Research - (2022) Volume 10, Issue 1
Evaluation of Eustachian Tube Function in Chronic Suppurative Otitis Media in Relation to Surgical Treatment Results
Mohan kumar J* and MK Rajasekar
*Correspondence: Mohan kumar J, Department of ENT, Sree Balaji Medical College and Hospital, Chromepet, Chennai, Tamilnadu, India, Email:
Abstract
This was a two-year prospective research that looked at the Eustachian tube patency and surgical prognosis in individuals with Chronic Suppurative Otitis Media (tubo tympanic type). This is done to evaluate the surgical result of CSOM in both normal and dysfunctional Eustachian tube function, as well as to view the end result of myringoplasty compares to Eustachian tube function in CSOM. Tympanogram and forced inflation test were used to evaluate the ETF. Patients are divided into two groups based on their ear findings: Group 1: A successful graft will be one that has strong middle ear function. Group-2: Graft rejection or perforation as a result of otitis media will be classified as failure. The data was tabulated using the Chi-square test and the Fisher Exact Test. The statistical significance level was set at (P=0.05). The findings were analysed using SPSS version 17 and Microsoft Excel 2007.
Keywords
CSOM, Myringoplasty, Tympanogram, Surgical prognosis
Introduction
Persistent Suppurative otitis media is characterized as constant aggravation of middle ear cleft restricted to eustachian tube, anterior and inferior part of the mesotympanum and hypotympanumbecause of unsettled intense suppurative otitis media or intense necrotising otitis media which is irregular , mucopurulent , not noxious , moderate to plentiful , not blood stained release related with cp with two sorts (Type 1–permanent perforation syndrome, Type 2–persistent tubotympanic mucosal infection).
The Eustachian tube's function in chronic otitis media will be examined, The Eustachian tube's function in incomplete (no intact) tympanic membrane will be investigated using Impedance Audiometry and a dye instillation test to demonstrate the efficacy of the Eustachian tubes mucociliary transport mechanism. The following measures are used to evaluate the ventilation mechanism of the Eustachian tube [1-10].
Clinical evaluation
• Otoendoscopy.
• Nasopharyngoscopy and nasal endoscopy.
Audiometry
Tympanometry
Tympanometry is a test that determines how well the tympanic membrane, middle ear, and Eustachian tube are functioning. Middle ear effusion and negative middle ear pressure are consistently and objectively detected using this method. Some asymptomatic youngsters, on the other hand, may feel an increase in negative pressure. As a result, a substantially negative resting pressure implies Eustachian tube blockage, but a standard Tympanogram does not rule out the possibility of Eustachian tube malfunction. In situations with Patulous Eustachian tube dysfunction, a typical Tympanogram might be produced (Figure 1).
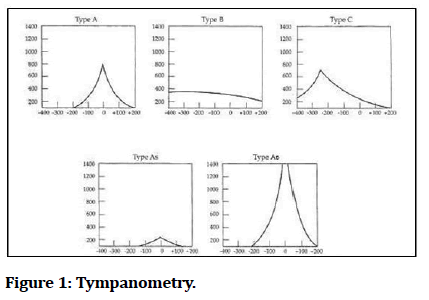
Figure 1: Tympanometry.
Manometry (Non intact TM)
The pump-manometer device is used to assess Eustachian tube function if the Tympanic membrane is not intact. The Eustachian tube's opening pressure should be between +400 and +600mm H20 (Figure 2).
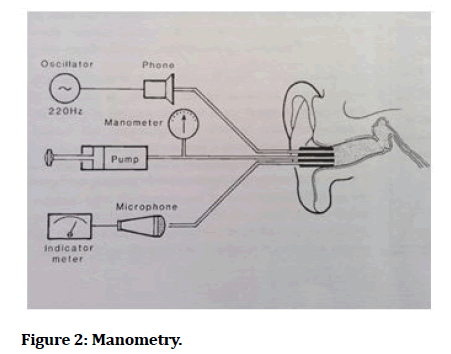
Figure 2: Manometry.
Toynbee test
The Toynbee test is performed to see if the eustachian tube is open or not. A positive test is the generation of negative pressure after swallowing with closed nostrils. Pneumaticotoscopy or a Tympanogram can be used to determine if the Tympanic membrane is intact before and after the surgery.
When the Tympanic membrane isn't intact, a manometer's impedance bridge can be used to complete the test.
Modified inflation-deflation test
Siemens model SD 30 tympanometer was utilised for the modified inflation-deflation test. With virtually every swallow, the typical Eustachian tube opens, and a negative or positive pressure delivered to the middle ear is gradually lowered until equalisation is achieved.
