Research - (2021) Volume 9, Issue 5
Evaluation of Beta-Tri Calcium Phosphate as Bone Substitute Materials for Ridge Preservation after Extraction Procedure (Comparative Study)
Shahbaa Ahmed Hadi and Sahar Shakir Al-Adili*
*Correspondence: Sahar Shakir Al-Adili, Department of Oral and Maxillofacial Surgery, Collage of Dentistry, University of Baghdad, Iraq, Email:
Abstract
Background: Bucco-lingual alveolar ridge collapse and significant ridge atrophy because of physiologic bone remodeling may continue up to 12 months’ post-extraction.
Bone substitute with suitable graft material and barrier membrane immediately after tooth extraction is most predictable way in ridge preservation. A synthetic graft, pure phase β-tricalcium phosphate, has been documented in human and animal studies to be resorbed and replaced by vital bone after 4 months with CBCT examination, in addition to resorbable collagen membrane for better stabilization.
In addition to preserve the ridge volume the clinical observations revealed excellent soft tissue healing without loss of attached gingiva.
Aims of the study: 1-To evaluate the effect of bio absorbable bone graft Material (B-tri calcium phosphate) with a collagen membrane to preserve the alveolar ridge dimensions following tooth extraction and to compare the results with unassisted alveolar sockets. 2-To evaluate the effect of the B-TCP on the bone density of post extraction–sockets by CBCT and to compare the density of cancellous bone formed between study and control groups.
Materials and Methods: This prospective clinical study took place at Department of Oral and Maxillofacial Surgery, College of Dentistry, Included 21 Patients 8 Male and 13 females with 38 extracted teeth. Age range of 22-60 years with a mean age (42.86 ± 10.57) participants were divided into two groups, , study group in which the B-TCP bone graft material was placed inside a fresh extraction socket and control group conducted without bone grafting. The patients' age, sex, number of teeth, oral hygiene state was recorded. CBCT X-Ray image were taken before extraction, both groups had simple non-traumatic teeth extraction, then with study group preparation of about 0.5 mg of B –TCP according to socket size, mix it with normal saline and gently adapt into the socket with condensation, cover with a resorbable collagen membrane and suturing for better stabilization. The suture was removed at 8 -10 days. After 4 months’ new bone formed in the socket measured by CBCT. Data description, analysis and presentation were performed using Statistical Package for social Science (SPSS version 21, Chicago, IL, USA) Statistical analyses.
Results: Of the 38 extracted teeth ,20 grafted teeth with bone graft and 18 was free from graft. There was a significant increase in bone density through 4 months Post-operatively in study group (1372.325 ± 133.216) compare with control group (505.907 ± 377.185). Alveolar socket height loss was reducing post -operatively in study group than control group (7.935 ± 2.194 versus7.372 ± 1.753) respectively, but with not statically difference between two groups. Regarding width loss, there were a significant difference in reduce width loss post operatively in study than control (5.082 ± 1.324 versus 3.981 ± 0.979).
Conclusion: In this study, the Quantity of bone formation in the form of linear measurement of Bone width and height exhibited noticeable preservation of the extraction socket and reduction of the degree of alveolar bone loss in ßTCPCol group. when the ridge dimensions at 4 months compared with those at base line with favorable results to ßTCP-Col study group over control group after complete healing of the extraction socket B-TCP show promising effect on accelerating the bone density of post –extraction sockets after 4 months.
Keywords
Beta-tri calcium phosphate, Alveolar bone, Calcium phosphate ceramics, ß-TCP
Introduction
Alveolar bone seems to play a key role in providing support to the teeth, which are anchored to the bone by periodontal ligament. After tooth extraction and because of a physiological bone resorption, the encirclement bones no longer induce by root and go immediately to shrink and collapse. In addition to the severity of the healing pattern, the clinician may pose an esthetic problem in the fabrication of a conventional prosthesis or implant-supported restoration [1].
