Research Article - (2022) Volume 10, Issue 10
Evaluation of Shear Bond Strength of Metal Orthodontic Brackets to Composite Using Different Surface Conditioning Methods
Ola Ali Mahmood1*, Mehdi Abdulhadi Mehdi1 and Asseel Yousif Rashid2
*Correspondence: Dr. Ola Ali Mahmood, Department of Orthodontics, College of Dentistry, University of Baghdad, Baghdad, Iraq, Email:
Abstract
Introduction: The rise of adult patient looking for orthodontic treatment that more likely to have existing restoration leads to increase in bonding of brackets to composite restoration. To ensure clinically optimum bond strength of brackets to composite, researchers are comparing and evaluating several surface treatment approaches.
Aims: The study's purpose is to assess the effect of different mechanical surface conditioning approaches (no preparation, diamond bur grinding, sandblasting with Al2O3, Er, Cr; YSGG laser irradiation) on Shear Bond Strength (SBS) of stainless steel orthodontic brackets to composite restoration.
Materials and methods: In this in vitro study 48 Composite discs were constructed (D=10 mm, H=4 mm). The samples were divided into two groups (n=24), one group underwent thermocycling (5000 cycle), then each group subdivided into four subgroups (n=6) according to the surface conditioning method (no-preparation, diamond bur, sandblasting with Al2O3, and Er, Cr: YSGG laser irradiation). After the brackets have been bonded to the composite discs, SBS of all the samples measured in a universal testing machine. Data was analyzed using one way ANOVA and post-hoc test. The samples were then examined at a magnification of x10 under a stereomicroscope to evaluate their failure mode and Adhesive Remnant Index (ARI). Kruskal-wallis test was used to compare ARI scores.
Results: No significant difference in shear bond strength between the composite control groups. However, significant difference in SBS values in the aged composite groups was recorded; the laser group values (10.81 MPa) were the highest among the tested groups. The no preparation aged group (2.95 MPa) has had the lowest SBS. ARI scores showed no significant difference among all groups (P>0.05). Sandblasting and grinding group mostly showed ARI score 2 and 3, however, score 0 and 1 were predominant in the no preparation and laser groups.
Conclusions: Diamond bur grinding, sandblasting with aluminum oxide and Er; Cr: YSGG laser irradiation of composite surface yields clinically acceptable outcomes in terms of shear bond strength and ARI values, bond strength with no preparation of composite surface was below the clinically acceptable range.
Keywords
Shear bond strength, Diamond bur, Sand blasting, Er-Cr YSGG laser
Introduction
An effective orthodontic treatment requires a strong bond between the orthodontic brackets and the tooth or restorative surfaces [1].
Composite are widely used to restore carious teeth, it could be seen on both the labial surfaces of maxillary incisors and the buccal surface of posterior teeth [2]. Bonding to composite surfaces is often accompanied with many difficulties. The bond strength should be capable of withstanding the applied loads by orthodontic appliances. Also, the composite restoration should not be damaged during debonding due to high bond strength [3]. To withstand the masticatory stresses, the minimum bond strength should be 6 to 8 MPa [4].
New composite bond strength to an aged composite restoration is weakened with time, resulting in the added resin failing prematurely [5]. As composites mature following placement, the number of vinyl groups (C=C) available for cross polymerization to the added composite layer diminishes. Chemical bonding between new and aged resin composites is not dependable [6]. Orthophosphoric acid etching has been shown to have no effect on composite surface and have the ability to cleans its surface only [2,7].
Surface roughening of an aged composite to encourage mechanical interconnecting and following treatment with bonding agents to facilitate surface wetting and effective chemical bonding are frequently required to improve bond strength of the new composite to the old composites surface [8].
Different approaches have been suggested to assess the most effective surface treatment method of the composite surface [6,9]. Previous studies [1,8] have suggested roughening with a bur, other recommended sandblasting as a conditioning method [2,10]. Some studies claimed that erbium lasers generate micron-scale explosions inside the restorative material and create craters in the composite resin, and they can be utilized to bond orthodontic brackets to composite restorations [11].
