Research Article - (2022) Volume 10, Issue 9
Evaluation of Marginal Bone Level Change Utilizing a Simplifed DrillingVersus Conventional Drilling Techniques
Al-Hassan Ali Naser* and Thair A Lateef Hassan
*Correspondence: Al-Hassan Ali Naser, Department of Oral and Maxillofacial Surgery,College of Dentistry, University of Baghdad, Iraq, Email:
Abstract
Background: Conventional drilling technique is effective for implant site preparation but it is time consuming, especially when multiple implants are to be placed and unpleasant for the patient as the duration of the intervention may be excessively long causing discomfort. Simplifying the drilling sequence would be meaningful for implant surgery if it does not exert a negative influence. This was prospective clinical study conducted to evaluate the stability and marginal bone level change of implant placements after simplifying the drilling sequence.
Aim: Evaluation of dental implant stability and marginal bone level change using a simplified drilling approach as opposed to a traditional drilling technique.
Materials and methods: A total of 17 patients (9 females and 8 males) included in this study. The patient’s age ranged from 18-64 years with 46 bone level dental implants. These patients were divided into two groups: group A (simplified drilling approach), in which only the first and final drills were used to prepare implant sites, and group B (traditional drilling technique), in which implants were implanted sequentially. The implant stability quotient was measured both immediately and 16 weeks after the dental implant was placed. Marginal bone level evaluated 7 days of surgery to determine the marginal bone level as baseline data and 16 weeks following to the surgery utilizing con beam computed tomography.
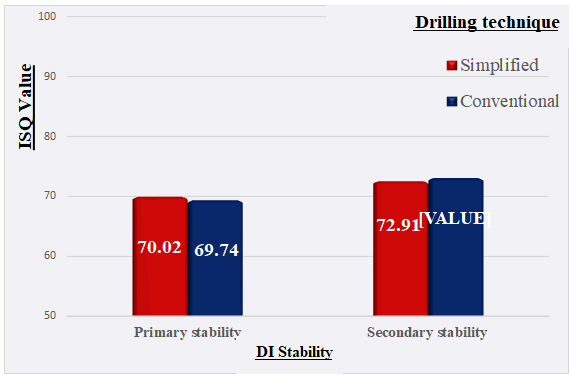
Results: Implant stability quotient values for secondary stability of group A measured at 16 weeks after implant installation was not significantly increased as compared with the primary base line value (70.02 vs. 72.91). While, there was a significant increase in the mean of implant stability quotient values from primary to secondary stability in group B after 16 weeks (69.74 vs. 73.44).
About 16 weeks after implant installation there was no significant difference in the marginal bone level changes between the two groups. During the study's follow-up check-ups, no implant was lost, resulting in a 100% survival rate.
Conclusion: In spite of the limits of this clinical trial, both drilling techniques produced successful results over a 16 weeks post-insertion follow-up period, however, the simplified drilling technique required less surgical time without having to sacrifice implant stability and bone level during implant site preparation.
