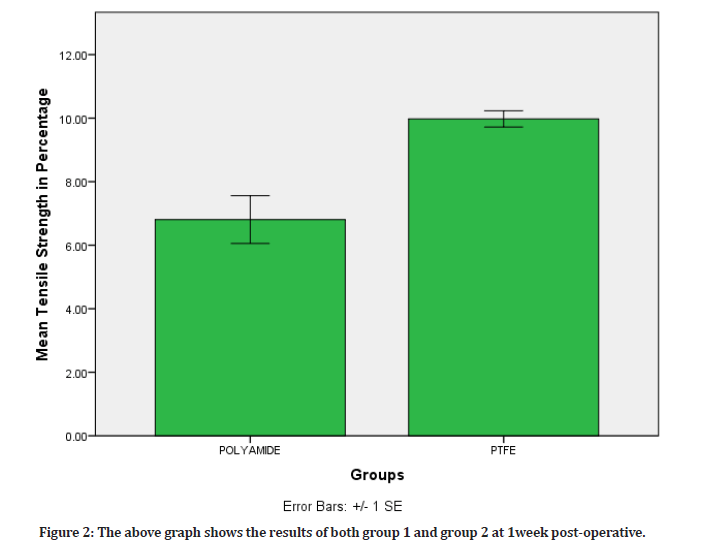
Figure 2: The above graph shows the results of both group 1 and group 2 at 1week post-operative.
Discussion
Despite decades of research on wound closure biomaterials, no suture material has completely satisfied all the ideal requirements for a particular clinical situation. When choosing the suture for wound closure, factors like tissue characteristics, Tensile Strength, reaction rate, absorption rates and handling properties are to be considered [10]. As the available evidence regarding the influence of these characteristics on wound healing is inconclusive, more research is needed to select the most appropriate suture material for each clinical scenario. Thus, this invivo study was designed to evaluate the sustainability of mechanical properties of two suture materials when exposed to oral cavity.
In our study, the tensile strength of polyamide at baseline was 2.10 ±1.72 kgf.cm2 which was contradicting to Gonalez, et al. study [11] where the tensile strength was 16.9 ± 3.3. At 1 week postoperatively, mean tensile strength of our samples was 4.35 kgf.cm. Since, there are no studies reporting the sustainability of polyamide invivo, we are unable to compare our results. The results of our study show that there is an increase in the tensile strength of polyamide after 1 week. Thus polyamide can help in holding the tissues together for a longer time thereby helping in proper wound healing.
Whereas the other material in our study, i.e, PTFE had initial baseline tensile strength of 5.70±1.76gf.cm² and got increased to a mean tensile strength of 6.3186 kgf. cm2 after 1 week postoperatively. These results were in accordance with Arce et al, where the tensile strength of PTFE had shown a marginal increase from baseline (7.52 ± 0.94) to 1 week post op (7.84 ± 0.26). Similar to polyamide, PTFE had also retained tensile strength.
When compared between the groups there was a statistically significant difference where PTFE was showing higher sustainability than polyamide. Previous reports comparing polyglactin, black silk and PTFE had shown no significant difference in reduction in tensile strength at 3, 7, 14, 21 days. This is further supported by an in vitro study where e-PTFE had shown to retain the tensile strength compared to silk and polyamide [11-14].
In both the groups, the change in tensile strength could be influenced by many factors. Firstly, the oral environment has a permanent presence of saliva, gingival crevicular fluid, high tissue vascularization which comes in direct contact with the sutures that may alter the physical properties of the suture material in turn altering the tensile strength. In addition it is also subjected to mechanical manipulations during speech- related functions, mastication, and swallowing. Secondly, during the process of suturing, the suture thread might be subjected to some physical damage from the handling of the material which might negatively influence the tensile strength of the suture; however, surprisingly our results show an increase in tensile strength of both the materials at 1 week irrespective of the physical and mechanical handling. Thus, both the materials have shown to sustain the properties that can positively influence the wound healing.
This is the first study done comparing the tensile strength of non-absorbable monofilament suture materials in the oral cavity. However, in our study limitations include smaller sample size, tensile strength measured on only 7th postoperative day, single property was evaluated and only surgeon's knot was used and there is no standardized method till date to evaluate the tensile strength which might in turn influence the results. Further research is needed with a larger sample size keeping in mind the other factors responsible for tensile strength degradation. Other mechanical properties can also be included for further confirmation of our results [15-25].
Conclusion
From our results it is wise to conclude that both PTFE and Polyamide have retained their tensile strength and PTFE did sustain better properties throughout the healing period. Hence, PTFE sutures can be the material of choice for periodontal surgeries involving longer healing periods.
References
- Pillai CKS, Sharma CP. Absorbable polymeric surgical sutures: Chemistry, production, properties, biodegradability, and performance. J Biomater Appl 2010; 25:291–366.
