Research - (2021) Volume 9, Issue 2
Endodontic Periodontal Lesion Diagnosis and Treatment Decision Analysis
Keerthika R and Nivedhitha MS*
*Correspondence: Nivedhitha MS, Department of Conservative dentistry and Endodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical And Technical Sciences, Saveetha University Tamilnadu, India, Email:
Abstract
The relationship between periodontal and endodontic disease has been a controversial aspect for more than a century. Differentiating between these periodontal and endodontic disease is very difficult due their developmental, embryonic, anatomic and functional similarities. Nature pain is often considered as the first clue which should be supported by the radiographic and clinical evaluation for the correct diagnosis of the condition. The aim of this review was to develop a decision tree for easier and accurate diagnosis of periodontal and endodontic disease. A brief pubmed search was performed on endodontic and periodontal lesion using “MESH” terms “endo-perio lesion”, “diagnosis of endo perio lesion”,” decision making of endo-perio lesion”. In addition some websites and local guidelines were screened. By following the correct and appropriate diagnostics methods ,accurate diagnosis of Endodontic -Periodontal disease can be done and the treatment for the particular condition could be achieved. With a decision tree, the diagnosis and pharmacological management of the pulpal and periapical diseases becomes easier for the dentist in regular clinical practice. A decision tree and a flow chart for daily practice which should be started up as soon as the patient presents with pain or swelling due to pulpal or periodontal periapical pathology. In this aspect active management of the infection can be done with sound knowledge on the endodontic periodontal lesions.
Keywords
Endoperio lesion, Periodontal, Pulpal, Diagnosis, Treatment plan
Introduction
Skin and soft tissue infections (SSTIs) have variable etiology and clinical presentation and is commonly seen in both in ambulatory and hospital The interrelation between the pulp and the periodontium are very difficult to understand and also have been a controversial topic over years which could be owed to their developmental, embryonic, anatomic and functional similarities [1,2]. It was first described by Simring et al. [3]. Differentiating the disease being a pulpal or periodontal origin presents various challenges due to the complexity in the communicating pathways between the pulp and the periodontium [3,4]. The endodontic and periodontal lesion is closely interrelated presenting both the signs of pulpal and periodontal involvement which makes their diagnosis quite complex. The disease can be a result of one or other or even can be from two different unrelated processes which gets related with the advancement of disease. Diagnosing the disease is the most challenging aspect of this disease which requires deeper knowledge and insight into subject [5].
We have numerous highly cited publications on well-designed clinical trials and lab studies [6-21]. This has provided the right platforms for us to pursue the current study. Thus the aim of this review was to develop a decision tree for easier and accurate diagnosis of periodontal and endodontic diseases.
Classification
Based on the primary cause of the disease, Simon et al. has given classification of endodonticperiodontal lesion as [2,5,22,23]
(i) Primary endodontic lesions,
(ii) Primary endodontic lesions with secondary periodontal involvement,
(iii) Primary periodontal lesions,
(iv) Primary periodontal lesions with secondary endodontic involvement,
(v) True combined lesions.
In 1999, the world workshop for classification of periodontal diseases gave classification of periodontitis associated with endodontic disease as
(i) Endodontic-periodontal lesion,
(ii) Periodontal-endodontic lesion,
(iii) Combined lesion.
Pathways of communications
Three main pathways which were considered as prime route for endodontic-periodontal lesions are [3-5,22,24],
Apical foramen.
Dentinal tubules.
Lateral and accessory canals.
Etiopathogenesis of endo-perio lesions
✓ Live pathogens-bacteria, fungi, viruses.
✓ Nonliving etiological agents -foreign bodies, cholesterol crystals, Russell bodies, Rushton hyaline bodies.
Contributing factors [3,24,25]
✓ Poor endodontic treatment.
✓ Coronal leakage.
✓ Root resorption.
✓ Perforations.
✓ Trauma.
✓ Developmental malformations [26].
✓ Cracked tooth syndrome.