Keywords: Dental implant, Conventional drilling, Marginal bone level, Stability
Introduction
Implant success is defined as the lack of a continuous radiolucency around the implant and the absence of any observable implant movement, both of which are influenced by a variety of parameters, including the drilling sequence and drilling efficiency [1]. As a result, the primary goal of drilling is to provide fixation for the implant in the apical portion and/or fixation to the lateral walls of the surrounding bone in order to achieve primary stability [2]. This is defined as the implant’s ability to withstand axial, lateral, and rotational loading [3]. Implant stability can be achieved through two methods: the mechanical stability established between the implant and the surrounding bone at the time of surgery or primary mechanical implant stability, and the biological stability achieved through the Osseo integration process and bone remodelling during the functional life of the implant (secondary implant stability) [4]. The primary success of dental implants is achieving Osseo integration, which is influenced by many factors including implant design, surface treatments, as well as treatment method. Implant drilling is also a major influential factor [5]. Described different methods of detection of implant stability into two categories as invasive and non-invasive methods [6]. Resonance Frequency Analysis (RFA) is non-invasive and the most accurate and precise method [3]. The implant bone site preparation plays a key role in Osseo Integration (OI) development because it allows obtaining an implant bone bed suitable for the fixture dimensions ensuring primary implant stability [7]. Marginal bone level defined as the distance from the first bone-to-implant contact to the implant abutment interface was determined at the mesial and distal aspect of the implant [8]. A crucial factor in the construction of the placement location has been a gradual drilling sequence (conventional drilling). Using plenty of drills to place a single implant, on the other hand, can become boring for doctors, especially when numerous implants are being placed, as well as for the patient, as the procedure can take an inordinate amount of time and cause discomfort. Furthermore, because of the increased release of pro-inflammatory cytokines and the resulting enhanced inflammatory response, extended tissue exposure may be harmful to the postoperative course. Therefore, any simplification of the techniques for site preparation can be favourably accepted by both clinicians and patients [9-10]. Simplified drilling consists of the reduction in the number of drills through the use of a pilot drill followed by a final one [2]. This clinical study focuses on determining dental implant stability and marginal bone level using a simplified versus traditional drilling approach, as well as measuring drilling duration.
Materials and Methods
This clinical prospective comparative study was conducted from December 2020 to November 2021 in the College of Dentistry Teaching Hospital, Department of Oral and Maxillofacial Surgery/Dental Implant Unit/University of Baghdad and Napoli private dental clinic. The sample registered patients aged ≥ 18 years presented with missing teeth in maxilla, mandible or both and requested implant supported restoration utilizing dental implant (NucleOSS™ T6, Turkey). A total of 17 Iraqi patients aged 18-64 years (9 females and 8 males) met the eligibility criteria enrolled in this study receiving 46 DI. These cases were separated into two groups: group A (simplified drilling approach), in which just the initial and final drills were used to prepare the implant sites, and group B (traditional drilling technique), in which the implants were inserted by sequential drilling. For both, the surgical site of DI was examined for the hard and soft tissue clinically and preliminary Ortho Pantomo Gram (OPG).
Eligibility criteria: Good general health without any systemic diseases or local conditions that may compromise bone healing potential (as heavy smoking, hyperparathyroidism, fibrous dysplasia etc.), Patient’s age ≥ 18 years of both genders, Partially or completely edentulous maxilla or mandible with at least 6 months after teeth extraction subjected to (delayed implant placement protocol) and straightforward cases according to SAC classification.
Exclusion criteria: Patients excluded if any one of the following existed: systemic conditions that could interfere with normal healing or inability to withstand surgery such as current pregnancy, psychosis or unrealistic expectations, uncontrolled systemic diseases like uncontrolled diabetes, irradiation of the head and neck region or chemotherapy over the past 5 years, local conditions such as the presence of acute/chronic infection or local pathological conditions in the implant zone, active periodontitis and poor oral hygiene, advanced and complex cases according to SAC classification, and history or clinical evidence of Para functional habits (bruxism or clenching).