Furthermore, about 40% - 60% of socket height and width respectively is expected to be lost within first year after extraction. the goal is to is to preserve the quality and the quantity of the osseous tissues and gingiva without any significant problem’s creation [2].
Several techniques and Methods of stabilizing the bone, thereby reducing the extent of the resorption process, include the insertion of suitable biomaterial and membrane immediately after extraction, this is considering the most reliable and predictable way for reduce bone resorption into the alveolar cavity for alveolar ridge preservation (ARP) [3,4].
Bone grafting is the main treatment modality for reconstruction and repair of bone defect and replace the volumetric bone loss in oral and maxillofacial fields [5].
Bone grafting is possible because the ability of bone tissue to regenerate completely if provided enough space for it to grow into, with time when natural bone grow it completely replaces the graft material. The result fully integrated area of new bone [6], auto grafts, allografts, xenografts, and alloplasts has been used as bone graft, the ideal graft material should have specific attributes. it should be osteoinductive, osteoconductive, and biocompatible. It’s important to be totally replaced by host bone that have appropriate resorption time in relation to new bone formation, also maintain graft volume stability with satisfactory mechanical properties.
Alloplastic represent synthetic bone graft which are more widely used, one of the most promising groups of them is calcium phosphate ceramics, in the form of beta tricalcium phosphate (β-TCP) is commonly used [4].
ß-TCP is commonly preferred as a biomaterial for its chemical stability, mechanical strength, and bio resorption properties.it also osteoconductive, biocompatible material in both animal and clinical studies. after implantation in the extracted socket, It will resorbed within 3-6 months by osteoclastic cell and by chemical dissolution of body fluids provide calcium and magnesium ion that create ionic environment which activate alkaline phosphatase as it important for bone formation and in addition to provide space for bone formation [7,8]. (b-TCP) was first reported in 1920 by Albee, the chemical formula of Ca3(PO4)2, b-TCP has Ca/P ratio of 1.5 that more rapidly resorbed than HA and interconnected porous structures for bony replacement and fibro vascular invasion [9]. In other hand ß-TCP has unpredictable.
In this present study, use of ß-TCP as a bone substitute and after 4 months it will be biodegrading and be replaced by new bone without fibrous tissue proliferation when it uses immediately after tooth extraction.
The use of GBR represented by collagen membrane in flapless socket preservation can prevent soft tissue invasion inside the socket and prevent the escape of graft material out the socket [10].
Materials and Methods
This prospective observational clinical study included patients, who attended the Department of Oral and Maxillofacial Surgery at the College of Dentistry, University of Baghdad for tooth extraction.in the period between December 2019 to September 2020.
Twenty –one patients (13 females and 8 males), age ranged from (22-60) years (mean of 42.86 ± 10.57) with badly carious anterior tooth.
The inclusion criteria included: healthy individuals without any systemic disease and with no local pathological lesion at the peri apical area, patient’s age ≥ 20 years.
A total 38 extracted teeth were divided into two groups, the study group include 20 teeth in which fresh extracted socket filled with B-TCP bone graft material plus resorbable collagen membrane.
The control group include 18 patients in which the fresh extracted sockets were left to heal normally without application of graft material. The project of the study was approved by the Ethical Committee of the College of Dentistry/ University of Baghdad (reference no. 35 in 9/1/2019). All patients were informed about the nature of the study and they signed a written consent form for their participation in this study.
Extraction procedure and preparation of B-TCP
Before tooth extraction, all patients presented a clinically healthy periodontium. Patient was asked to rinse with chlorhexidine 0.12% for two minutes [11].
Surgical procedures were performed under local anesthesia without flap elevation that to minimize surgical trauma and preserve vascularization.
After extraction, the sockets were carefully debrided with fine curettes to remove all soft tissue remnants and granulation tissue, then copious rinsing with sterile saline in case of socket filled with graft material (study group) [12], while in control group the sockets healed spontaneously without any debridement of soft tissue and without any graft materials also with no sutures. (natural physiological healing).