Characteristics of diseases
The characteristics of diseases are mentioned in Table 1 [3,5,24,25].
| Pathogenesis | Clinical Features | Treatment | Prognosis | |
|---|---|---|---|---|
| Primary Endodontic Lesion | It arises as a sequel of pulpitis from dental caries, wear defects, trauma and fracture. A primary endodontic lesion presents a necrotic pulp and a chronic periapical abscess with a sinus tract draining through periodontal ligament space or gingival sulcus. | The lesion presents an ‘isolated’ periodontal problem in relation to the affected tooth only, without a generalized periodontal disease. H/O pulpitis. A sinus tract, originating from apex, is present in sulcus. Negative pulp vitality test. | Endodontic therapy must be performed in multiple appointment, to reevaluate healing process between the beginning and completion of treatment. Periodontal therapy isn’t required usually. | They exhibit good prognosis. Radiographic and clinical healing occurs rapidly. A sinus tract heals soon after canal debridement -within 3-6 months. |
| Primary Periodontal Lesion | The lesion develops as sequelae of progressing periodontal problem extending to the apex. Plaque represents the prime etiologic factor. | Patients present with generalized chronic periodontitis. Minimal or no pain. Positive pulp vitality test. | Surgical/ non-surgical periodontal therapy. Re-evaluation must be done periodically to check for retro-infection of pulp | The prognosis is entirely dependent on periodontal therapy and hence, extent of periodontal damage. |
| Primary Endodontic Lesion with Secondary Periodontal Involvement | It arises when periodontal problem develops on teeth with PEL. Plaque and calculus is often deposited in draining sinus tract; creating a secondary periodontal problem | Negative pulp vitality test. Presence of plaque and calculus, in the way of sinus tract. | Endodontic therapy. Periodontal therapy – should not be employed until complete debridement of canal is achieved | Prognosis of endodontic therapy is predictable. Regeneration of periodontal tissue depends upon the extent of tissue destruction |
| Primary Periodontal Lesion with Secondary Endodontic Involvement | It arises as retro-infection of pulp, when periodontal lesion extends to apex. It may also follow the path through a lateral canal. | Negative/ altered pulp vitality test (as pulp can be necrotic/ partially vital, especially in multi-rooted teeth) | Surgical/ non-surgical periodontal therapyEndodontic therapy | The prognosis depends upon periodontal therapy and hence, extent of periodontal damage. |
| True Combined Lesion | Here pulpal and periodontal lesions develop and unite independently. | Features are similar to primary periodontal lesions. In addition, there must be some caries, trauma, fracture, wear defects, deep restoration or history of endodontic therapy. Negative pulp vitality test. | Endodontic therapy and periodontal therapy. Root resection can be in need with regenerative therapy. | Prognosis of lesion is related to extent of periodontal damage. |
Table 1: Characteristics of diseases.
Table 2 describes the diagnostic features of endo perio lesion.
| Clinical | Pulpal | Periodontal |
|---|---|---|
| Vitality | Non vital | Vital |
| Restorative | Deep or extensive | Not related |
| Plaque/calculus | Not related | Primary cause |
| Inflammation | acute | chronic |
| Pockets | Single, narrow | Multiple, wide coronally |
| pH value | Often acid | Usually alkaline |
| Trauma | Primary or secondary | Contributing factor |
| Microbial | few | complex |
| Radiographic | ||
| Pattern | localized | generalised |
| Bone Loss | Wider apically | Wider coronally |
| Periapical | radiolucent | Not often related |
| Vertical bone loss | no | yes |
| Histopathological | ||
| Junctional epithelium | No apical migration | Apical migration |
| Granulation tissue | apical | coronal |
| Gingival | normal | recession |
| Treatment | Root canal therapy | Periodontal treatment |
Table 2: Diagnosis.
Table 3 describes the findings of endo perio lesion [3,24]
| Examination/ tests |
Primary Endodontic lesion |
Primary periodontal lesion |
Primary endodontic secondary periodontal |
Primary periodontal secondary endodontic |
True combined lesion or concomitant lesions |
|---|---|---|---|---|---|
| Visual | Presence of sinus opening. Presence of decay/large restoration, fractured restoration or tooth/erosions/ abrasions/cracks/ discolorations/ poor RCT |
Inflamed gingiva/gingival recession, Accumulation of plaque and subgingival calculus around multiple teeth. Intact teeth Presence of periodontal abscess |
Plaque forms at the gingival margin of the sinus tract and leads to inflammation of marginal gingiva exudate Root perforation /fracture/ displaced post |
Presence of plaque, subgingival calculus and swelling around multiple teeth Presence of pus, Exudate. Presence of localized/ generalized gingival recession and exposure of root |
Plaque, calculus and periodontitis will be present in varying degrees. Swelling around single or multiple teeth Presence of pus, exudate |
| Pain | Sharp | Usually dull ache Sharp only in acute condition |
Usually sharp shooting. Dull ache in chronic conditions |
Usually sharp shooting. Dull ache in chronic conditions |
Dull ache usually Only in acute conditions it is severe |
| Palpation | It does not indicate the origin | Pain on palpation | Pain on palpation | Pain on palpation | Pain on palpation |
| Percussion | Tender on percussion | Tender on percussion | Tender on percussion | Tender on percussion | Tender on percussion |
| Mobility | Fractured roots and recently traumatized teeth often present high mobility |
Localized to generalized mobility of teeth |
Localized mobility | Generalized mobility | Generalized mobility with higher grade of mobility related to the involved tooth |
| Pulp vitality using cold test, electric pulp test | A lingering response‐irreversible pulpitis. No response in necrotic pulp |
The pulp is vital and responsive to testing | Pulp vitality tests negative |
Pulp vitality may be positive in multirooted teeth |
Usually negative. Positive response in multirooted teeth |
| Pocket probing | None unless sinus tract | Moderate | Evident or sinus tract | Severe | Severe, connects with periapex |
| Sinus tracing | A radiograph with gutta percha points to apex or furcation area in molars |
Sinus tract mainly at the lateral aspect of the root |
Sinus tract mainly at the apex or furcation area | Sinus tract mainly at the lateral aspect of the root | Difficult to trace out the origin of the lesion |
| Radiographs | Possible periapical radiolucency | Decreased crestal bone height | Radiolucency from apex to sulcus,decreased crestal bone height |
Bone loss approaching apex | Bone loss extending to apex |
| Cracked tooth | Painful response to chewing | No symptoms | Painful response to chewing | No symptoms | Painful response to chewing |
Table 3: Findings of endo perio lesion.