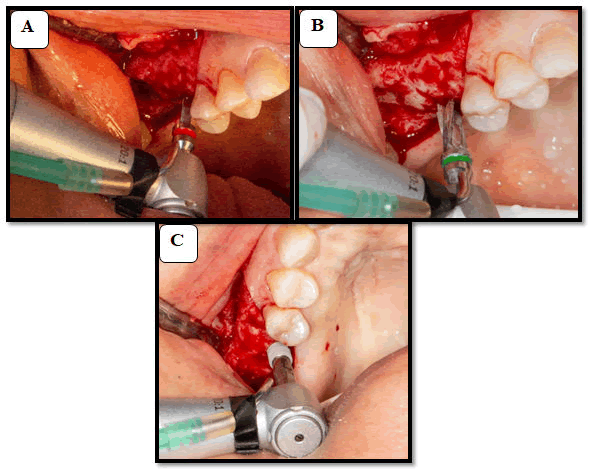
Surgical procedure: Lidocaine 2% (Septodent) was used to provide local anaesthetic to the anticipated surgical field, starting one tooth before and ending one tooth after the implantation location. Three-sided extensive flaps design to exposes the implant site. In the conventional drilling group, the preparation of the implant bed was carried out with drills of increasing diameter with copious normal saline solution irrigation and sequential drilling technique according to implant system recommendations using dental engine hand piece set at 800 (rpm) and torque equal to 35 N/cm. On the other hand, in the simplified drilling group, only the initial and final drills were used to prepare the implant’s bed. The implants were inserted by a surgical micro motor hand piece with a torque of 35 N/cm and speed of 35 rpm (Figure 1). Seating of DI was completed manually into its final position with the aid of a ratchet.
Figure 1: Simplified drilling technique. A) Locating the tooth site #3 by point drill; B) Final drill with diameter of 4.1 mm used as a final drill of tooth site #3; C) Installation of the implant into the prepared site in the motorized way.
The ISQ was measured immediately by the RFA test utilizing the PenguinRFA device with type 66 MulTipeg. The measurements were done in buccopalatal and mesiodistal directions and the average value was registered (Figure 2). Furthermore, the drilling time was calculated from the start of the pilot drill to the finish of the drilling procedure. Finally, the closer cap is subjoined to the implant. Interrupted 3/0 braided black silk sutures are used to close the wound. The prescribed medications were (Amoxicillin 500 mg+Clavulanic acid 125 mg) 3 times a day for 5 days, and Metronidazole 250 mg tablet 3 times a day for 5 days. Paracetamol 500 mg+Caffeine 65 mg tab was administered as a good choice of pain killer on need.
Figure 2: Measurement of the ISQ of DI using PenguinRFA device.
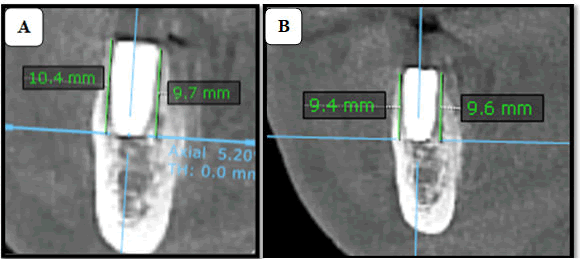
Follow up and data collection:For both groups (simplified and conventional groups) sutures were removed 7 days after surgery and the patients were subjected to CBCT examination to determine the MBL as baseline data.
The MBL evaluation made with (KAVO OP 3D; Germany) by determining the horizontal plane at the apical part and perpendicular to the long axis of the fixture. This resulted in four circumferential measurements buccomesial, linguomesial, buccodistal and linguodistal from the apical part of the implant to the margin of the crest. The average values of these sides also can be taken to estimate overall bone level changes.
The MBL change measurement and 2nd Stage Surgery: Sixteen weeks following surgery, all patients were informed to obtain another CBCT in order to measure MBL changes (Figure 3).
Figure 3: Two sagittal views of CBCT illustrating the bone level in relation to the tooth site # 30 within 1 week and 16 week after surgery.
Two sagittal views of CBCT illustrating the bone level in relation to the tooth site #30 within 1 week and 16 week after surgery. Two sagittal views of CBCT illustrating the bone level in relation to the tooth site #30 within 1 week and 16 week after surgery. Two sagittal views of CBCT illustrating the bone level in relation to the tooth site #30 within 1 week and 16 week after surgery.
The second stage surgery was accomplished with exposure of the DI using tissue punch with use of micro motor engine with 600 rpm. The secondary stability was measured in the same way applied for the primary one and a suitable healing abutment (gingival former) was placed for (7-14 days) to be ready for final prosthesis.