Materials and Methods
Sample preparation: forty eight composite discs with a diameter of 10 mm and a thickness of 4 mm were fabricated from composite resin (3 MTM ESPA, Minnesota, USA)using a plastic mold. Then using a visible light-curing unit, the composite surface light cured for 20 sec. 5 N weight placed on top of the slide for 20 sec. The weight and slide then removed, extra composite removed, and light-cured for another 20 sec. The composite discs were removed from the plastic mold and then polished with silicon carbide papers, then ultrasonically cleaned in distal water for 5 minutes and visually examined for cracks or faults. The samples incubated in artificial saliva for 24 hours at 37°C.
Mounting of the samples: Acrylic blocks were fabricated to hold the samples during the procedure of surface treatment and debonding.
Grouping of samples: The forty eight composite samples were randomly divided into two groups (n=24), the composite control group and the aged group (by thermocycling), then each groups subdivided into four groups consist of six specimens (n=6) according to the surface treatment method (Figure 1).
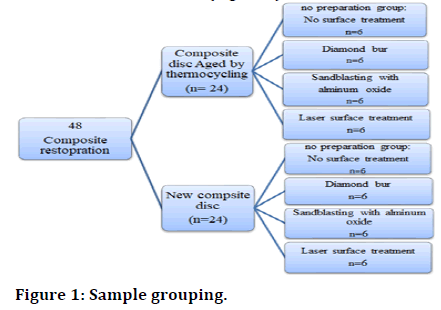
Figure 1: Sample grouping.
No preparation group: no surface treatment was carried out on composite disc.
Diamond bur grinding group: Using a high-speed dental hand piece and continual water spray, The composite discs was abraded with a diamond bur (Horico, Hopf, Ringleb and Co. GmbH and CIE Gardeschutzenweg 82,12203 Berlin) from two directions perpendicular to each other for three times in each direction [12].
Sandblasting with aluminium oxide group: Using air abraser, under pressure of 2.8 bar (0.28 MPa), the composite surface was abraded from 10 mm distance, with 50 μm aluminium oxide particles at a 450 angle for 15 sec [13].
Er, Cr: YSGG laser group: the composite surface irradiated with Water lase I plus Er, Cr: YSGG Laser. The beam irradiation was in a focused non-contact phase from 2 mm distance perpendicular to the composite surface, the laser wavelength was 2780 nm. The bonding surface was treated for 20 seconds with power of 3 W and frequency of 20 Hz using scanning movement [14].
Bonding procedure
Stainless steel 0.022" MBT maxillary central incisor brackets (OrthoTechnology-Tampa, Florida, USA). With 11.46 mm2 surface area bonded to the conditioned composite surfaces. In all groups a thin coating of the primer was applied to the etched composite surface, then an equal amount of the adhesive applied on the base of brackets and positioned in the centre of the surface of composite cylinder by clamping tweezers. Then a constant load of 7.05 ounce (200 gm.) was applied on the bracket by using dental surveyor at 90℃ to the bracket for 10 sec to ensure that the brackets were placed under equal pressure. The extra adhesive around the brackets was then removed with an explorer. Then, from the mesial surface, light-cured for 20 sec and from the distal surface, light-cured for 20 seconds [15]. The samples stored in artificial saliva at 37℃ for 48 h then thermocyclied for 500 cycles before the bond strength test.
Testing
Shear bond strength testing: The tinius olsen universal testing machine was used to perform the shear bond strength test, which had a loading cell of 50 kg. And a crosshead speed (0.5 mm/min).
Each sample was placed on the testing machine's base in a metal vice. The chisel end rod was put into the upper arm of the testing machine with the chisel end parallel to the bonded composite surface, creating a shear force at the bracket base until the bracket debonded. The ultimate magnitude of the reading at the time of bracket debonding from the composite surface was taken; the force applied by the testing equipment was measured in kilograms and converted into newton’s by the equation below
Force (N)=Load (kg) X Ground acceleration (9.8 m/sec.).
The force was divided by the surface area of the bracket base to measure the bond strength in Mega Pascal (MPa) units.
