Research - (2020) Advances in Dental Surgery
Evaluation of Association between Dietary Habits and Temporomandibular Joint Disorders
Nur Liyana Hannah BintiIzham Akmal1, Santhosh Kumar MP1* and Revathi Duraisamy2
*Correspondence: Santhosh Kumar MP, Department of Oral and Maxillofacial Surgery, Saveetha Dental College,Saveetha Institute of Medical and Technical Science, Saveetha University, Chennai, India, Email:
Abstract
Temporomandibular joint disorders (TMD) are often characterized by impaired function of the Temporomandibular joint (TMJ) and the associated neuromuscular system, which often leads to TMD-related pain. It involves a group of clinical conditions affecting the masticatory muscles, TMJ and other associated structures such as capsule and articular discs. Chewing and dietary habits are often considered as the factors stimulating the onset of TMD with many TMD patients complaining of pain around the area of TMJ following the intake of hard foods. The aim of this study was to evaluate the association of dietary habits of patients with temporomandibular joint disorders (TMD) and its effects on the development of TMD. This retrospective study was conducted by reviewing the case records of 86,000 dental patients reported to Saveetha Dental College and Hospital, Chennai, India from June 2019 to March 2020. About 104 cases were included in the study by a simple random sampling method. These included 52 patients with temporomandibular disorder, and 52 patients without temporomandibular disorder. Patient’s name, patient’s identification number (PID), age, gender and dietary habits were collected from the patients’ case records. Data collected were analyzed using the SPSS version 23.0 and results obtained. Descriptive analysis was done, and categorical variables were expressed in frequency and percentage. Chi square test was used to evaluate the association between dietary habits and TMD. P value < 0.05 was considered statistically significant. Majority of the patients were on a mixed diet (65.38%) and the rest of them were vegetarian (34.62%). Prevalence of TMD was seen slightly higher in males (51.92%) compared to females (48.08%). Most of the TMD cases were observed in individuals within the 31-40 years age group (46.15%). A statistically significant association was present between dietary habits and TMD [p=0.039 (<0.05)]. Within the limits of the present study, temporomandibular disorders (TMD) showed higher predilection in males, within 31-40 years of age and in mixed diet patients. The association between dietary habits and temporomandibular joint disorders were statistically significant.
Keywords
Diet, Food habits, Temporomandibular disorders, Temporomandibular joint
Introduction
The ability of temporomandibular joints (TMJ) to function properly highly depends on the balance and harmony of the different structures of TMJ such as condyles, glenoid fossa and ligaments [1]. Any distortion to the normal structure of TMJ by external factors such as psychological factors and habits may lead to the impairment of TMJ function. The ability of the human body to recover helps to repair any damage to the TMJ and prevent its progression but if this condition persists beyond the ability for repair, the body will lose its ability to recover and eventually leads to the development of severe conditions such as temporomandibular joint disorders (TMD) with various signs and symptoms [2].
It has been reported previously that the prevalence of temporomandibular joint and muscle disorder varies between 5% and 12% with higher incidence of TMD observed in younger individuals which was considered unusual for chronic pain conditions [3]. In terms of gender, it is reported that the prevalence of TMD in females is at least twice that of males with higher risk seen in females who consume supplemental estrogen or oral contraceptives. Similarly, a recent study also reported that TMD accounts for 25% of the population with up to 11% in chronic pain [4]. TMD is considered as the second most common chronic pain condition with a prevalence of 5% to 12% in the general population and only musculoskeletal lower back pain has a greater prevalence [5].
Temporomandibular joint disorders (TMD) are often characterized by impaired function of the TMJ and the associated neuromuscular system, which often leads to TMJ-related pain [2,6]. It involves a group of clinical conditions affecting the masticatory muscles, TMJ and other associated structures such as capsule and articular discs [6-8]. Various etiologies are described in the study of TMD such as trauma, systemic factor, iatrogenic factor, and mental health disorders [9-15]. Previous studies suggested morphologic malocclusions and parafunctional habits as part of the causes of TMD [16,17]. It has also been reported that psychosocial functioning, stress, depression, and multiple somatic symptoms may lead to the development of TMD [2,6,18].