In study group the sockets were completely filled with β-TCP, layer by layer with spoon excavator that after mix graft material with normal saline and with spoon excavator fill the entire socket in order to occupy all the volume of the socket up to the level of the surrounding host bone, addition with condense the particle by condenser, care taken not to overfill the socket just up to 2 mm apical to the soft tissue margin as this could result in subsequent sequestration of the exposed coronal granules or displacement of the entire graft mass after mechanical irritation during the first phases of healing [13].
The socket then covered with a hemostatic dressing material (collagen membrane), The membrane was formed in a way to overlap the sockets margins by 2-3mm and placed slightly below the marginal mucosa. with cross-mattress tension suture was placed over to maintain soft tissue stability and to hold over the membrane in place [14].
Radiological method
99 CBCT measurement were done at baseline before extraction, because of bone defect margin remained clearly discernable so easy to measure socket width and height (Figure 1) [15] and after 4 months’ interval after grafting material using the software program tools, at the same reference point and lines [16,17].
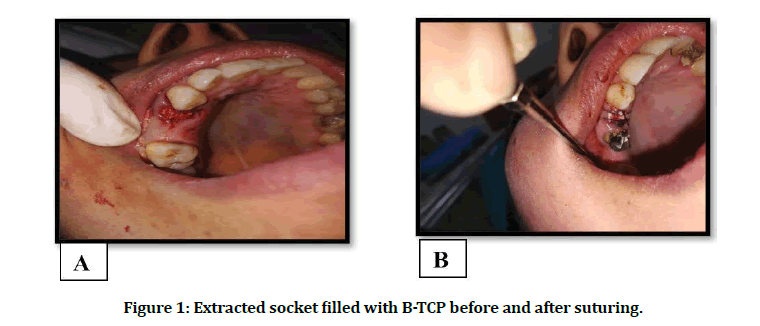
Figure 1: Extracted socket filled with B-TCP before and after suturing.
99 From the reconstructed image of CBCT software program we choose an OPG (panoramic view) to detect the cross-sectional trans axial view (Figure 2).
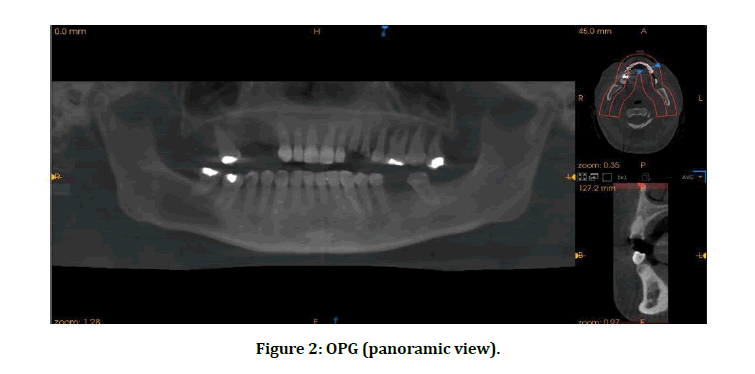
Figure 2: OPG (panoramic view).
99 Two horizontal line was drawn, one from the lowest outer point on crestal surface of alveolar bone buccally and lingually or palatally of tooth socket (line A). Another line was drawn parallel to line A passing through the most apical point in the tooth socket (line B) (Figure 3A).