Adhesive remnant index measurement. The adhesive remnant was evaluated and scored under a stereomicroscope at a magnification of 10X. The 4-point artun and bergland scale was employed in the ARI evaluation
Results
Shear bond strength
Testing the normality of the distribution of data: The normality of distribution of data was evaluated using Shapiro-Wilk test. Test results showed that there is no significant difference between groups. So the data are normally distributed p-value ˃0.05 (Table 1).
| Groups | Sub groups | Shapiro- Wilk test |
Df | P-value |
|---|---|---|---|---|
| Composite Control group | No preparation | 0.876 | 6 | 0.249 |
| Diamond bur | 0.893 | 6 | 0.334 | |
| Sandblasting | 0.804 | 6 | 0.064 | |
| Er-Cr YSGG Laser | 0.801 | 6 | 0.059 | |
| Aged composite | No preparation | 0.824 | 6 | 0.095 |
| Diamond bur | 0.962 | 6 | 0.835 | |
| Sandblasting | 0.974 | 6 | 0.921 | |
| Er-Cr YSGG Laser | 0.954 | 6 | 0.770 |
Table 1: Testing the normality of the distribution of data.
Descriptive statistics of the Shear Bond Strength (SBS)
Mean, standard deviation, minimum, maximum values of SBS for all groups are presented in table 2 the test result showing the highest mean SBS was produced in ER-CR YSGG Laser aged group (10.81 ± 2.58 MPa) while the lowest mean SBS was produced by the aged composite no preparation group (2.95 ± 1.80 MPa).
| Groups | Sub groups | N | Mean | SD | SE | Min | Max |
|---|---|---|---|---|---|---|---|
| Composite control group | No preparation | 6 | 5.9633 | 3.67412 | 1.49995 | 2.03 | 10.34 |
| Diamond bur | 6 | 8.7483 | 3.82706 | 1.56239 | 4.79 | 15.58 | |
| Sandblasting | 6 | 9.03 | 3.84505 | 1.56973 | 6.11 | 16 | |
| ER-CR YSGG Laser | 6 | 10.3033 | 3.0936 | 1.26296 | 5.54 | 12.78 | |
| Aged composite | No preparation | 6 | 2.95833 | 1.806415 | 0.737466 | 1.44 | 5.98 |
| Diamond bur | 6 | 8.9383 | 2.12272 | 0.8666 | 6.24 | 11.78 | |
| Sandblasting | 6 | 10.805 | 3.55766 | 1.45241 | 6.54 | 16.27 | |
| ER-CR YSGG Laser | 6 | 10.8133 | 2.58491 | 0.458338 | 7.72 | 14.4 |
Table 2: Descriptive statistics of the Shear Bond Strength (SBS).
Inferential statistics of the shear bond strength test
Shear bond strength between groups with different surface treatment: Mean difference comparison of the shear bond strength between the composite different surface treatment subgroups in the control and the aged group with was tested using one way analysis of variance (ANOVA). Data homogeneity was confirmed using Levene ´s test. Post-hoc Tukey´s test was used to reveal the difference in SBS between the groups.
Composite control group (without aging) with different surface treatment: Test result showed that there is no significant difference in shear bond strength between the composite control groups with different surface treatment as presented in Table 3. The highest bond strength was produced by the laser group (10.30 ± 3.09 MPa) while the lowest bond strength was produced by the No preparation group (5.59 ± 3.67 MPa).
| Groups | ANOVA test | Tuckey´s test | ||
|---|---|---|---|---|
| Between groups | F-test | P-value | Among groups | P-value |
| 1.528 | 0.238 | No preparation–Diamond bur | 0.555 | |
| No preparation-Sandblasting | 0.475 | |||
| No preparation–Er-Cr YSGG Laser | 0.195 | |||
| Diamond bur-Sandblasting | 0.999 | |||
| Diamond bur-Er-Cr YSGG Laser | 0.878 | |||
| Sandblasting–Er-Cr YSGG Laser | 0.928 | |||
Table 3: Comparison of SBS values between Composite controls groups with different surface treatment by ANOVA and Post hoc Tuckey´s test.