Chewing and dietary habits are often considered as the factors stimulating the onset of TMD [19- 23]. Various cases of TMD have reported on patient’s complaints of pain around the area of TMJ following the intake of hard foods [24] Others studies have mentioned that the texture and hardness of foods may affect the movement of TMJ and influence the level of masticatory muscle activity [19-21]. Prolonged mastication of hard foods may result in masseter muscle pain, impaired masticatory laterality, and displacement of the mandibular condyle over period [23,25-27].
TMD are often characterized by numerous signs and symptoms such as musculoskeletal orofacial pain, TMD pain or both, which can be observed in all populations [28,29]. Other studies also mentioned the presence of orofacial and preauricular pain, as well as restricted mouth opening, TMD bruit during function and displacement of articular disc as some of the signs and symptoms of TMD. Orofacial pain may affect the daily activities of an individual with TMD, particularly in terms of psychological condition which further leads to chronic pain and improper eating disorder [30-32]. The presence of TMD along with impaired eating habits and psychological problems faced by an individual may increase the severity of the initial condition. It is important to evaluate the association between TMD signs and symptoms and the ability of a TMD patient to consume food to understand the level of impairment experienced by an individual with TMD [33].
One of the common concerns of individuals with TMD is a change in their diet, which affects the quality and quantity of the food that they consume in order to minimize the pain associated with TMD [34-38]. Many TMD patients have also reported on the intake of medication to reduce TMD symptoms such as pain and discomfort, along with the consumption of soft foods such as porridge and soup, which require less chewing in order to reduce the severity of TMD pain [39-41]. However, most of the TMD patients tend to focus solely on the food texture instead of the nutritional contents of the food that they consume, which eventually leads to other health problems such as improper digestion, weight gain or loss, lack of energy and mental health problems [34,37,42,43]. If these conditions persist over a period, an individual with TMD may experience bigger problems involving their overall health and quality of life [8,44,45]. This study was done to evaluate the association of dietary habits of individuals with TMD and its effects on the development of TMD.
Materials and Methods
Study design and study setting
This retrospective cross-sectional study was conducted in Saveetha dental college and hospital, Saveetha university, Chennai, to evaluate the association between dietary habits and temporomandibular joint disorders among dental patients reporting to outpatient department of oral and maxillofacial surgery from June 2019 to March 2020. The study was initiated after approval from the institutional review board.
Study population and sampling
Among 86000 dental patients reported to our institution from June 2019 to March 2020, about 104 cases were included in the study by a simple random sampling method to minimise sampling bias. These included 52 patients with temporomandibular disorder, and 52 patients without temporomandibular disorder. All missing or incomplete data, nutritionally debilitated patients and patients with severe systemic illnesses were excluded from the study. Each patient's dental records, treatment reports and photographs were reviewed thoroughly. Cross verification of data for errors was done with the help of an external examiner.
Data collection and tabulation
A single calibrated examiner evaluated the digital case records of the patients collected from June 2019 to March 2020 who reported with and without TMJ disorders and reviewed their dietary habits. Information on the patients’ name, age, gender, dietary habits and presence of TMD were collected from the patients’ case records. Age of the patients were categorized for statistical convenience as 11-20, 21-30, 31-40, 41-50 and 51-60. Patients’ dietary habits were classified into a mixed diet and vegetarian diet.
Statistical analysis
The collected data was validated, tabulated and analysed with Statistical Package for Social Sciences for Windows, version 23.0 (SPSS Inc., Chicago, IL, USA) and results were obtained. Descriptive analysis was done to assess the prevalence of TMD in different age groups and gender. Categorical variables were expressed in frequency and percentage, and continuous variables in mean and standard deviation. Chisquare test was used to test association between dietary habits and TMD. P value < 0.05 was considered statistically significant.
Results and Discussion
In our study, among 104 patients, there were an equal number of patients with TMDs (n=52) and without TMDs (n=52). Our study showed that the prevalence of TMD was slightly higher in males (51.92%) compared to females (48.08%) (Figure 1). Most of the cases with TMD in our study are seen in individuals within the 31-40 years age group (46.15%) while those within the 51-60 years age group showed the least prevalence for TMD (7.69%) (Figure 2).