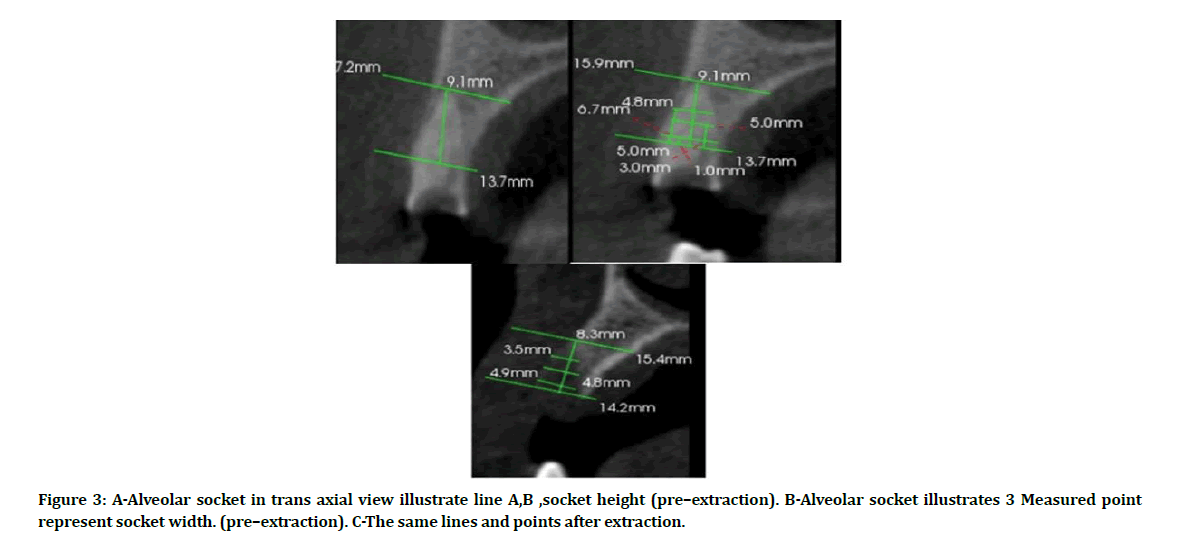
Figure 3: A-Alveolar socket in trans axial view illustrate line A,B ,socket height (pre–extraction). B-Alveolar socket illustrates 3 Measured point represent socket width. (pre–extraction). C-The same lines and points after extraction.
99 A vertical reference line was drawn from line A to line B bisecting the tooth in its center, this represents the height of the socket (Figure 3A).
99 Three horizontal reference lines down at 1,3,5 mm starting from crestal bone parallel to line A, these lines represent the width of socket at 3 points (Figure 3B).
99 After 4 months, the measurement of width of socket in 1,3,5, were re measured and compared with first measurement in each group and between two groups (Figure 3C).
99 The vertical line (socket height) also re measured after 4 months and compare with the first measurements in each groups and also between two groups (Figure 3C).
99 The bone density (VV)was measured in areas at 1, 3, 5 horizontal lines to evaluate the bone calcification after 4 months between two groups (Figure 3C) [18].
Statistical analysis
Data description, analysis and presentation were performed using Statistical Package for social Science (SPSS version 21, Chicago, IL, USA) Statistical analyses.
Descriptive statistical analysis included calculation of mean ± standard deviation (SD) and inferential analysis included Independent sample –t-test used to test the difference between two groups. and the probability value <0.05 was considered.
Results
Twenty-five patients, 8 males (38.10%) and 13females (61.90) with an age range of 22-60 and a mean age (± SD) 42.86 ± 10.57 years participated in this study, with a total of 38 extracted teeth, divided randomly into two groups (study and control), 20 extracted teeth assisted with bone graft and 18 unassisted extracted teeth.
The mean height changes post -operatively was (7.935 ± 2.194) in study group than (7.372 ± 1.753) in control group. But the differences between the two groups was statistical non significance (p >0.05) (Table 1).
Table 1: Calculated statistical differences for changes in ridge height over 4months in both groups
| Groups | Independent sample T test | Df | P value | ||
|---|---|---|---|---|---|
| Study Mean±SD |
Control Mean±SD |
||||
| After 4 months post oprativaly | 7.935±2.194 | 7.372±1.753 | 0.867 | 36 | 0.392 NS |
The mean ridge width changes at the three levels (1,3,5) below the crest in both groups post – operatively, represent in mean ± SD in study group versus control group (5.645 ± 1.465 vs 4.417 ± 1.035), (5.030 ± 1.339 vs 4.089 ± 0.978), (4.570 ± 1.389 vs 3.439 ± 1.155) with statistically significant (p< 0.05).