The tube with a hereditary, anatomical, or pathological defect impacting its normal function does not experience this normal decrease. In such situations, the drop in pressure finally reaches a point where additional swallowing has no effect on the pressure.
At most, the measurement can last no more than 4 minutes (240 seconds).
Nine step inflation-deflation tympanometric test
Bluestone developed a nine step test to study the Eustachian tube function if Tympanic membrane is intact (Figure 3).
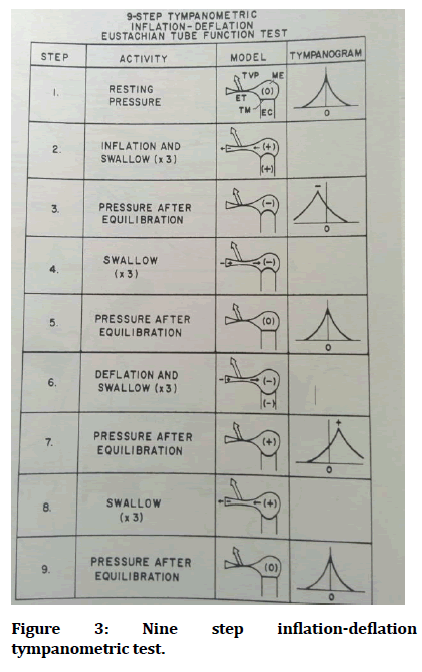
Figure 3: Nine step inflation-deflation tympanometric test.
Test of forced inflation
In CSOM patients with a non-intact Tympanic membrane, the forced inflation test is performed to evaluate Eustachian tube function. The middle ear pressure is raised to 500dPa with the manometer probe placed into the test ear before the Eustachian tube opens and the pressure drops. The Eustachian vent's passive opening is referred to as "opening pressure." Closing pressure is the pressure at which the Eustachian tube shuts after the pressure has been equilibrated. The patient is advised to swallow 3-5 times if the Eustachian tube does not open passively. The Eustachian tube will be opened, lowering the pressure. The Eustachian tube is in the process of opening. This is seen to be a successful test.
If the Eustachian tube does not open after swallowing, it is a bad sign. A positive test shows that the Eustachian tube is functioning normally, whereas a negative test suggests that the tube is significantly damaged.
Surgical procedure
Patients were scheduled for myringoplasty based on the status of their middle ear after an examination of Eustachian tube activity. For one week, antibiotics, analgesics, antihistamines, and multivitamins were given. On the seventh day following surgery, the sutures were removed.
Outcomes
Based on post-operative ear evaluations, patients were split into two groups.
A healed graft with robust middle ear work is a good result.
Graft failure or perforation owing to Otitis media during follow-up is defined as failure.
Case study 1 (Figure 4)
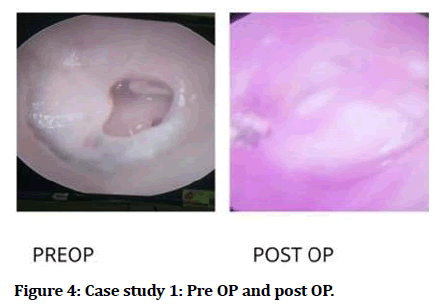
Figure 4: Case study 1: Pre OP and post OP.
Case study 2 (Figure 5)
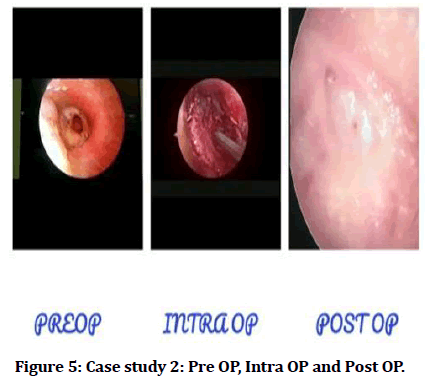
Figure 5:Case study 2: Pre OP, Intra OP and Post OP.
Study groups
Internally, data from 100 randomly selected participants was compared, collated, analysed, and interpreted using descriptive and inferential statistics to meet the study's stated goals. The graft success and failure rates are represented in the Table 1 and Figure 6.
| Study Groups | Graft Successful | Graft failure | Total |
|---|---|---|---|
| Number | 77 | 23 | 100 |
| Percentage | 78 | 22 | 100 |
Table 1: Study groups.