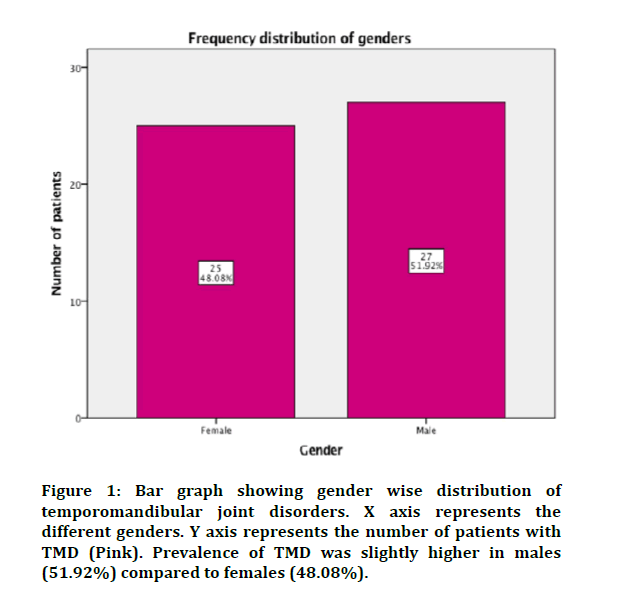
Figure 1: Bar graph showing gender wise distribution of temporomandibular joint disorders. X axis represents the different genders. Y axis represents the number of patients with TMD (Pink). Prevalence of TMD was slightly higher in males (51.92%) compared to females (48.08%).
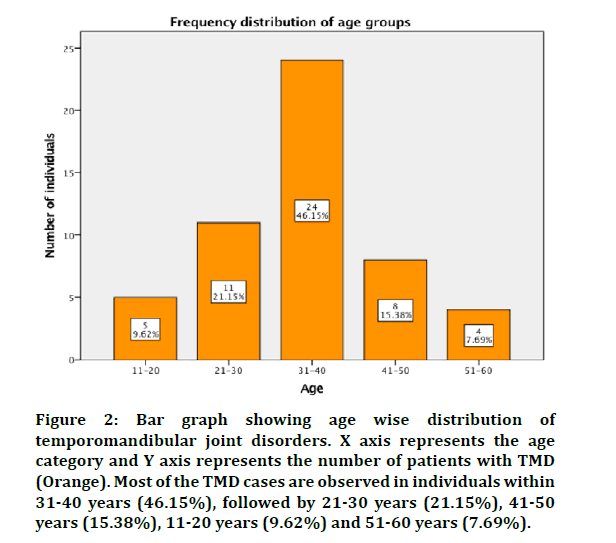
Figure 2: Bar graph showing age wise distribution of temporomandibular joint disorders. X axis represents the age category and Y axis represents the number of patients with TMD (Orange). Most of the TMD cases are observed in individuals within 31-40 years (46.15%), followed by 21-30 years (21.15%), 41-50 years (15.38%), 11-20 years (9.62%) and 51-60 years (7.69%).
Majority of individuals in our study presented a mixed diet (65.38%) while the rest of them were vegetarians (34.62%) (Figure 3). In our study shows that there is no statistically significant association between diet and TMD (p>0.05). The association between dietary habits and TMD was evaluated. TMD was predominantly present in patients on mixed diet than on vegetarians and the results were statistically significant. [Pearson’s chi square value - 4.248, df -1; p=0.039 (<0.05)] (Figure 4).
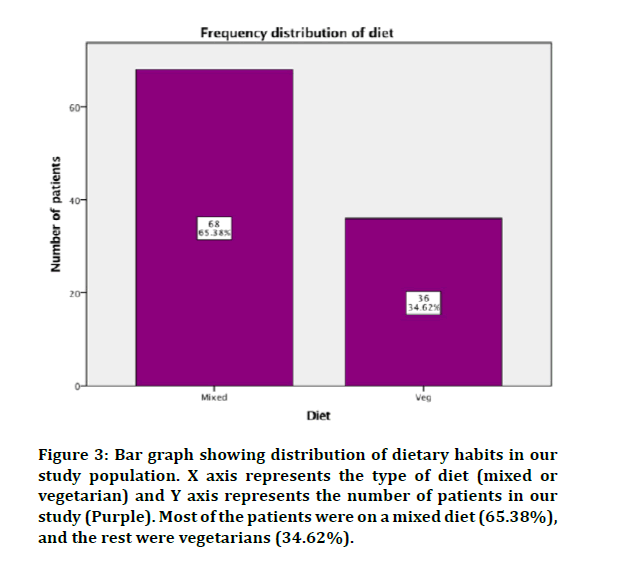
Figure 3: Bar graph showing distribution of dietary habits in our study population. X axis represents the type of diet (mixed or vegetarian) and Y axis represents the number of patients in our study (Purple). Most of the patients were on a mixed diet (65.38%), and the rest were vegetarians (34.62%).