The total width mean in study group was 5.082 ± 1.324 than control group 3.981 ± 0.979 post- operatively. All these result with statistically significant (p< 0.05) (Table 2).
Table 2: Calculated statistical differences for changes in ridge width over 4 months in both groups.
| Groups | Independent sample T test | DF | P value | ||
|---|---|---|---|---|---|
| Study Mean±SD |
Control Mean±SD |
||||
| 1mm | 5.645±1.465 | 4.417±1.035 | 2.953 | 36 | 0.006sig |
| 3mm | 5.030±1.339 | 4.089±.978 | 2.451 | 36 | 0.019sig |
| 5mm | 4.570±1.389 | 3.439±1.155 | 2.711 | 36 | 0.010sig |
| Mean | 5.082±1.324 | 3.981±.979 | 2.885 | 36 | 0.007sig |
Post- operatively, the bone density measured at the three levels (1,3,5) below the crest in both groups represent in mean ± SD in study group versus control group, (1739.550 ± 176.220 vs 570.833 ± 450.615), (1683.750 ± 233.210 vs 507.056 ± 431.441), (1347.150 ± 360.090 vs 513.389 ± 379.226). The mean postoperative bone density measured in study group 1372.325 ± 133.216 VV, compared with the mean bone density in control group 505.907 ± 377.185 VV, the differences between the groups reached statistical significance (p < 0.005) (Table 3).
Table 3: Comparison between studies groups in bone density using independent sample t- test.
| Groups | Independent sample T test | Df | P value | ||
|---|---|---|---|---|---|
| Study Mean±SD |
Control Mean±SD |
||||
| Desity 1mm | 1739.550± 176.220 |
570.833± 450.615 |
10.736 | 36 | 0.000 Sig. |
| Density 3mm | 1683.750± 233.210 |
507.056± 431.441 |
10.606 | 36 | 0.000 Sig. |
| Density 5mm | 1347.150± 360.090 |
513.389± 379.226 |
6.950 | 36 | 0.000 Sig. |
| Density mean | 1372.325± 133.216 |
505.907± 377.185 |
9.639 | 36 | 0.000 Sig. |
Discussion
Digitalization with CBCT software analysis offer significant benefits in visible marginal bone demonstration with better accuracy, but still there is a possible source of errors for bone modeling in detection of incomplete mineralize bone. However, CBCT facilitate dimensional measurement better than clinical measurement [19].
Alveolar process shows significant greater resorption after extraction especially in buccal plate than lingual or palatal during healing period as a part of normal physiological bone resorption [20] in his study clarified that buccal plate consists mainly of bundle bone which it completely removed during extraction, later replace with woven bone during bone remodeling. with time, volumetric changes occurred which is more obvious in width reduction than height in this research, the healing fallow up period was 4 months, that Most of the dimensional alterations – horizontal as well as vertical of the alveolar ridge took place during this time, the condition of the healed alveolar bone has a significant effect on the assessment of the outcomes. According to [21] that at the first three months of healing most of the bone resorption process occurs, mainly due to the resorption of the buccal bone plate but the dimensional changes can be observed up to 1 year or more after tooth extraction. B-TCP has an osteo conductive property which result in good bone growth and enhances healing process [22]. Furthermore, B-TCP graft material of particles size between 7-10 μm, show acceptable resorbable/ degradable and maintain mechanical properties with excellent results [23].
In this study, pure phase of B-TCP was used in a granular form size measure 0.5-1mm in extracted socket. clinically observed that the alveolar socket shows adequate mechanical stability and provide structural integrity in the grafted site without any complications and uneventful, satisfactory soft tissue healing.
Radiographically, there was a considerable limitation in the amount of alveolar socket height loss in grafted socket as compare with unassisted socket. These results were close to the outcome mentioned by [19] who used B-TCP as bone graft right after extraction and compare the results with control group in 3 and six months after extraction, ARP with β-TCP led to significantly reduction in alveolar bone resorption was detected in alveolar bone height in compression with control group.
