Research - (2021) Volume 9, Issue 9
Evaluation of Effect of Diclofenac Patch for Third Molar Surgeries
Ramvihari Thota* and Senthilnathan Periasamy
*Correspondence: Ramvihari Thota, Department of Oral & Maxillofacial Surgery, Saveetha Dental College, Saveetha Institute of Medical and Technical Science, Saveetha University Tamilnadu, India, Email:
Abstract
Aim: The purpose of this study was to compare the analgesic efficacy of oral diclofenac sodium to diclofenac sodium transdermal patch in the treatment of postoperative pain after surgical removal of impacted mandibular third molars. Materials and methods: 40 patients from saveetha dental college and hospitals of mean age 30 were selected randomly. After completing the first operation on one side, the patients were given diclofenac sodium 100mg once a day for 3 days, and the same patients were given diclofenac sodium transdermal patch 100mg once a day for 3 days after doing the second surgery on the contralateral side. Results: When compared to the medicine delivered trans dermally, diclofenac sodium taken orally shows slightly less significant efficacy on the first postoperative day. However, there was no statistical or clinical difference in pain control between the two routes of administration on the second and third postoperative days. Conclusion: According to the findings, transdermal diclofenac sodium can be utilised as an alternate pain reliever after the removal of impacted mandibular third molars.
Keywords
Diclofenac, Analgesia, Thirdmolar, Transdermal patch, NSAIDs
Introduction
Pain is one of the most common side effects of surgery, and it is a major source of concern for surgeons. It is frequently referred to as a defensive mechanism because it is usually triggered by an environmental change that causes harm to sensitive tissue.
Controlling or eliminating pain is one of the most significant components of dentistry practise. Pain was once so intimately associated with dentistry that the words pain and dentistry were almost interchangeable [1].
Due to the following characteristics, third molar surgical experiences are excellent pain models to study the analgesic efficacy and tolerability of oral analgesics: the procedures are elective; patients are young, healthy, and ambulatory. The treatments are reliable and usually take less than 25 minutes to complete. Patients undergoing third molar extractions are considered a standardised mode for evaluating acute surgical pain, especially those who present with bilaterally similarly impacted lower third molars, which allows two similar surgical procedures to be performed on separate occasions. These patients act as their own controls in cross-over trials. Because an estimated 63.5 percent of patients have significant pain at some point during the first day, oral analgesics are prescribed as standard therapy for at least 24 hours after surgery. Nonsteroidal anti-inflammatory medications (NSAIDs) are effective in reducing mild to moderately severe postoperative pain associated with 3rd molar surgery [2].
Oral, parenteral, inhalation, and transdermal analgesic medications are only a few of the ways they might be administered. The oral route carries the danger of firstpass metabolism, which results in significant medication loss before it is absorbed systemically. Parenteral medication administration can be excruciatingly unpleasant, and a quick spike in drug concentration in the plasma can have unfavourable consequences.
Transdermal administration has the benefit of being a very simple, uncomplicated route of administration without the drawbacks of the other routes described above, as well as having less side effects and difficulties.
This study used diclofenac sodium as a reference medication and gave it via oral and transdermal routes to compare two alternative drug delivery systems in the management of postoperative pain following surgical removal of impacted mandibular third molars.
Local signs of inflammation, including pain, are usually examined after the removal of impacted third molars. This procedure has been widely used as a model for evaluation of analgesic efficacy of various drugs. Postoperative pain after the surgical removal of third molar teeth is a highly sensitive model to evaluate analgesic efficacy of NSAIDs, since the pain is confined to the surgical area with apparent inflammation. The analgesic effects of NSAIDs such as naproxen, meloxicam, rofecoxib, acetaminophen, diflunisal, ibuprofen, ketorolac have been reported using this pain model.
Materials and Methods
Forty healthy subjects belonging to both the sexes in the age group of 18–40 years, without any systemic diseases or previous drug allergy, who presented with bilaterally impacted mesioangular mandibular third molars to the department of Oral and Maxillofacial Surgery, Saveetha Dental College and Hospitals were selected for the study. The selected patients were divided into 2 groups. Group 1- patients treated postoperatively with diclofenac transdermal patch and Group 2- patients treated with diclofenac oral tablets. The patients were informed about the nature and purpose of the study and the likely adverse effects and complications from the drugs being investigated. A written informed consent was obtained from all patients. Preoperative radiographs and routine haematological investigations were also performed.