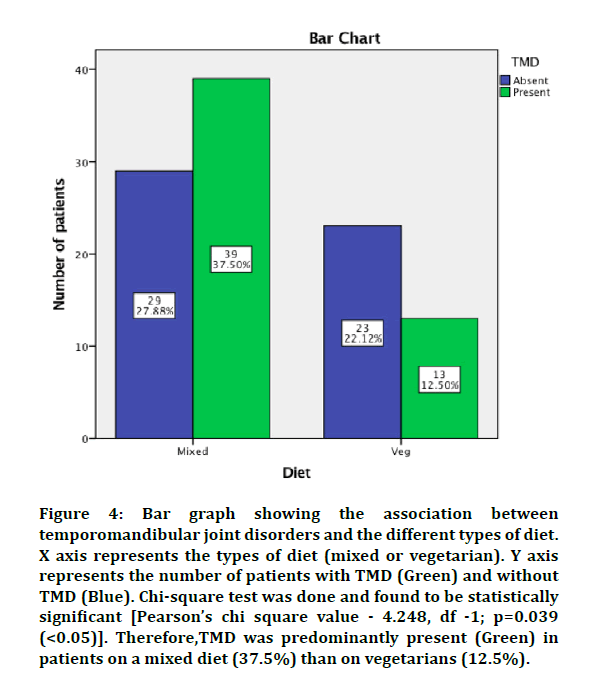
Figure 4: Bar graph showing the association between temporomandibular joint disorders and the different types of diet. X axis represents the types of diet (mixed or vegetarian). Y axis represents the number of patients with TMD (Green) and without TMD (Blue). Chi-square test was done and found to be statistically significant [Pearson’s chi square value - 4.248, df -1; p=0.039 (<0.05)]. Therefore,TMD was predominantly present (Green) in patients on a mixed diet (37.5%) than on vegetarians (12.5%).
Our study showed that the prevalence of TMD was slightly higher in males (51.92%) compared to females (48.08%). Akhter et al. revealed a significant association between gender and TMD with TMJ pain being more common in males compared to females. However, another study concluded that no significant relationship is observed between males and females regarding TMD disorders [27]. Another study by AlShaban et al. reported most of the TMD cases in their study are seen in males (65%) compared to females (35%), which is similar to the finding by Lee et al who reported the predominance of male with TMD [46,47]. Some studies have clearly shown the predominance of female with TMD which is associated with pubertal development, but the diagnosis remains unknown [48-51]. This is further supported by Shet et al. who reported that females (60.4%) have a significantly higher prevalence of TMD signs than males (39.6%), which is associated with biological, psychosocial, and hormonal differences between the two groups [52].
Most of the cases with TMD in our study are seen in individuals within the 31-40 years age group (46.15%) while those within the 51-60 years age group showed the least prevalence for TMD (7.69%). A study by AlShaban et al. revealed a maximum percentage of TMD patients between the age ranges of 19-29 (58%) and the minimum is between the age ranges of 60-69 (1%) [46]. A study by Akhter et al reported on the significant relationship between age and TMJ pain, which is commonly observed in older individuals [27]. While Karibe et al. described that TMD symptoms are commonly reported in middleaged individuals, rather than in children; with TMD symptoms being age-dependent among adults who are 20-70 years old [53].
Our study showed that there was a statistically significant association between dietary habits and TMD. TMD was predominantly present in patients on mixed diet than on vegetarians and the results were statistically significant. In contrary, a study by Akhter et al reported that there is no significant association between TMD clinical signs and dietary habits, although they agreed that dietary habits may contribute to the symptoms of TMD, especially TMJ pain which may be potential risk factors for TMD [27]. This is further supported by previous studies which mentioned the correlation of severity of masticatory muscle pains with biting hard foods as the activity of masticatory muscles and TMJ increases in relation to food hardness and texture [26,54,55].