Moreover, with the use of b-TCP with resorbable collagen membrane in study group, there was significant reduction in the bucco-lingual width loss than control group, B-TCP has biocompatible property which bond directly to bone, slow –down the shrinkage correlated with healing. The Resorbable cross-linked collagen membrane used shows biocompatibility with soft tissue and B-TCP graft material, in which there was no sign of infection or inflammation with good clinical outcomes of wound tissue healing without recorded any complications in clinical examination 4 months post operatively, in addition to its biodegradation property with Less ridge width loss and more bone infill than untreated control socket.
Hong et al. [24] clarified that the use of collagen membrane over the B-TCP bone graft material for better stabilization of graft material, came with better preservation of bone height, width and thickness of keratinize tissue. These outcomes were supported by another study conducted by Elsaid et al. [25] who compare between two groups, the first group socket filled with B-tcp graft material plus collagen membrane, the second one socket filled Platelet Rich Fibrin (PRF) and compare the results clinically and with CBCT image. the socket filled with B-tcp /collagen came with significant result in width preservation over PRF group.
Radiographically, density changes diagnosis was based on degree of the brightness and darkness of images, which expressed with gray scale value in CBCT and with Hounsfield Unit in CT scan in which there are a strong correlation between HU value and gray scale value with no significant different [26]. Voxel value was used in this study for measured bone density. The results of the current study indicated that there was high bone density formed in the socket of study group as compared to the control group after 4-month healing period this due to biological effect of B-TCP as bone graft material plus collagen membrane. there was an early osseous regeneration in study group compare to control group. B- TCP has an osteoconductive property act as scaffold for bone grows on a surface, support the bone healing process, with prevention of collapse in the augmented region.
Calcium phosphate (Ca-P) in the form of tricalcium phosphate (β-TCP) which is a bioactive biocompatible and osteoconductive material can build a resorbable -interlocking chain in the defect site led to improve bone healing and bone growth, highest number of phosphorous ions and calcium was released by T-CP due to its faster degradation that’s lead to increase in new bone formation in graft site [27]. This outcome was supported by other study done by [28] who determines the efficiency of (βTCP) resorbable bone graft in new bone deposition with better densities of the regenerated bone by two methods of analysis, Histopathological examination on 5 rabbit and Radio graphical measures on 30 patients.
Regard age and gender, with advance age there is great variation in bone remodeling, reduced bone regeneration and formation due to gradual reduction of tissue metabolism and decrease in healing process [29]. Females seem to be more exhibition to hormone imbalance throughout the life than males. this opinion came in agreement with Mascarenhas et al. [30] who confirmed that Sexual hormones have an important role in influencing progression of periodontal disease and wound healing. The Limitations of this study related to Small sample size. and Short follow up period that does not include a long-term assessment of complete resorption of graft material.
Conclusion
Ridge preservation with B -TCP and a resorbable collagen membrane is useful in maintaining ridge dimension after tooth extraction and reduces the need for future ridge augmentation before dental implant placement. B -TCP show promising effect on accelerating the bone density of post –extraction sockets after 4 months.
References
- Al-Fhdawi, L.S., 2015. Tooth Socket Preservation Using Beta Tricalcium Phosphate (β-TCP) Clinical and Experimental Studies. Al-Anbar Medical Journal, 12(1).
- Bronstein, M., Nappe, C., Villavicencio, J., Toro, H. and Guiñez, H., 2016. Preservation of alveoli by beta tricalcium phosphate, with and without membrane. Clinical journal of periodontics, implantology and oral rehabilitation, 9 (2), pp. 168-174.
- Bhatt, A.K. and Pandey, V.A.P.M., 2015. Alveolar Ridge Preservation with beta-tricalcium phosphate Bone Graft and Implant Placement: A Case Report. IJSS Case Reports & Reviews, 1, pp.28-31.