Figure 1 shows the decision analysis for diagnosis of endodontic-periodontal lesion.
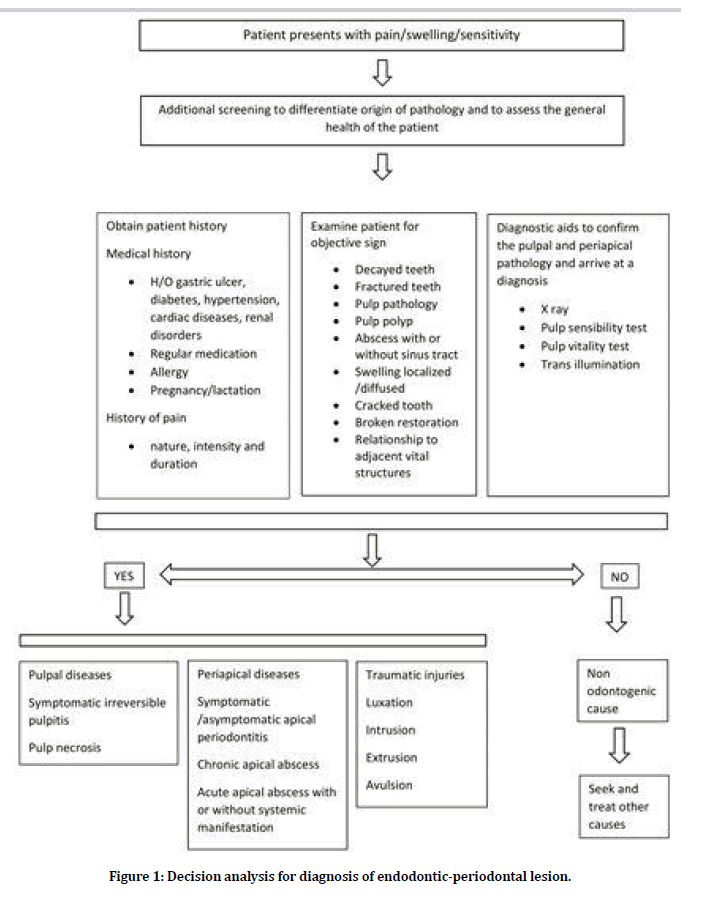
Figure 1. Decision analysis for diagnosis of endodontic-periodontal lesion.
Figure 2 Shows decision analysis for diagnosis of endodontic-periodontal lesion [22].
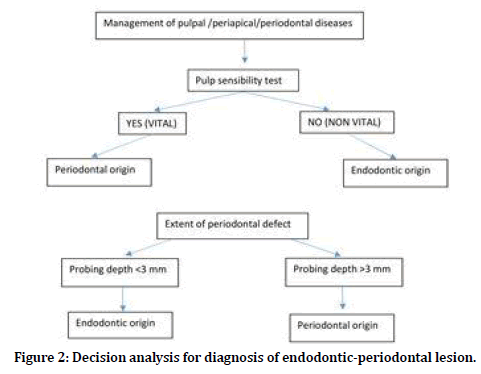
Figure 2. Decision analysis for diagnosis of endodontic-periodontal lesion.
Decision analysis for the treatment of endodontic and periodontal lesion (Figure 3) [24,28-31].