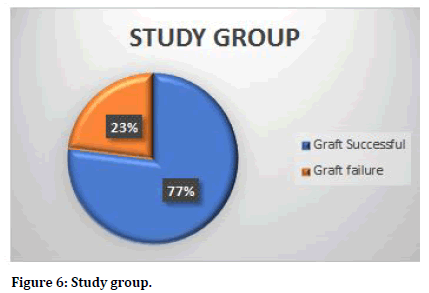
Figure 6:Study group.
The goal of this study is to assess the relevance of ETF in surgical outcome in 100 patients with CSOM (tubotympanic-safe type) inactive stage.
The history, clinical examination, and investigations were all thoroughly examined in each instance.
All patients were treated surgically and medically, and all cases were followed up on.
A proforma was used to collect clinical data, and the observations were analysed using the master chart.
The clinical association between age and post-operative graft status is depicted in the table and bar chart above (Table 2 and Figure 7).
| Age Groups | Graft Successful | % | Graft failure | % | Total | % |
|---|---|---|---|---|---|---|
| 15-20 years | 8 | 10.39 | 3 | 13.04 | 11 | 11 |
| 21-30 years | 31 | 40.26 | 10 | 43.48 | 41 | 41 |
| 31-40 years | 35 | 45.45 | 10 | 43.48 | 45 | 45 |
| 40-45 years | 3 | 3.9 | 0 | 0 | 3 | 3 |
| Total | 77 | 100 | 23 | 100 | 100 | 100 |
| Age Distribution | Graft Successful | Graft failure | Total | |||
| Mean | 19.25 | 5.75 | 25 | |||
| SD | 13.93 | 4.38 | 18.27 | |||
| P value Unpaired t Test | 0.343 | |||||
Table 2: Age.
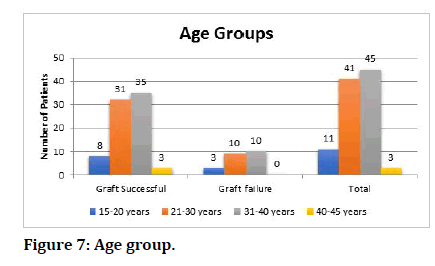
Figure 7:Age group.
Gender
The Table 3 and Figure 8 show the link between gender and post-operative graft status.
| Gender Groups | Graft Successful | % | Graft failure | % | Total | % |
|---|---|---|---|---|---|---|
| Male | 35 | 44.87 | 12 | 52.17 | 47 | 47 |
| Female | 42 | 53.85 | 11 | 47.83 | 53 | 53 |
| Total | 78 | 100 | 23 | 100 | 100 | 100 |
| P value Chi Squared Test | 0.756 | |||||
Table 3: Gender.
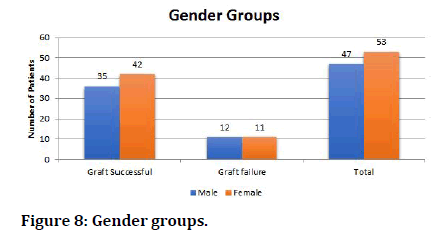
Figure 8:Gender groups.
The Table 4 and pie chart (Figure 9) show the frequency of pneumatisation of the mastoid air cell system in our research group.
| X-Ray mastoid | |
|---|---|
| Well pneumatised | 77 (77%) |
| Poorly pneumatised | 23 (23%) |
| Total | 100 (100%) |
Table 4: X-Ray mastoid.
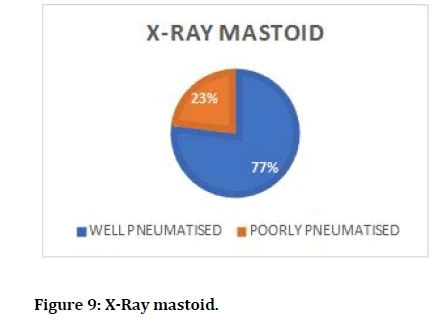
Figure 9:X-Ray mastoid.
The frequency of Eustachian tube activity as measured by Tympanometry in the sample group is shown in the Table 5 and pie chart (Figure 10).
| Tympanometry-ETF test | |
|---|---|
| Normal | 79 (79%) |
| Impaired | 21 (21%) |
| Total | 100 (100%) |
Table 5: Tympanometry-ETF test.