- Wikesjö UM, Nilvéus RE, Selvig KA. Significance of early healing events on periodontal repair: A review. J Periodontol 1992; 63:158–165.
- Daunton C, Kothari S, Smith L, et al. A history of materials and practices for wound management. J Australian Wound Manage Assoc 2012; 20.
- Parell GJ, Joseph Parell G, et al. Comparison of absorbable with nonabsorbable sutures in closure of facial skin wounds. Arch Facial Plastic Surg 2003; 5:488–490.
- Kim JC, Lee YK, Lim BS, et al. Comparison of tensile and knot security properties of surgical sutures. J Mater Sci Mater Med 2007; 18:2363–2369.
- Cohen ES. Atlas of cosmetic and reconstructive periodontal surgery. PMPH-USA 2007.
- Hiatt WH, Stallard RE, Butler ED, et al. Repair following mucoperiosteal flap surgery with full gingival retention. J Periodontol 1968; 39:11–16.
- Vasanthan A, Satheesh K, Hoopes W, et al. Comparing suture strengths for clinical applications: A novel in vitro study. J Periodontol 2009; 80:618–624.
- Burkhardt R, Lang NP. Coverage of localized gingival recessions: Comparison of micro and macrosurgical techniques. J Clin Periodontol 2005; 32:287–293.
- Greenberg JA, Clark RM. Advances in suture material for obstetric and gynecologic surgery. Rev Obstet Gynecol 2009; 2:146–158.
- González-Barnadas A, Camps-Font O, Espanya-Grifoll D, et al. In vitro tensile strength study on suturing technique and material. J Oral Implantol 2017; 43:169–174.
- Abullais SS, Alqahtani NA, Alkhulban RM, et al. In-vitro evaluation of commonly used beverages on tensile strength of different suture materials used in dental surgeries. Medicine 2020; 99:e19831.
- Arce J, Palacios A, Alvítez-Temoche D, et al. Tensile strength of novel nonabsorbable PTFE (Teflon®) versus other suture materials: An in vitro study. Int J Dent 2019; 2019:1–5.
- Taysi AE, Ercal P, Sismanoglu S. Comparison between tensile characteristics of various suture materials with two suture techniques: An in vitro study. Clin Oral Investig 2021; 25:6393–6401.
- Abellán D, Nart J, Pascual A, et al. Physical and mechanical evaluation of five suture materials on three knot configurations: An In vitro study. Polymers 2016; 8:147.’
- Obermeier A, Schneider J, Harrasser N, et al. Viable adhered Staphylococcus aureus highly reduced on novel antimicrobial sutures using chlorhexidine and octenidine to avoid surgical site infection (SSI). Plos One 2018; 13:e0193284.
- Pirnazar P, Wolinsky L, Nachnani S, et al. Bacteriostatic effects of hyaluronic acid. J Periodontol 1999; 70:370–374.
- Klimach O, Underwood CJ, Charlesworth D. Femoropopliteal bypass with a Goretex prosthesis: A long-term follow-up. Br J Surg 2005; 71:821–824.
- Feliciano DV, Mattox KL, Graham JM, et al. Five-year experience with PTFE grafts in vascular wounds. J Trauma Injury Infect Critic Care 1985; 25:71.
- Clowes AW, Kirkman TR, Clowes MM. Mechanisms of arterial graft failure. II. Chronic endothelial and smooth muscle cell proliferation in healing polytetrafluoroethylene prostheses. J Vasc Surg 1986; 3:877–884.
- Stone IK, von Fraunhofer JA, Masterson BJ. Mechanical properties of coated absorbable multifilament suture materials. Obstetr Gynecol 1986; 67:737–740.
- Stone IK, von Fraunhofer JA, Masterson BJ. A comparative study of suture materials: Chromic gut and chromic gut treated with glycerin. Am J Obstetr Gynecol 1985; 151:1087–1093.
- Stone IK, Masterson BJ, Von Fraunhofer JA. Knot stability and tensile strength of an absorbable suture material. Surface Coatings Technol 1986; 27:287–293.
- Fraunhofer JA von, von Fraunhofer JA, Storey RJ, et al. Tensile properties of suture materials. Biomaterials 1988; 9:324–327.
- Hertweck SP, von Fraunhofer JA, Masterson BJ. Tensile characteristics of PTFE sutures. Biomaterials 1988; 9:457.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Bhavana Garapati* and Thamaraiselvan Murugan
Department of Periodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical sciences (SIMATS), Saveetha University, Chennai, IndiaReceived: 07-Aug-2022, Manuscript No. jrmds-22-63048; , Pre QC No. jrmds-22-63048(PQ); Editor assigned: 09-Aug-2022, Pre QC No. jrmds-22-63048(PQ); Reviewed: 24-Aug-2022, QC No. jrmds-22-63048(Q); Revised: 29-Aug-2022, Manuscript No. jrmds-22-63048(R); Published: 06-Sep-2022