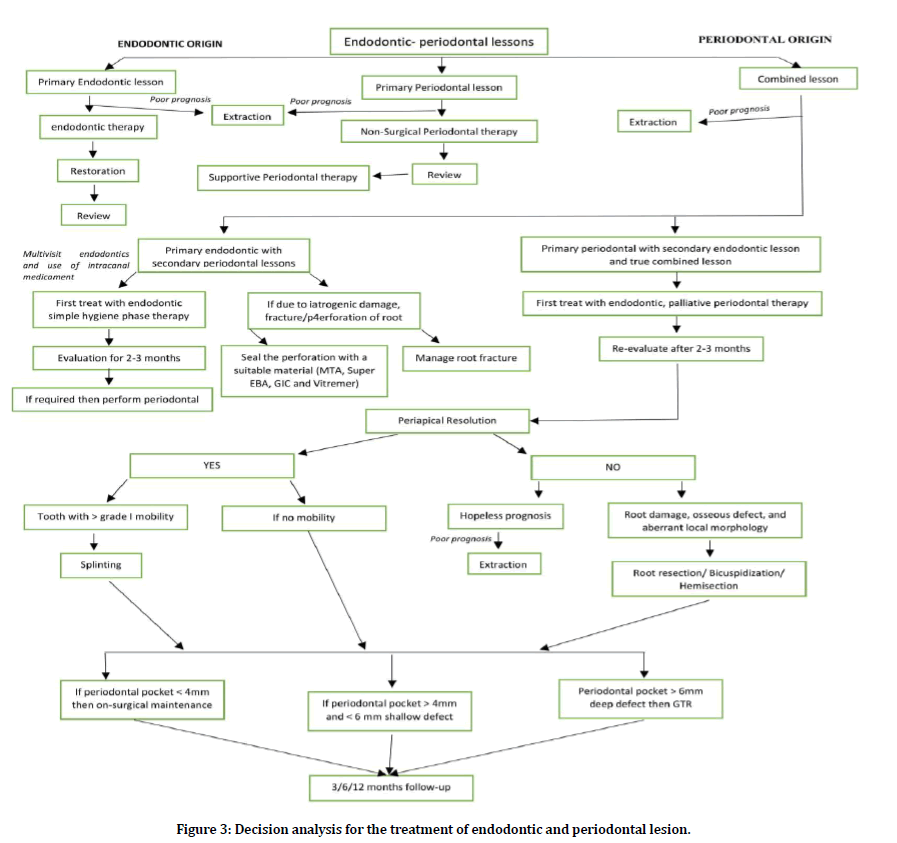
Figure 3. Decision analysis for the treatment of endodontic and periodontal lesion.
Acknowledgement
The authors would like to acknowledge all the faculties of the Department of Conservative Dentistry and Endodontics for their constant encouragement with my work during all stages.
Conflict of Interest
There is no conflict of interest.
References
- Al-Fouzan KS. A new classification of endodontic-periodontal lesions. Int J Dent 2014; 2014.
- Simon JH, Glick DH, Frank AL. The relationship of endodontic–periodontic lesions. J Endodont 2013; 39:41-46.
- Raja Sunitha V, Emmadi P, Namasivayam A, et al. The periodontal–endodontic continuum: A review. J Conservative Dent 2008; 11:54.
- Zehnder M, Gold SI, Hasselgren G. Pathologic interactions in pulpal and periodontal tissues. J Clin Periodontol 2002; 29:663-671.
- Shenoy N, Shenoy A. Endo-perio lesions: Diagnosis and clinical considerations. Indian J Dent Res 2010; 21:579.
- Govindaraju L, Neelakantan P, Gutmann JL. Effect of root canal irrigating solutions on the compressive strength of tricalcium silicate cements. Clin Oral Investigations 2017; 21:567-571.
- Azeem RA, Sureshbabu NM. Clinical performance of direct versus indirect composite restorations in posterior teeth: A systematic review. J Conservative Dent 2018; 21:2.
- Jenarthanan S, Subbarao C. Comparative evaluation of the efficacy of diclofenac sodium administered using different delivery routes in the management of endodontic pain: A randomized controlled clinical trial. J Conservative Dent 2018; 21:297.
- Manohar MP, Sharma S. A survey of the knowledge, attitude, and awareness about the principal choice of intracanal medicaments among the general dental practitioners and nonendodontic specialists. Indian J Dent Res 2018; 29:716-720.
- Mahalakshmi Nandakumar IN. Comparative evaluation of grape seed and cranberry extracts in preventing enamel erosion: An optical emission spectrometric analysis. J Conservative Dent 2018; 21:516.