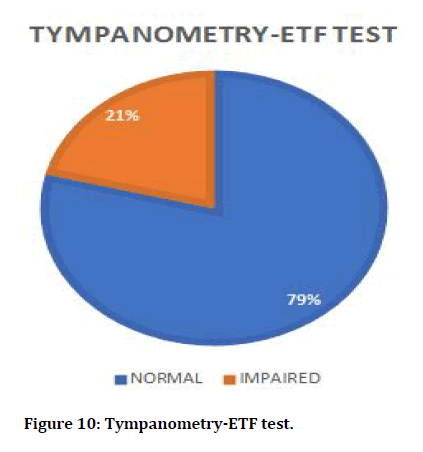
Figure 10:Tympanometry-ETF test.
The frequency of post-operative graft status in our sample group is represented in the Table 6 and pie chart (Figure 11).
| Post op follow up-graft uptake | |
|---|---|
| Taken up | 77 (77%) |
| Perforation | 23 (23%) |
| Total | 100 (100%) |
Table 6: Post op follow up-graft status.
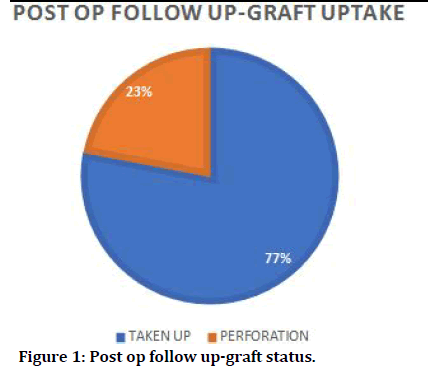
Figure 11:Post op follow up-graft status.
The association between Eustachian tube function and post-operative graft status is depicted in the Table 7 and bar chart (Figure 12).
| Tympanometry-ETF Test | Graft Successful | Graft failure | Total |
|---|---|---|---|
| Normal | 77 (97.47%) | 2 (2.53%) | 79 (100%) |
| Impaired | 0 (0%) | 21 (100%) | 21 (100%) |
| Total | 77 (77%) | 23 (23%) | 100 (100%) |
| P value | <0.001 | ||
| Chi Squared Test | |||
Table 7: Tympanometry-etf test vs post op follow up-graft uptake.
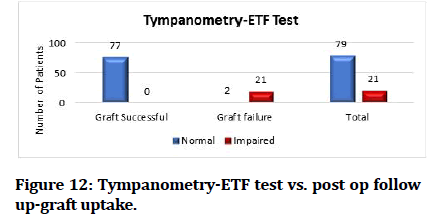
Figure 12:Tympanometry-ETF test vs. post op follow up-graft uptake.
The majority of graft active study participants had normal outcomes (n=77, 97.47 percent), while the majority of graft failure study patients (n=21, 100.00 percent) had impaired results (p=0.001, chi squared test).
When the percentage of normal test results in the graft effective group (97.47%) and graft failure group (2.53%) is compared to the percentage of impaired test results in the graft successful group (0.00%) and graft failure group (0.00%), the difference in the percentage of normal test results in the graft successful group (0.00%) and graft failure group (0.00%) was statistically significant (100%) and later was found to be statistically insignificant (p <0.05).
Discussion
Tympanometry vs. graft uptake
Tympanometry is used to measure ETF in this study. The tympanometric tests indicated that 79 patients out of 100 had normal Eustachian tube function, 2 patients (2.53%) had graft failure, 77 patients (97.47%) had effective graft uptake, and 21 patients (100%) had perforation with significant impairment of Eustachian tube function. The Eustachian tube must work properly in order to keep the middle ear pressure at the same level as the ambient air pressure. This, in turn, is necessary for the middle ear's impedence matching function to work.The impedence audiometer is a more therapeutically reasonable and relevant technique of evaluating ET function because it examines the physiological function of ET, which is more significant to the clinician than just assessing the anatomical patency of the tube, which is attainable with most other methods. Tubal function must be adequate for reconstructive middle ear surgery to be successful.
A trend of significantly higher incidence of normal tympanometry-ETF test status at diagnosis in the graft successful group and significantly higher incidence of impaired tympanometry-ETF test status at diagnosis in the graft failure group. He used impedence audiometry and dye instillation to assess ETF and found a 95.5 percent success rate in patients with normal ETF.
impedance audiometry to quantify ETF and reported an 80% success rate in normal ETF. Patients with normal ETF had an 87 percent success rate in a research done. The treatment had a high percentage of success in restoring healthy eustachian tube function in adults before and after tympanoplasty in a study of eustachian tube function in adults before and after tympanoplasty. As a result, an ETF evaluation should be completed before to surgery to assure a positive outcome.