According to AlShaban et al. the results in their study stated that most patients consume hard diet (56%) which could be a contributing factor in cause the disorders as shown in previous related studies [46]. It is believed that masticating hard foods induce displacement of TMJ causes pain by increasing the activity of masticatory muscles which leads to change in the dietary habits by taking softer foods that requires less chewing to minimize pain [34]. This explains the prevalence of TMD in patients with mixed diet compared to those with vegetarian diet in our study.
The present study had few limitations of study design. Since it is a retrospective study, follow up of subjects was not possible to extrapolate the study results. This study also failed to assess the other confounding variables such as education and socioeconomic status of the patients. Further prospective study including all possible factors for TMD has to be investigated to prove the hypothesis.
One of the primary concerns of TMD patients is the change in the quality and quantity of food intake to minimize pain which is one of the main symptoms of TMD. Further advancement in diagnosis and newer preventative measures are believed to be helpful in reducing the risk of TMD development. Future studies should include clinical examination of these associations to help in better understanding of the condition.
Conclusion
Within the limits of the present study, temporomandibular disorders (TMD) showed higher predilection in males, within 31-40 years of age and in mixed diet patients. The association between dietary habits and temporomandibular joint disorders were statistically significant.
Acknowledgement
We would like to thank Saveetha Dental College and Hospital for the contributions and involvement through this study.
Conflict of Interests
There was no conflict of interest.
References
- Marimuthu M, Andiappan M, Wahab A, et al. Canonical WNT pathway gene expression and their clinical correlation in oral squamous cell carcinoma. Indian J Dent Res 2018; 29:291–297.
- Schiffman E, Ohrbach R, Truelove E, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: Recommendations of the international RDC/TMD consortium network and orofacial pain special interest group. J Oral Facial Pain Headache 2014; 28:6–27.
- Prevalence of TMJD and its signs and symptoms. National Institutes of Health. 2008.
- Shephard MK, Macgregor EA, Zakrzewska JM. Orofacial pain: A guide for the headache physician. Headache 2014; 54:22–39.
- Safour W, Hovey R. A phenomenologic study about the dietary habits and digestive complications for people living with temporomandibular joint disorders. J Oral Facial Pain Headache 2019; 39:377–388.
- Bagheri SC. Reconstructive oral and maxillofacial surgery. Clin Review Oral Maxillofac Surg 2008; 263–302.
- Langendoen J, Müller J, Jull GA. Retrodiscal tissue of the temporomandibular joint: clinical anatomy and its role in diagnosis and treatment of arthropathies. Man Ther 1997; 2:191–198.
- Miloro M. Peterson’s principles of oral and maxillofacial surgery. PMPH-USA 2004; 1800.
- Wieckiewicz M, Boening K, Wiland P, et al. Reported concepts for the treatment modalities and pain management of temporomandibular disorders. J Headache Pain 2015; 16:106.
- Kobs G, Bernhardt O, Kocher T, et al. Oral parafunctions and positive clinical examination findings. Stomatologija 2005; 7:81–83.
- Kijak E, Lietz-Kijak D, Sliwiński Z, et al. Muscle activity during rehabilitation of masticatory motor system functional disorders. Postepy Hig Med Dosw 2013; 67:507–516.
- Liu F, Steinkeler A. Epidemiology, diagnosis, and treatment of temporomandibular disorders. Dent Clin North Am 2013; 57:465–479.
- Miettinen O, Lahti S, Sipilä K. Psychosocial aspects of temporomandibular disorders and oral health-related quality-of-life. Acta Odontologica Scandinavica 2012; 70:331–336.
- Manfredini D, Borella L, Favero L, et al. Chronic pain severity and depression/somatization levels in TMD patients. Int J Prosthodont 2010; 23:529–534.
- Bono AE, Learreta JA, Rodriguez G, et al. Stomatognathic system involvement in rheumatoid arthritis patients. CRANIO®. 2014; 32:31–37.
- List T, Wahlund K, Larsson B. Psychosocial functioning and dental factors in adolescents with temporomandibular disorders: A case-Control study. J Orofac Pain 2001; 15:218–227.