- Teja KV, Ramesh S, Priya V. Regulation of matrix metalloproteinase-3 gene expression in inflammation: A molecular study. J Conservative Dent 2018; 21:592.
- Janani K, Sandhya R. A survey on skills for cone beam computed tomography interpretation among endodontists for endodontic treatment procedure. Indian J Dent Res 2019; 30:834-838.
- Khandelwal A, Palanivelu A. Correlation between dental caries and salivary albumin in adult population in Chennai: An in vivo study. Br Dent Sci 2019; 22:228-233.
- Malli Sureshbabu N, Selvarasu K, Nandakumar M, et al. Concentrated growth factors as an ingenious biomaterial in regeneration of bony defects after periapical surgery: A report of two cases. Case Reports Dent 2019; 2019.
- Poorni S, Srinivasan MR, Nivedhitha MS. Probiotic Streptococcus strains in caries prevention: A systematic review. J Conservative Dent 2019; 22:123.
- Rajakeerthi R, Nivedhitha MS. Natural product as the storage medium for an avulsed tooth–A systematic review. Cumhuriyet Dent J 2019; 22:249-256.
- Rajendran R, Kunjusankaran RN, Sandhya R, et al. Comparative evaluation of remineralizing potential of a paste containing bioactive glass and a topical cream containing casein phosphopeptide-amorphous calcium phosphate: An in vitro study. Pesquisa Br Odont Clin Integr 2019; 19.
- Ramarao S, Sathyanarayanan U. CRA Grid-A preliminary development and calibration of a paper-based objectivization of caries risk assessment in undergraduate dental education. J Conservative Dent 2019; 22:185.
- Siddique R, Nivedhitha MS. Effectiveness of rotary and reciprocating systems on microbial reduction: A systematic review. J Conservative Dent 2019; 22:114.
- Siddique R, Sureshbabu NM, Somasundaram J, et al. Qualitative and quantitative analysis of precipitate formation following interaction of chlorhexidine with sodium hypochlorite, neem, and tulsi. J Conservative Dent 2019; 22:40-47.
- Siddique R, Nivedhitha MS, Jacob B. Quantitative analysis for detection of toxic elements in various irrigants, their combination (precipitate), and para-chloroaniline: An inductively coupled plasma mass spectrometry study. J Conservative Dent 2019; 22:344.
- Rotstein I, Simon JH. Diagnosis, prognosis and decision‐making in the treatment of combined periodontal‐endodontic lesions. Periodontology 2004; 34:165-203.
- Goiriz B, Diaz E, Estevez R, et al. Management in the diagnosis and treatment of Endo-Perio lesions. J Clin Exp Dent 2017; S15–15.
- Parolia A, Gait TC, Porto IC, et al. Endo-perio lesion: A dilemma from 19 th until 21 st century. J Interdisciplinary Dent 2013; 3:2.
- Parolia A, Gait TC, Porto IC, et al. Endo-perio lesion: A dilemma from 19 th until 21 st century. J Interdisciplinary Dent 2013; 3:2.
- Satpathy A, Mohanty G, Datta P, et al. Palatogingival groove and the perio-endo lesion: Management through endo--perio regenerative (IPRF) approach: A case report. Indian J Public Health Res Develop 2019; 10.
- Berman LH, Hargreaves KM, Cohen SR. Cohen’s pathways of the pulp expert consult-E-Book. Elsevier Health Sciences 2010.
- Kuka Gİ, Barut G, Gürsoy H. Classification and current treatment options of endo-perio lesions. Yeditepe Dent J 2017; 45–48.
- Schmidt JC, Walter C, Amato M, et al. Treatment of periodontal‐endodontic lesions–a systematic review. J Clin Periodont 2014; 41:779-790.
- Vishwanath V, Rao HM, Prasad BK, et al. Successful endodontic management of endo-perio lesions with different treatment modalities: Case series. J Res Dent Sci 2019; 10:105.
- Solomon C, Chalfin H, Kellert M, et al. The endodontic-periodontal lesion: a rational approach to treatment. J Am Dent Assoc 1995; 126:473-479.
Author Info
Keerthika R and Nivedhitha MS*
Department of Conservative dentistry and Endodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical And Technical Sciences, Saveetha University Tamilnadu, Chennai, IndiaCitation: Keerthika R, Nivedhitha MS, Endodontic Periodontal Lesion Diagnosis and Treatment Decision Analysis, J Res Med Dent Sci, 2021, 9 (2): 140-145.
Received: 23-Sep-2020 Accepted: 02-Feb-2021