- Elsaid, M.A.E., El-Awady, A.A., Edrees, M.F. and Hosny, M.M., 2020. Clinical and Radiographic Evaluation of Fresh Socket Grafting using Beta-tri-calcium Phosphate with Collagen and Platelet-Rich Fibrin for Receiving Dental Implant. Al-Azhar Assiut Dental Journal, 3(2), pp.121-128.
- Fairbairn, P., Leventis, M., Mangham, C. and Horowitz, R., 2018. Alveolar Ridge Preservation Using a Novel Synthetic Grafting Material: A Case with Two-Year Follow-Up. Case reports in dentistry, 2018.
- Helmy, M.A., 2017. Review of Socket Preservation Technique. EC Dental Science, 14, pp.07-14
- Horowitz, R.A., Mazor, Z., Foitzik, C., Prasad, H., Rohrer, M. and Palti, A., 2010. β-tricalcium phosphate as bone substitute material: properties and clinical applications. Journal of Osseointegration, 2(2), pp.61-68
- Hong, H.R., Chen, C.Y., Kim, D.M. and Machtei, E.E., 2019. Ridge preservation procedures revisited: A randomized controlled trial to evaluate dimensional changes with two different surgical protocols. Journal of periodontology, 90(4), pp.331-338.
- Iskaros, M., Silver, J., Blye, J. and Cardenas, M., 2017. Does B-Tricalcium Phosphate Work as a Bone Regenerative Material. J Dent Oral Biol, 2, pp.1106-1109.
- Jambhekar, S., Kernen, F. and Bidra, A.S., 2015. Clinical and histologic outcomes of socket grafting after flapless tooth extraction: a systematic review of randomized controlled clinical trials. The Journal of prosthetic dentistry, 113(5), pp.371-382.
- Jamjoom, A. and Cohen, R.E., 2015. Grafts for ridge preservation. Journal of functional biomaterials, 6(3), pp.833-848.
- Jung, R.E., Sapata, V.M., Hämmerle, C.H., Wu, H., Hu, X.L. and Lin, Y., 2018. Combined use of xenogeneic bone substitute material covered with a native bilayer collagen membrane for alveolar ridge preservation: A randomized controlled clinical trial. Clinical oral implants research, 29(5), pp.522-529. -
- Jung, R.E., Philipp, A., Annen, B.M., Signorelli, L., Thoma, D.S., Hämmerle, C.H., Attin, T. and Schmidlin, P., 2013. Radiographic evaluation of different techniques for ridge preservation after tooth extraction: a randomized controlled clinical trial. Journal of clinical periodontology, 40(1), pp.90-98
- Kamaruddin, N., Rajion, Z.A., Yusof, A. and Aziz, M.E., 2016, December. Relationship between Hounsfield unit in CT scan and gray scale in CBCT. In AIP Conference Proceedings (Vol. 1791, No. 1, p. 020005). AIP Publishing LLC.
- Kang, H.J., Makkar, P., Padalhin, A.R., Lee, G.H., Im, S.B. and Lee, B.T., 2020. Comparative study on biodegradation and biocompatibility of multichannel calcium phosphate based bone substitutes. Materials Science and Engineering: C, 110, p.110694.
- Kumar, P., Vinitha, B. and Fathima, G., 2013. Bone grafts in dentistry. Journal of pharmacy & bioallied sciences, 5(Suppl 1), p. S125.
- Lee, J., Lim, Y.J., Kim, B., Koo, K.T. and Lee, Y.M., 2020. Biphasic Calcium Phosphate Sphere Graft Combined with a Double-Layer Non-Crosslinked Collagen Membrane Technique for Ridge Preservation: A Randomized Controlled Animal Study. Materials, 13(1), p.18.