Analgesics and Antibiotics were administered postoperatively. Following removal of the impacted mandibular third molar on one side the patients were given oral Diclofenac 100mg once daily and when the same patients returned for the surgery on the contralateral side the drug administered was Diclofenac sodium transdermal patch 100mg once daily. The study drugs were administered to the patients 30 minutes prior to the surgery and the sides and drugs were randomly chosen. The teeth were either sectioned or removed in toto. Standardization was maintained by either removing both the teeth in the same patient in toto or both the teeth were sectioned and removed. Of the forty cases in this study, in twenty cases, the teeth were sectioned and removed and in twenty cases the teeth were removed in toto. Oral formulation of diclofenac sodium was used in the dosage of 100mg and was administered once daily for a period of three days.
Four subjective scales were used to record the pain postoperatively. The Visual Analog Scale (VAS) and three others four-point scales. A simple category scale, such as the four points ‘none, mild, moderate and severe’ scale is acceptable for recording pain magnitude but needs numbers to be assigned to each level (0,1,2,3) to quantify the data. The four-point scales used were a Verbal Rating Scale (VRS), a Pain Relief Scale (PRS) and a Pain Intensity Scale (PIS). Further a scale to record any adverse effects was also used. The patients had to assign scores for each parameter at intervals of 2hrs, 4hrs, 8hrs, 12hrs and 24 hrs postoperatively. Further the patients were asked to assign scores for a total of 72 postoperatively.
The VAS provides a simple, efficient, and non-invasive measure of pain intensity that has been used widely in clinical and research settings where a quick index of pain is required and to which a numerical value can be assigned. The VAS consists of a l0 cm horizontal or vertical line with the two endpoints labelled ‘no pain’ and ‘worst pain ever.’ The patient is required to mark the l0 cm line at a point that corresponds to the level of pain intensity he or she presently feels, The distance in centimetres from the low end of the VAS and the patient’s mark is used as a numerical index of the severity of pain.
The Verbal Rating Scale is a four-point scale with values assigned ranging from 0–3. Comfortable, Mild, Moderate and Severe were the corresponding interpretation for the above scores.
The Pain Relief Scale is also a four-point scale, again with values from 0–3. In this scale, the interpretation for the values was complete relief for a score of 0 and no relief for a score of 3.
The Pain Intensity Scale is a scale which is like the Verbal Rating Scale. In this scale, the interpretation for the values was ‘none, mild, moderate and severe’ for corresponding scores between 0–3.
Results
According to the statistical data, transdermal treatment provided considerably greater pain alleviation than oral treatment at the 12-hour interval for the visual analogue scale. The p values obtained indicated that there was no difference in efficacy between the two routes of delivery during the next two days.
According to the statistical data, transdermal delivery provided considerably superior pain alleviation than oral treatment at both the 2 hour and 12-hour intervals on the verbal rating scale. The p values found indicated that there was no difference in pain control between the two routes of administration during the next two days.
The P value for the pain relief scale revealed considerably superior pain relief on transdermal compared to oral delivery at the 2-hour interval, based on statistical data. Over the next two days, there was no statistical difference in the efficacy of either route of administration in terms of p values.
The P value revealed relatively substantial pain alleviation on transdermal compared to oral delivery at the 2nd, 4th, 8th, and 24-hour intervals based on statistical data for the pain intensity scale. Over the next two days, there was no statistical difference in the efficacy of either route of administration in terms of p values.
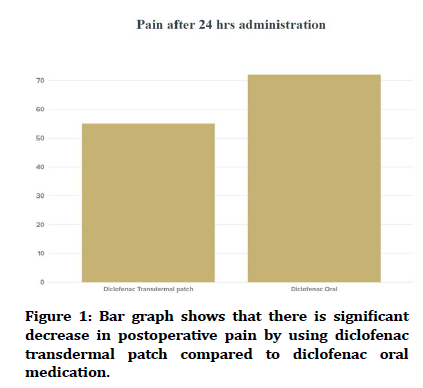
Over the first twenty-four hours, research suggests that diclofenac sodium taken orally is slightly less efficacious than diclofenac sodium delivered trans dermally. On the second and third days, however, there is no statistically significant difference in pain control between the two modes of delivery. Patients did not experience any negative side effects because of any of the operations (Figure 1).