The aged composite group: As presented in Table 4, there is a significant difference in shear bond strength between the tested groups, within the groups the No preparation group showed the lowest SBS (2.59 ± 1.80) compared with the diamond bur, sandblasting and the laser group. There was no significant difference in SBS between diamond bur with sandblasting and laser groups and between the sandblasting with laser group.
| Groups | ANOVA test | Tuckey´s test | ||
|---|---|---|---|---|
| Between groups | F-test | P-value | Among groups | P-value |
| 12.250 | 0.000 | No preparation–Diamond bur | 0.004 | |
| No preparation-Sandblasting | 0.000 | |||
| No preparation–Er-Cr YSGG Laser | 0.000 | |||
| Diamond bur-Sandblasting | 0.609 | |||
| Diamond bur–Er-Cr YSGG Laser | 0.604 | |||
| Sandblasting–Er-Cr YSGG Laser | 1.000 | |||
Table 4: Comparison of SBS values between aged composite with different surface treatment by ANOVA and Post hoc Tuckey´s test.
Comparison of SBS between the control and aged composite groups
As presented in Table 5, no significant difference in mean SBS between the composite control and aging group in all the tested groups.
| Groups | Shear bond strength | Comparison | ||||
|---|---|---|---|---|---|---|
| Control group | Aged group | |||||
| Mean | S.D. | Mean | S.D. | T-test | P-value | |
| No preparation | 5.963 | 3.674 | 2.958 | 1.806 | 1.798 | 0.114 |
| Diamond bur | 8.7483 | 3.82706 | 8.9383 | 2.12272 | -0.106 | 0.917 |
| Sandblasting | 9.0300 | 3.84505 | 10.8050 | 3.54716 | -0.830 | 0.426 |
| Er-Cr YSGG Laser | 10.3033 | 3.09360 | 10.8133 | 2.58491 | -0.310 | 0.763 |
Table 5: Comparison of SBS between the control and aged composite groups using independent T-test.
Adhesive Remnant Index (ARI)
Frequency distribution of the Adhesive Remnant Index (ARI) scores (Table 6).
| Groups | Subgroups | Score 0 | Score 1 | Score 2 | Score 3 |
|---|---|---|---|---|---|
| Composite control group | No preparation | 4 (66%) | 1 (16%) | 1 (16%) | 0 (0%) |
| Diamond bur | 1 (16%) | 2 (33.3%) | 1 (16%) | 2 (33.3%) | |
| Sandblasting | 1 (16%) | 1 (16%) | 0 (0%) | 4 (66%) | |
| Er-Cr Laser | 2 (33.3%) | 4 (66%) | 0 (0%) | 0 (0%) | |
| Aged composite group | No preparation | 4 (66%) | 0 (0%) | 2 (33.3) | 0 (0%) |
| Diamond bur | 0 (0%) | 4 (66%) | 1 (16%) | 1 (16%) | |
| Sandblasting | 1 (16%) | 4 (66%) | 0 (0%) | 1 (16%) | |
| Er-Cr Laser | 1 (16%) | 5 (83.3%) | 0 (0%) | 0 (0%) |
Table 6: Frequency distribution of the Adhesive Remnant Index (ARI scores in all tested groups.
Comparison of ARI scores within tested groups: Statistical analysis showed that ARI scores are normally distributed. The Kruskal–Wallis test showed that there is no significant difference in ARI distribution among groups.
Discussion
In recent years, an increasing number of adults have sought orthodontic treatment. As a result, there is a greater need for orthodontic appliances to be placed on teeth that have already been restored with composite resin restorations or composite laminate veneers [7]. Bonded brackets are subjected to different types of forces in the oral cavity which are difficult to measure. Orthodontic forces rarely exceed 4.45 N per tooth, according to Newman. Reynolds and von Fraunhofer, on the other hand, discovered that minimum bond strength of 5.9 to 7.8 MPa was sufficient for most clinical orthodontic purposes
In this study composite control group had an average SBS of (2.95 MPa ± 1.80 SD) and (5.96 MPa ± 3.67 SD) for the aged group which was lower than the acceptable values of 6–8 MPa for clinically appropriate bond strength of a metal bracket to enamel [4]. This comes in agreement with a study by Demirtas, et al. in which the 37 % phosphoric acid surface treatment on composite group showed low SBS values 4.6 ± 1.4 MPa. Except for the control group, all surface conditioning groups' mean SBS values were within or beyond these limits, indicating that they were satisfactory for clinical applications.