- Leventis, M.D., Fairbairn, P., Kakar, A., Leventis, A.D., Margaritis, V., Lückerath, W., Horowitz, R.A., Rao, B.H., Lindner, A. and Nagursky, H., 2016. Minimally invasive alveolar ridge preservation utilizing an in situ hardening β-tricalcium phosphate bone substitute: a multicenter case series. International Journal of Dentistry, 2016.
- Loveless, T.P., Kilinc, Y., Altay, M.A., Flores-Hidalgo, A., Baur, D.A. and Quereshy, F.A., 2015. Hounsfield unit comparison of grafted versus non-grafted extraction sockets. Journal of oral science, 57(3), pp.195-200.
- Mascarenhas, P., Gapski, R., Al‐Shammari, K. and Wang, H.L., 2003. Influence of sex hormones on the periodontium. Journal of clinical periodontology, 30(8), pp.671-681.
- Min, S., Liu, Y., Tang, J., Xie, Y., Xiong, J., You, H.K. and Zadeh, H.H., 2016. Alveolar ridge dimensional changes following ridge preservation procedure with novel devices: Part 1–CBCT linear analysis in non‐human primate model. Clinical oral implants research, 27(1), pp.97-105.
- Pellegrini, G.G., Mattiuzzi, A.S., Pellegrini, M.A., Corso, L.A., Morales, C.P.C., Osinaga, E.A. and Zeni, S.N., 2018. Update on Bone Grafting Materials Used in Dentistry in the Bone Healing Process: Our Experience from Translational Studies to Their Clinical Use. Bone Grafting: Recent Advances with Special References to Cranio-Maxillofacial Surgery, p.73.
- Rodella, L.F., Favero, G. and Labanca, M., 2011. Biomaterials in maxillofacial surgery: membranes and grafts. International journal of biomedical science: IJBS, 7(2), p.81.
- Sabe-Alarab, M., Shomal, Y., Jaber, F. and Harba, A.N., 2019. Alveolar ridge preservation with β-TCP a randomized controlled trial.
- Schnutenhaus, S., Götz, W., Dreyhaupt, J., Rudolph, H., Luthardt, R.G. and Edelmann, C., 2020. Associations among Primary Stability, Histomorphometric Findings, and Bone Density: A Prospective Randomized Study after Alveolar Ridge Preservation with a Collagen Cone. Dentistry journal, 8(4), p.112.
- van Beek, J.H., Kirkwood, T.B. and Bassingthwaighte, J.B., 2016. Understanding the physiology of the ageing individual: computational modelling of changes in metabolism and endurance. Interface Focus, 6(2), p.20150079.
- Vanhoutte, V., Rompen, E., Lecloux, G., Rues, S., Schmitter, M. and Lambert, F., 2014. A methodological approach to assessing alveolar ridge preservation procedures in humans: soft tissue profile. Clinical Oral Implants Research, 25(3), pp.304-309.
- Wang, R.E. and Lang, N.P., 2012. Ridge preservation after tooth extraction. Clinical oral implants research, 23, pp.147-156.
- Wang, W. and Yeung, K.W., 2017. Bone grafts and biomaterials substitutes for bone defect repair: A review. Bioactive materials, 2(4), pp.224-247.
- Xia, Y., Xie, L., Zhou, Y., Song, T., Zhang, F. and Gu, N., 2015. A new method to standardize CBCT for quantitative evaluation of alveolar ridge preservation in the mandible: a case report and review of the literature. Regenerative biomaterials, 2(4), pp.251-260.
Author Info
Shahbaa Ahmed Hadi and Sahar Shakir Al-Adili*
Department of Oral and Maxillofacial Surgery, Collage of Dentistry, University of Baghdad, IraqCitation: Shahbaa Ahmed Hadi, Sahar Shakir Al-Adili, Evaluation of Beta-Tri Calcium Phosphate as Bone Substitute Materials for Ridge Preservation after Extraction Procedure (Comparative Study), J Res Med Dent Sci, 2021, 9 (5):105-111.
Received: 27-Apr-2021 Accepted: 10-May-2021 Published: 17-May-2021