Figure 1. Bar graph shows that there is significant decrease in postoperative pain by using diclofenac transdermal patch compared to diclofenac oral medication.
Discussion
Patients typically associate dental care with pain, and a bad dental treatment experience can cause patients to avoid or postpone treatment, as well as make them more difficult to treat [3].
Third molar extraction is a common procedure in oral and maxillofacial surgery. It is critical to get anaesthetic during the procedure, but appropriate postoperative analgesia is also critical for appropriate patient care [3,4]. Third molar tooth impaction is a typical problem that demands their extraction [5]. A popular model for testing the efficacy of analgesics for acute dental pain is surgical removal of an impacted third molar [3].
It is widely recognised that pain following the extraction of third molars is brief and peaks in intensity in the early postoperative period [5]. After third molar surgery, most young, healthy adults should anticipate having some symptoms and be limited in their activities for 5 days or less. Interference with daily activities, work, and school may be limited for the first three days following surgery, with discomfort reducing significantly over the next five days [6].
Because the surgical methods for both sides are the same, the individuals who will be investigated are the same, the depth and degree of impaction will be the same, and the pain perception will be the same, bilaterally symmetrical impacted mandibular third molars are a useful mode of comparison, the impacted mandibular third molars provide an opportunity to perform two similar surgical procedures on two different occasions because the parameters assessed will be the same bilaterally symmetrical impacted mandibular third molars provide an opportunity to carry out two similar surgical procedures on two different occasions because the parameters assessed will be the same.
Pain is one of the most experienced symptoms in surgery and as such is a major concern to the surgeon. It is often spoken of as a protective mechanism, since it is usually manifested when an environmental change occurs that causes injury to responsive tissue One of the most important aspects of the practice of dentistry is the control or elimination of pain. In the past, pain has been so closely associated with dentistry that the words pain and dentistry have become almost synonyms [1].
The third molar surgical experiences are desirable pain models to evaluate the analgesic efficacy and tolerability of oral analgesics due to the following characteristics: the surgeries are elective; patients are young and healthy and ambulatory. The performed procedures are consistent and are generally completed within 25 minutes. Patients undergoing removal of third molars, are considered standardized mode for the evaluation of acute surgical pain and especially those who present with bilaterally similar impacted lower third molars provide an opportunity to carry out two similar surgical procedures on separate occasions such patients act as their own controls in cross over trials. An estimated 63.5% of patients experience severe pain at sometime during the first day for this reason oral analgesic is provided as standard care for postoperative time periods for at least 24 hours. Non-steroidal anti-inflammatory drugs work well to relieve mild to moderate intense postoperative pain caused by 3rd molar surgery [2].
The contribution of non-steroidal anti-inflammatory drugs (NSAIDs) in the alleviation of pain cannot be underestimated. Right from the commonly used acetaminophen that affords relief by its antipyretic and analgesic effects in our day to day lives to diclofenac also commonly used for acute and musculoskeletal pain, the role of these drugs is indispensable. Though many adverse effects are commonly associated with the use of NSAIDs, these tools have to be applied at the right time with the right method to sculpt a pain free and comfortable experience for the patient. It has been documented that the most common adverse effect with the use of NSAIDs by either oral or parenteral route is the gastric irritability that occurs secondary to the inhibition of the protective effects of cyclooxygenase 1.1,2 The introduction of the transdermal drug delivery system gives a solution to the question of achieving a therapeutic concentration without producing undesirable side effects. This route of administration differs from the traditional topical administration in that, after penetration of the skin barrier, the drug enters the circulation to be distributed systemically.3 The major advantage of transdermal route is the constant drug dosage that is available and maintained in the circulation due to its sustained release properties.4,5 Thus a stable concentration is maintained systemically without concentrated higher doses in the gastrointestinal system, the hepatic metabolism is also bypassed [6].