Statistical analysis: Data descriptive and analysis were performed with the use of IBM SPSS (Statistical Package for Social Sciences), software version 26. Wilcoxon signed rank and Mann-Whitney U test were used to test these data. Significant at P<0.05 not significant at P>0.05.
Results
Seventeen patients contributed to this study aged from 18-64 years with an average of 45.7 years and a standard deviation (SD) ± 14.602 as demonstrated in Figure 3. This study included 9 female and 8 male patients (52.9% vs. 47.1%) respectively with a female to male ratio of 1.1:1. Both groups received the same number 23 DI. From statistical point of view the mean of ISQ values for secondary stability of group A measured at 16 weeks after implant installation was not significantly increased as compared with primary stability base line value (70.02 vs. 72.91). While, there was a significant increase in the mean of ISQ values from primary to secondary stability in group B after 16 weeks (69.74 vs. 73.44). As well as there was no significant difference between the means of primary and secondary stability of both groups as illustrated in (Figure 4) and Table 1.
Figure 4: A column chart described the primary and secondary implant stability.
| Variable | No. of DI | Primary stability | P value | Secondary | P value | P value |
|---|---|---|---|---|---|---|
| Group | ||||||
| A | 23 | 70.02 ± 10.91 | 0.253 | 72.91 ± 5.73 | 0.809 | 0.183 |
| B | 23 | 69.74 ± 7.88 | 73.44 ± 4.48 | 0.013 | ||
Table 1: The primary and secondary implant stability.
Table 2 describe the significant time difference between simplified and traditional drilling techniques.
| Variable | Cone Beam Computed Tomography Reading (mm) | |||
|---|---|---|---|---|
| No. of DI. | MBL change | P value | P value | |
| Group | ||||
| A | 23 | 0.41 | 0 | 0.442 |
| B | 23 | 0.42 | 0 | |
Table 2: Correlation of drilling technique with MBL changes.
Marginal bone level was significantly decrease P<0.05 in both simplified and conventional group with no significant difference between groups, as presented in Table 3.
| Group | Mean ± SD (sec) | P value |
|---|---|---|
| A | 31.09 ± 4.02 | 0 |
| B | 60.66 ± 6.99 |
Table 3: Association of groups and drilling time.
Discussion
In the current study, the average of ISQ value of primary stability in the control and test groups was 69.74 ± 7.88 and 70.02 ± 10.91 respectively with no statistical significance. The average ISQ values 16 weeks after the placement were found to be 73.44 ± 4.48 and 72.91 ± 5.73, also with no statistical difference between the two groups.
Consequently the ISQ values of primary and secondary stability of the two groups, the control group exhibited a significant increase from 69.74 ± 7.88 to 73.44 ± 4.48, while the test group demonstrated a lesser increase from 70.02 ± 10.91 to 72.91 ± 5.73; however, these differences were statistically not significant.
The result of the current study is incompatible with a previous study performed by who found that there was a statistically significant difference of the average ISQ values after implant placement in the test and control groups (68.76 ± 15.75 and 82.12 ± 10.17) respectively. Also, the average ISQ values 5 months after the procedure were found to be 71.83 ± 9.00 and 80.72 ± 6.76, with statistically significant differences between the two groups [5].
Independent of DI size, recipient jaw, and implant zones, there is a high significant association (P=0.00) between drilling time required for simplified vs. conventional drilling techniques in the current study. The conventional drilling required more time (60.666.99 seconds) than the simplified drilling (31.094.02 seconds). This can be interpreted, that conventional drilling required more time owing to the increased number of drills utilized in sequential drilling according to the manufacture instruction from pilot drill reaching to the final one that corresponds to the diameter of selected DI, while utilizing the simplified technique resulted in a very short drilling time since only 2 drills were used.
According to, simplifying the drilling sequence reduced operative time by an average of 3.6 minutes while also reducing the number of problems. In this clinical study, simplify drilling reduced drilling time by an average of 47 seconds.