In the grinding group SBS values were not particularly high (8.4010 ± 1.82 SD) for the control group and (8.93 ± 2.12 SD) for the aged group, however, the findings in this group was all higher than the clinically acceptable limit (6-8 MPa) [4].
Similar results in a study by Bayram, et al. discovered that using a diamond bur and air abrasion resulted in mean shear bond strengths of 10.6 and 10.3 MPa, respectively, compared to only 2.8 MPa when no surface preparation was utilized.
In contrast, grinding provided the highest shear bond strength values when compared to other processes, according to Bishara, et al. and Eslamian, et al. findings. Previous research have not established an assessable method for surface treatment using a bur, hence it is susceptible to operator bias [2].
As a result of the lack of precise control and measurement in grinding, the results can be inconstant. The type of material used to polish the surface could have an effect on the results. Bishara, et al. for example, used carbide bur instead of diamond bur.
Grinding is contraindicated for composite surface preparation, according to Bayram, et al. and Demirtas et al. due to its unexpected effect and possible damage of composite surface that could lead to discoloration and plaque build-up.
The study findings found that clinically appropriate bond strengths were attained in sandblasting with aluminum oxide group (9.03 MPa ± 3.09 SD) for the control group and (10.80 MPa ± 3.55 SD) for the aged group.
Bond strength in the sandblasting group was high and this could be attributed to the uneven and deep dents that are generated in composite surface; according to Viwattanatipa, et al. pitting abnormalities with no distinct pattern were detected using a scanning electron microscope. Aluminium oxide particles caused micro porosities on the composite surface. Which were not found in other groups? As a result, a greater surface area of resin matrix and filler particles will be available for adhesive bonding.
Sandblasting with Al2O3 produced a small preparation area on the composite surface and could be considered more suitable for conditioning the composite surface to enhance SBS and it is an easier and more controllable method. Despite clinically appropriate SBS levels in the diamond bur group, the procedure should be applied with cautions due to the diamond bur's unpredictable abrasion [10].
Bond strength produced by laser irradiation of composite surface was (10.30 ± 3.09 MPa) for the control group and (10.81 ± 2.58 MPa) for the aged group.
The effect of the Er:YAG laser on composite resin ablation has been studied [16,17]. And it has been found that explosive vaporization is followed by hydrodynamic ejection in composite resin ablation. Rapid melting causes powerful expansion forces as the volume of the material changes during the melting process. Furthermore, surface protrusions form as a result of opposing forces interacting with the composite resin structure, and these projections are ejected as droplets away from the surface. This type of effect is thought to occur in composite resin ablation after Er:Cr:YSGG laser irradiation by a process analogous to that seen in hard tissue irradiation by Er:Cr:YSGG and Er:YAG lasers [18].
The absence of a smear layer on the surface of the composite may explain why the laser-treated group's repair bond strength is higher than the bur grinding group. The bur wears out substrates like restorative materials and leaves a smear layer behind, while the laser ablates the restoration surface without leaving a smear layer. The Er:Cr:YSGG laser does not create a smear layer, according to [16]. And many other studies [18,19]. Due to its low surface energy, the formation of a smear layer makes adhesive resin bonding difficult [20]. Because the aluminum oxide particles in the sandblasting method have some negative effects on the human body, Er:Cr:YSGG laser can be regarded a harmless substitute modality for composite surface roughening [21].