A follow-up was done one month and three months following surgery. After surgery, patients are examined with otoscopy and otoendoscopy. A research in 2012 that found a 100 percent success rate in patients with normal ETF. Impedance audiometry to assess ETF before surgery in 1979 and found that conventional ETF had a success rate of 95%.
Based on ear results, patients were classified into two groups:
A healed graft was identified as a successful outcome.
Graft failure or perforation was described as failures [11-15].
Conclusion
The eustachian tube is crucial to tympanoplasty success because it is an essential component of normal middle ear function. The following important findings were drawn from outcome comparisons (graft success versus graft failure) following myringoplasty in both normal functioning Eustachian tube and Dysfunction Eustachian tube. The tympanometry-ETF test is a useful tool for determining the functional state of the Eustachian tube, and it appears to have a direct impact on the degree of post-operative graft uptake.
79 patients had normal Eustachian tube function in this study, with 77 patients having a successful outcome with healed grafts and two patients having graft failure with perforation. Perforation of the Eustachian tube in 21 individuals resulted in decreased Eustachian tube function. When compared to patients with defective ETF, patients with normal ETF had a higher success rate of transplant uptake. Effective post-operative graft uptake requires treating the source of Eustachian tube dysfunction. As a result, tubal function testing before to surgery is important in order to get a good Myringoplasty outcome.
References
- Naderpour M, Moghadam YJ, Ghanbarpour E, et al. Evaluation of factors affecting the surgical outcome in tympanoplasty. Iranian J Otorhinolaryngol 2016; 28:99.
- Emir H, Ceylan K, Kizilkaya Z, Gocmen H, et al. Success is a matter of experience: Type 1 tympanoplasty.Eur Arch Otorhinolaryngol 2007; 264:595–599.
- Mohan C, Sharma S, Srivastava A. Has mastoid pneumatization any bearing on tympanoplasty?. Indian J Otol 2015; 21:266-269.
- Holmquist J, Bergström B. The mastoid air cell system in ear surgery. Arch Otolaryngol 1978; 104:127‑9.
- Priya K, Karthikeyan P, Coumare VN, et al. Evaluation ofEustachian tubefunction in chronic suppurative otitis media (tubotympanic type) with reference to its treatment outcome. Indian J Otol 2012; 18:179–183.
- Tarnoom SS, Sridharanarayanan MK. Evaluate the eustachian tube function in chronic suppurative otitis media with reference to its surgical treatment outcome. Annals Romanian Society Cell Biol 2021; 4067-77.
- Srivastava A, Mohan C, Sengar A. How relevant is eustachian tube function in surgical outcome of tympanoplasty?. J Evol Med Dent Sci 2014; 3:1855-9.
- Sato H, Nakamura H, Honjo I, et al. Eustachian tube function in tympanoplasty. Acta Oto-Laryngol 1990; 110:9-12.
- Palva T. Surgical treatment of chronic middle ear disease: 1. Myringoplasty and tympanoplasty. Acta Oto-laryngol 1987; 104:279-84.
- Yoganandh M. Evaluation of eustachian tube function in chronic suppurative otitis media (tubotympanic type) with reference to surgical outcome.Master’s thesis, Madras Medical College, Chennai.
- Prasad KC, Hegde MC, Prasad SC, et al. Assessment of eustachian tube function in tympanoplasty. Otolaryngol Head Neck Surg 2009; 140:889-93.
- Biswas A. Eustachian tube function test: A new dimension in the management of CSOM. Indian J Otolaryngol Head Neck Surg 1999; 51:14-22.
- Sen S, Guha S, Biswas A, et al. A comparative study of methods of evaluation of Eustachian tube functions in chronic otitis media. Indian J Otol 1998; 4:147-9.
- https://www.who.int/pbd/publications/Chronicsuppurativeotitis_media.pdf
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Mohan kumar J* and MK Rajasekar
Department of ENT, Sree Balaji Medical College and Hospital, Chromepet, Chennai, Tamilnadu, IndiaCitation: Mohan kumar J, MK Rajasekar,Evaluation of Eustachian Tube Function in Chronic Suppurative Otitis Media in Relation to Surgical Treatment Results, J Res Med Dent Sci, 2022, 10(1): 623-629
Received: 06-Dec-2021, Manuscript No. JRMDS-21-43945; , Pre QC No. JRMDS-21-43945; Editor assigned: 08-Dec-2021, Pre QC No. JRMDS-21-43945; Reviewed: 22-Dec-2022, QC No. JRMDS-21-43945; Revised: 27-Dec-2021, Manuscript No. JRMDS-21-43945; Published: 03-Jan-2022