Diclofenac sodium is a nonselective cyclooxygenase enzyme inhibitor belonging to the oxicam group with balanced cyclooxygenase inhibition and excellent tolerability with earlier research that found diclofenac sodium to be a long-acting agent with a half-life period of 8–12 hours. NSAIDs reduce prostaglandin production by inhibiting cyclooxygenase enzyme activity, thereby reducing the local inflammatory response and peripheral sensitization of nociceptors [5]. Diclofenac sodium, which is an NSAID with analgesic and antipyretic activities, inhibits prostaglandin synthesis [6]. It is among the most extensively used NSAIDs and is prescribed in rheumatoid arthritis, osteoarthritis, bursitis, ankylosing spondylitis, toothache, dysmenorrhea, renal colic, and posttraumatic and postoperative inflammatory conditions [6-10]. Adverse effects of diclofenac sodium are generally mild epigastric pain, nausea, headache, dizziness, and rashes and rarely gastric ulceration and earache. As postoperative pain after surgical extraction of third molars is moderate to severe, pain relief or control is often challenging to achieve. However, this condition offers an opportunity to study and evaluate the potency of analgesics in validated clinically relevant models. Various NSAIDs are being used after third molar extractions for pain relief. Diclofenac sodium have been studied with different drugs for postoperative analgesia in dentistry, but data are limited on the comparative effect of diclofenac sodium transdermal patches for pain control after surgical extraction of third molars in the Indian population.
The surgical removal of mandibular third molars serve as a standard model for any research pertinent to analgesia. 7 This is due the fact that surgical removal of third molars cause pain due to both incisional and inflammatory injury, thus eliciting both peripheral and central response. Also, with the surgical removal of mandibular third molars, standardization is possible to reduce the bias caused by the level of surgical difficulty.
Patients typically associate dental care with pain and an experience of poorly managed pain related to dental treatment can lead patients to avoid or postpone treatment, as well as make them more difficult to treat. Third molar removal represents a major part of oral and maxillofacial surgical practice. It is essential that anaesthesia be obtained during removal, but effective postoperative analgesia is equally important for good patient care [5]. The concentration of prostaglandins in acutely injured tissue reaches its maximum level at 3 or 4 h after injury with the result of a peak intensity of postoperative pain.
Impaction of third molar teeth is a common disorder which often necessitates their removal [6]. Surgical removal of an impacted third molar is a model used commonly to test the efficacy of analgesics for acute dental pain [4]. It is well documented that pain after removal of third molars is of short duration and reaches its maximum intensity in the early postoperative period [6]. Most young, healthy adults may expect to experience some symptoms and limitation of activity for 5 days or less after third molar surgery. Interference with routine activities and work and school may be expected to be restricted to the first 3 days after surgery, with pain decreasing steadily over the first 5 days.
Bilaterally symmetrical impacted mandibular third molars are a useful mode of comparison because the surgical procedures for both the sides remain the same, the individuals who will be studied are the same, the depth and degree of impaction will be the same, the pain perception also remains the same, since the parameters assessed will be the same bilaterally symmetrical impacted mandibular third molars provide an opportunity to carry out two similar surgical procedures on two different occasions.
Analgesic drugs can be administered in a variety of routes, including oral, parenteral, inhalation as well as transdermal. Oral route carries the risk of first pass metabolism and loss of substantial quantities of the drug before it is absorbed systemically. Parenteral administration of drugs can be extremely painful and sudden increase in drug concentration in the plasma could lead to certain adverse effects. Transdermal administration has the advantages of being a very easy, simple route of administration without the disadvantages of the routes mentioned above and also comparatively fewer side effects and complications.
NSAIDs have the capacity to reduce both pain and inflammation, making them effective analgesics for pain management following surgical excision of mandibular third molar impactions. Surgical tooth extraction causes a common type of pain that peaks during the extraction time and then subsides to mild levels [7]. In that regard, anaesthesia is crucial during the procedure of surgical removal of mandibular third molars; however, proper pain control is also vital in the immediate postoperative period, as the pain from surgical removal of third molars reaches its maximal level during this time. We standardised the procedure's difficulty level, operator variability, and patient inclusion and exclusion criteria in this study.