Nano filled composite was used in this study as in as study by Viwattanatipa, et al. In Demirtas, et al. study nanohybrid composite have been used, while in Najafi, et al. study micro hybrid composite was used. During surface treatment large filler particles are dislodged in hybrid composites (micro hybrid and nanohybrid), resulting in a rougher surface. Nano cluster filler particles in nanofill composites are abraded at an equal amount to the adjacent matrix. As a result, a comparatively smoother surface is produced; resulting in decreased shear bond strength as a result of reduced micromechanical retention [22]. The relatively low SBS value may be attributed to the type of composite used.
Mode of bond Failure
The result of this study found no significant difference in ARI score was found between the different surface treatment groups Table 7.
| Group | Df | P-value |
|---|---|---|
| Composite control group | 6 | 0.063 |
| Aged composite group | 6 | 0.313 |
Table 7: Comparison of ARI scores among different surface treatment group using Kruskal-Wallis test.
In the no preparation and laser group low ARI scores are predominant indicating that the mode of failure is mostly adhesive at the tooth adhesive interface.
In the diamond bur grinding group, there was a high rate of cohesive failure. The cohesive failure mode jeopardizes the integrity of resin-based composite restorations and increases the cost of repair or replacement [5].
The results found that ARI scores of 3 were the most common in the sandblasting group. It revealed that most of the adhesive stayed on the composite surface, indicating adequate adhesive adherence and high bond strength [23].
Conclusion
In this in vitro study, alternative mechanical surface conditioning procedures were used to test brackets bonding to aged composites by different mechanical surface conditioning methods. Within the study's limitations, the conclusions are:
• Surface roughening is effective mechanical method in bonding an orthodontic attachment to aged resin composite surfaces.
• Clinically, acceptable shear bond strength values can be obtained with the application of diamond bur grinding, AI2O3 particle abrasion, or Er:Cr:YSGG laser irradiation
• Roughening the surface of a composite resin restoration mechanically with a Er:Cr:YSGG laser, provided greater bond strengths, while the diamond bur yield the lowest SBS among the surface treatment methods
• With sandblasting with Al2O3 particles and diamond bur application, bracket failure patterns were at the bracket adhesive interface and for no preparation and Er:Cr:YSGG laser, failure patterns were at the composite adhesive interface. In the sandblasting and diamond bur grinding specimens, the bulk of the adhesive retained on the composite surface, whereas in the no preparation and laser specimens, the adhesive was predominantly separated from the composite surface.
References
- Keim RG, Gottlieb EL, Nelson AH, et al. JCO Orthodontic Practice Study. Part 1: trends. J Clin Orthod 2013; 47:661-680.
- Viwattanatipa N, Jermwiwatkul W, Chintavalakorn R, et al. The effect of different surface preparation techniques on the survival probabilities of orthodontic brackets bonded to nanofill composite resin. J Orthod 2010; 37:162-173.
- Bayram M, Yesilyurt C, Kusgoz A, et al. Shear bond strength of orthodontic brackets to aged resin composite surfaces: effect of surface conditioning. Eur J Orthod. 2011; 33:174-179.
- Reynolds I. A review of direct orthodontic bonding. Br J Orthod 1975; 2:171-178.
- Eslamian L, Farahani AB, Mousavi N, et al. The effects of various surface treatments on the shear bond strengths of stainless steel brackets to artificially-aged composite restorations. Aust Orthod J 2011; 27:28–32.
- Padipatvuthikul P, Mair LH. Bonding of composite to water aged composite with surface treatments. Dent Mater 2007; 23:519–525.
- Hammad SM, El Banna MS. Effects of cyclic loading on the shear bond strength of metal orthodontic brackets bonded to resin composite veneer surface using different conditioning protocols. Prog Orthod 2013; 14:14.
- Hemadri M, Saritha G, Rajasekhar V, et al. Shear bond strength of repaired composites using surface treatments and repair materials: an in vitro study. J Int Oral Health 2014; 6:22.
- Rinastiti M, Ozcan M, Siswomihardjo W, et al. Effects of surface conditioning on repair bond strengths of non-aged and aged microhybrid, nanohybrid, and nanofilled composite resins. Clin Oral Investig 2011; 15:625–633.