This difference with the current study could be due to the manner of time measurement used, which starts with site preparation and ends with complete implant seating [2].
Demonstrated in their study that a fast drilling phase, causing a decrease of the overall surgical time in which tissues remain exposed, also reduces tissue suffering. This may lead to better tissue preservation, reduced postoperative discomfort and better patient’s acceptance of the treatment [9].
The MBL change for the simplified and conventional group respectively 0.41 mm, 0.42 mm demonstrate no significant difference.
This is in agreement with who demonstrated the radiographic bone level changes 4 months after loading, the patients in the single drill group lost an average of 0.54 mm of peri-implant bone compared with 0.41 mm for those in the multiple-drill group [2]. There were no statistically significant differences for marginal bone level changes between the two groups (difference 0.13 mm, P=0.108). The present findings suggested no difference in marginal bone level changes can be expected between implants placed with a single drill versus implants inserted with multiple conventional drilling steps [10].
Conclusion
Both drilling techniques produced successful results over the 16 weeks post-insertion follow-up despite the limitation of this clinical trial; however, the simplified drilling technique required less surgical time without compromising implant stability or bone level during implant site preparation.
References
- Geckili O, Bilhan H, Geckili E, et al. Evaluation of Possible Prognostic Factors for the Success, Survival, and Failure of Dental Implants. Implant Dent 2014; 23:44–50.
- Guazzi P, Grandi T, Grandi G. Implant site preparation using a single bur versus multiple drilling steps: 4 months post-loading results of a multi-centre randomised controlled trial. Europe J Oral Implantol 2015; 8:283-290.
- Sachdeva A, Dhawan P, Sindwani S. Assessment of Implant Stability: Methods and Recent Advances. British J Med Res 2016; 12:1–10.
- Delgado-Ruiz R, Gold J, Somohano Marquez T, et al. Under-Drilling versus Hybrid Osseo densification Technique: Differences in Implant Primary Stability and Bone Density of the Implant Bed Walls. Materials 2020; 13:390.
- Kim HM, Cho JY, Ryu J. Evaluation of implant stability using different implant drilling sequences. J Dent Sci 2019; 14:152–156.
- Balaji VR, Manikandan Dhanasekaran D, BalaMuralei S. Implant stability-a measure of implant success. World J Advanced Sci Res2021; 4:17-26.
- Trisi P, Falco A, Berardini M. Single-drill implant induces bone corticalization during submerged healing: an in vivo pilot study. Int J Implant Dent 2020; 6.
- Raes F, Cosyn J, Crommelinck E, et al. Immediate and conventional single implant treatment in the anterior maxilla: 1 year results of a case series on hard and soft tissue response and aesthetics. J Clin Periodontol 2011; 38:385–394.
- Bettach R, Taschieri S, Boukhris G, et al. Implant Survival after Preparation of the Implant Site Using a Single Bur: A Case Series. Clin Implant Dent Relat Res 2013; 17:13–21.
- Patel A, Gil L, Castellano A, et al. Effect of Simplified One-Step Drilling Protocol on Osseo integration. Int J Periodontics Restorative Dent 2016; 82–87.
Author Info
Al-Hassan Ali Naser* and Thair A Lateef Hassan
Department of Oral and Maxillofacial Surgery,College of Dentistry, University of Baghdad, IraqCitation: Al-Hassan Ali Naser, Thair A Lateef Hassan, Evaluation of Marginal Bone Level Change Utilizing a Simplified Drilling Versus Conventional Drilling Techniques, J Res Med Dent Sci, 2022, 10 (9): 000-000.
Received: 18-Jul-2022, Manuscript No. JRMDS-22-55467; , Pre QC No. JRMDS-22-55467; Editor assigned: 20-Jul-2022, Pre QC No. JRMDS-22-55467; Reviewed: 03-Aug-2022, QC No. JRMDS-22-55467; Revised: 19-Sep-2022, Manuscript No. JRMDS-22-55467; Published: 26-Sep-2022