Bhaskar et al [8] in his study, they also found that diclofenac transdermal patches were well accepted by the patients, with only two patients reporting gastric irritation and nausea after taking oral diclofenac tablets. In a meta-analysis by Mason et al [9] topical NSAIDs have been demonstrated to have no significant gastrointestinal side effects or an increased risk of renal failure. Also, in a study by Naesdal et al. [10] because topical NSAIDs have lower systemic concentrations, overall gastrointestinal problems such as ulcer and dyspepsia have been demonstrated to be statistically considerably lower. Apart from the discomforts, patients who received transdermal drug administration showed improved compliance and were excited about the potential of pain treatment without the need for oral drugs, as seen in the earlier trial by Bhaskar et al [8].
The comparative analgesic efficacy trial was conducted on 20 patients undergoing surgical excision of bilateral mesioangularly impacted mandibular third molars using the medication diclofenac sodium, 100 mg as a reference.
On the immediate postoperative day, statistical study and clinical observation show that diclofenac sodium delivered orally gives slightly less analgesia than diclofenac sodium delivered trans dermally. However, no clinical or statistical differences were seen on the second and third postoperative days.
Conclusion
Given the evidence of its established analgesic effectiveness with a lower frequency of systemic adverse effects, the transdermal diclofenac patch appears to be a potential analgesic modality for the management of mild to moderate pain following tooth extractions. Transdermal diclofenac therapy, possibly with a stronger analgesic medication in the transdermal patch, may have a role to play in post-traumatic pain. Longer clinical studies with a bigger sample size are needed, however, before the true scope of the transdermal diclofenac patch for surgical tooth extractions can be determined. According to the findings, transdermal diclofenac sodium can be utilised as an alternate pain reliever after the removal of impacted mandibular third molars.
Acknowledgement
None.
Funding
No funding to declare.
References
- Oʼneill R. Monheimʼs local anaesthesia and pain control in dental practice. Pain 1985; 22:101.
- Zuniga JR, Phillips CL, Shugars D, et al. Analgesic safety and efficacy of diclofenac sodium softgels on postoperative third molar extraction pain. J Oral Maxillofac Surg 2004; 62:806–815.
- Pozos-Guillen A, Martinez-Rider R, Aguirre-Banuelos P, et al. Pre-emptive analgesic effect of tramadol after mandibular third molar extraction: A pilot study. J Oral Maxillofac Surg 2007; 65:1315–1320.
- Bailey BMW, Zaki G, Rotman H, et al. A double-blind comparative study of soluble aspirin and diclofenac dispersible in the control of postextraction pain after removal of impacted third molars. Int J Oral Maxillofac Surg 1993; 22:238–241.
- Meechan JG, Seymour RA. The use of third molar surgery in clinical pharmacology. Br J Oral Maxillofac Surg 1993; 31:360–365.
- Shugars DA, Benson K, White RP, et al. Developing a measure of patient perceptions of short-term outcomes of third molar surgery. J Oral Maxillofac Surg 1996; 54:1402–1408.
- Yamashita Y, Sano N, Shimohira D, et al. A parallel-group comparison study of celecoxib with loxoprofen sodium in third mandibular molar extraction patients. Int J Oral Maxillofac Surg 2014; 43:1509–1513.
- Bhaskar H, Kapoor P, Ragini. Comparison of transdermal diclofenac patch with oral diclofenac as an analgesic modality following multiple premolar extractions in orthodontic patients: A cross over efficacy trial. Contemp Clin Dent 2010; 1:158–163.
- Mason L, Moore RA, Edwards JE, et al. Topical NSAIDs for acute pain: A meta-analysis. BMC Fam Pract 2004; 5:10.
- Naesdal J, Brown K. NSAID-associated adverse effects and acid control aids to prevent them: A review of current treatment options. Drug Saf 2006; 29:119–132.
Author Info
Ramvihari Thota* and Senthilnathan Periasamy
Department of Oral & Maxillofacial Surgery, Saveetha Dental College, Saveetha Institute of Medical and Technical Science, Saveetha University Tamilnadu, Chennai, IndiaCitation: Ramvihari Thota, Senthilnathan Periasamy, Evaluation of Effect of Diclofenac Patch for Third Molar Surgeries, J Res Med Dent Sci, 2021, 9(9): 94-98
Received: 14-Aug-2021 Accepted: 06-Sep-2021