- Demirtas HK, Akin M, Ileri Z, et al. Shear bond strength of orthodontic brackets to aged nanohybrid compositeresin surfaces using different surface preparation. Dent Mater J 2015; 34:86–90.
- Mirhashemi AH, Chiniforush N, Sharifi N, et al. Comparative efficacy of Er, Cr: YSGG and Er: YAG lasers for etching of composite for orthodontic bracket bonding. Lasers Med Sci 2018; 33:835–841.
- Bishara SE, Ajlouni R, Oonsombat C, et al. Bonding orthodontic brackets to composite using different surface preparations and adhesive/primers: a comparative study. World J Orthod 2003; 4:343–347.
- Valizadeh, Sara, et al. "In vitro evaluation of shear bond strength of orthodontic metal brackets to aged composite using a self-adhesive composite: Effect of surface conditioning and different bonding agents." Int Orthod 18.3 2020; 528-537.
- Humaid, J, Adel S, Sumit B, et al. "Effect of erbium laser on microtensile bond strength of fissure sealant in primary teeth: an in vitro study." Saudi J Med Sci 2018; 27.
- Najafi HZ, Mousavi M, Nouri N, et al. Evaluation of the effect of different surface conditioning methods on shear bond strength of metal brackets bonded to aged composite restorations. Int Orthod 2019; 17:80-88.
- Lizarelli Rde F, Moriyama LT, Bagnato VS, et al. Ablation of composite resins using Er: YAG laser–comparison with enamel and dentin. Lasers Surg Med 2003; 33:132–139.
- Lizarelli Rde F, Moriyama LT, Pelino JEP, Ablation rate and morphological aspects of composite resins exposed to Er: YAG laser. J Oral Laser App 2005; 5:151–160.
- Hossain M, Nakamura Y, Yamada Y, et al. Microleakage of composite resin restoration in cavities prepared by Er; Cr: YSGG laser irradiation and etched bur cavities in primary teeth. J Clin Pediatr Dent 2002; 26:263–268.
- Basaran G, Ozer T, Berk N, et al. Etching enamel for orthodontics with an erbium, chromium: yttrium-scandium-gallium-garnet laser system. Angle Orthod 2007; 77:117–123.
- Celik E U, Ergu cu Z, Turkun LS, et al. Shear bond strength of different adhesives to Er:YAG laserprepared dentin. J Adhes Dent 2006; 8:319–325.
- Usumez S, Orhan M, Usumez A, et al. Laser etching of enamel for direct bonding with an Er; Cr: YSGG hydrokinetic laser system. Am J Orthod Dentofacial Orthop 2002; 122:649–656.
- Viwattanatipa N, Prasertsangwal J, Juntavee N, et al. Weibull analysis of shear/peel bond strength of orthodontic buccal tubes bonded to five resin composites. Orthod Waves 2008; 67:120-127.
- Carstensen W. Effect of reduction of phosphoric acid concentration on the shear bond strength of brackets. Am J Orthod Dentofacial Orthop 1995; 108:274–277.
Author Info
Ola Ali Mahmood1*, Mehdi Abdulhadi Mehdi1 and Asseel Yousif Rashid2
1Department of Orthodontics, College of Dentistry, University of Baghdad, Baghdad, Iraq2Department of laser/Dentistry, Al Elweah specialized dental center , Iraqi ministry of health, Baghdad, Iraq
Citation: Ola Ali Mahmood, Mehdi Abdulhadi Mehdi, Asseel Yousif Rashid, Evaluation of Shear Bond Strength of Metal Orthodontic Brackets to Composite Using Different Surface Conditioning Methods, J Res Med Dent Sci, 2022, 10 (10): 239-245.
Received: 02-Aug-2022, Manuscript No. JRMDS-22-56337; , Pre QC No. JRMDS-22-56337(PQ); Editor assigned: 04-Aug-2022, Pre QC No. JRMDS-22-56337(PQ); Reviewed: 18-Aug-2022, QC No. JRMDS-22-56337; Revised: 03-Oct-2022, Manuscript No. JRMDS-22-56337(R); Published: 13-Oct-2022