- Winocur E, Gavish A, Finkelshtein T, et al. Oral habits among adolescent girls and their association with symptoms of temporomandibular disorders. J Oral Rehabil 2001; 28:624–629.
- Packiri S, Gurunathan D, Selvarasu K. Management of paediatric oral ranula: A systematic review. J Clin Diagn Res 2017; 11:ZE06–ZE09.
- Peyron MA, Maskawi K, Woda A, et al. Effects of food texture and sample thickness on mandibular movement and hardness assessment during biting in man. J Dent Res 1997; 76:789–795.
- Peyron MA, Lassauzay C, Woda A. Effects of increased hardness on jaw movement and muscle activity during chewing of visco-elastic model foods. Exp Brain Res 2002; 142:41–51.
- Horio T, Kawamura Y. Effects of texture of food on chewing patterns in the human subject. J Oral Rehabil 1989; 16:177–183.
- Kurita H, Ohtsuka A, Kurashina K, et al. Chewing ability as a parameter for evaluating the disability of patients with temporomandibular disorders. J Oral Rehabil 2001; 28:463–465.
- Komiyama O, Asano T, Suzuki H, et al. Mandibular condyle movement during mastication of foods. J Oral Rehabil. 2003; 30:592–600.
- Dworkin SF, Huggins KH, LeResche L, et al. Epidemiology of signs and symptoms in temporomandibular disorders: Clinical signs in cases and controls. J Am Dent Assoc 1990; 120:273–281.
- Mizumori T, Tsubakimoto T, Iwasaki M, et al. Masticatory laterality--evaluation and influence of food texture. J Oral Rehabil 2003; 30:995–999.
- Shiau YY, Peng CC, Wen SC, et al. The effects of masseter muscle pain on biting performance. J Oral Rehabil 2003; 30:978–984.
- Akhter R, Hassan NMM, Nameki H, et al. Association of dietary habits with symptoms of temporomandibular disorders in Bangladeshi adolescents. J Oral Rehabil 2004; 31:746–753.
- Abhinav RP, Selvarasu K, Maheswari GU, et al. The patterns and etiology of maxillofacial trauma in South India. Ann Maxillofac Surg 2019; 9:114–117.
- Santhosh Kumar MP. Relationship between dental anxiety and pain experience during dental extractions. Asian J Pharm Clin Res 2017; 10:458–461.
- Kumar S, Sneha S. Knowledge and awareness regarding antibiotic prophylaxis for infective endocarditis among undergraduate dental students. Asian J Pharma Clin Res 2016; 9:154-159.
- Santhosh Kumar MP. The emerging role of botulinum toxin in the treatment of orofacial disorders: Literature update. Asian J Pharm Clin Res 2017; 10:21–29.
- Sweta VR, Abhinav RP, Ramesh A. Role of virtual reality in pain perception of patients following the administration of local anesthesia. Ann Maxillofac Surg 2019; 9:110–113.
- Christabel A, Anantanarayanan P, Subash P, et al. Comparison of pterygomaxillary dysjunction with tuberosity separation in isolated Le Fort I osteotomies: a prospective, multi-centre, triple-blind, randomized controlled trial. Int J Oral Maxillofac Surg 2016; 45:180–185.
- Touger-Decker R. Approaches to oral nutrition health risk screening and assessment. Nutrition Oral Med 2014; 351–367.
- Savoca MR, Arcury TA, Leng X, et al. Impact of denture usage patterns on dietary quality and food avoidance among older adults. J Nutr Gerontol Geriatr 2011; 30:86–102.
- Mobley CC, Dounis G. Dietary guidance for people wearing removable prostheses. J Am Dent Assoc 2013; 144:11–15.
- Yang SE, Park YG, Han K, et al. Dental pain related to quality of life and mental health in South Korean adults. Psychol Health Med 2016; 21:981–992.
- Raphael Kg M. Dietary fiber intake in patients with myofascial face pain. J Orofac Pain 2002; 16:39–47.
- Rao TD, Santhosh Kumar MP. Analgesic efficacy of paracetamol vs ketorolac after dental extractions. Res J Pharm Technol 2018; 11:3375.
- Vijayakumar Jain S, Muthusekhar MR, Baig MF, et al. Evaluation of three-dimensional changes in pharyngeal airway following isolated lefort one osteotomy for the correction of vertical maxillary excess: A Prospective Study. J Maxillofac Oral Surg 2019; 18:139–146.
- Jesudasan JS, Abdul Wahab PU, Muthu Sekhar MR. Effectiveness of 0.2% chlorhexidine gel and a eugenol-based paste on postoperative alveolar osteitis in patients having third molars extracted: a randomised controlled clinical trial. Br J Oral Maxillofac Surg 2015; 53:826–830.
- Patturaja K, Pradeep D. Awareness of basic dental procedure among general population. Res J Pharm Technol 2016; 9:1349.
- Patil SB, Durairaj D, Suresh Kumar G, et al. Comparison of extended nasolabial flap versus buccal fat pad graft in the surgical management of oral submucous fibrosis: A prospective pilot study. J Maxillofac Oral Surg 2017; 16:312–321.
- Rahman R SK. Knowledge, attitude, and awareness of dental undergraduate students regarding human immunodeficiency virus/acquired immunodeficiency syndrome patients. Asian J Pharm Clin Res 2017; 10:175–180.
- Santhosh Kumar, M.P., Rahman R. Knowledge, awareness, and practices regarding biomedical waste management among undergraduate dental students. Asian J Pharm Clin Res 2017; 10:341–345.
- AlShaban KK, Waheed ZGA. Prevalence of TMJ disorders among the patients attending the dental clinic of ajman university of science and technology–fujairah campus, UAE. Int J Dent 2018; 2018:1–6.
- Lee JY, Kim YK, Kim SG, et al. Evaluation of Korean teenagers with temporomandibular joint disorders. J Korean Assoc Oral Maxillofac Surg 2013; 39:231–237.
- Ebrahimi M, Dashti H, Mehrabkhani M, et al. Temporomandibular disorders and related factors in a group of iranian adolescents: A cross-sectional survey. J Dent Res Dent Clin Dent Prospects 2011; :123–127.
- Fernandes G, Franco-Micheloni AL, Siqueira JTT, et al. Parafunctional habits are associated cumulatively to painful temporomandibular disorders in adolescents. Br Oral Res 2016; 30.
- B. Murad NG, Sepah B, Rehman B, et al. Parafunctional habits among undergraduate clinical students and house officers at khyber college of dentistry. J Khyber College Dent 2016; 6:20-24.
- Bahrani F, Ghadiri P, Vojdani M. Comparison of temporomandibular disorders in Iranian dental and nondental students. J Contemporary Dent Practice 2012; 13:173–177.
- Shet RGK, Yadav RD, Rao S, et al. Prevalence of temporomandibular joint dysfunction and its signs among the partially edentulous patients in a village of north Gujarat. J Contemporary Dent Practice 2013; 14:1151–1155.
- Karibe H, Shimazu K, Okamoto A, et al. Prevalence and association of self-reported anxiety, pain, and oral parafunctional habits with temporomandibular disorders in Japanese children and adolescents: A cross-sectional survey. BMC Oral Health. 2015; 15:8.
- Plesh O, Bishop B, McCall W. Mandibular movements and jaw muscles’ activity while voluntarily chewing at different rates. Exp Neurol 1987; 98:285–300.
- Steiner JE, Michman J, Litman A. Time sequence of the activity of the temporal and masseter muscles in healthy young human adults during habitual chewing of different test foods. Archives Oral Biol 1974; 19:29–34.
Author Info
Nur Liyana Hannah BintiIzham Akmal1, Santhosh Kumar MP1* and Revathi Duraisamy2
1Department of Oral and Maxillofacial Surgery, Saveetha Dental College,Saveetha Institute of Medical and Technical Science, Saveetha University, Chennai, India2Department of Prosthodontics, Saveetha Dental College,Saveetha Institute of Medical and Technical Science, Saveetha University, Chennai, India
Citation: Nur Liyana Hannah Binti Izham Akmal, Santhosh Kumar MP, Revathi Duraisamy, Evaluation of Association Between Dietary Habits and Temporomandibular Joint Disorders, J Res Med Dent Sci, 2020, 8 (7): 291-297.
Received: 29-Sep-2020 Accepted: 02-Nov-2020 Published: 09-Nov-2020
