Research - (2022) Volume 10, Issue 12
EFFICIENCY OF LOW-LEVEL LASER THERAPY ON IMPLANTS RETAINED MANDIBULAR OVERLAY
*Correspondence: Lamya M Saeed, College of Dentistry, National University of Science and Technology, Iraq, Email:
Abstract
Background/Aim: Many difficulties are encountered in providing a successful complete denture treatment. Among these problems are the ways to provide comfort, function, proper esthetics, and retention for complete dentures in patients with missing natural dentitions. The aim of this study deals with the successful rehabilitation of edentulous mandibular ridge (split-mouth technique), retained with dental implants in the canine regions, using a flapless surgical technique, with an exposure of Low-Level Laser Therapy (LLLT) after implant installment to evaluate its influence on the osseointegration, implant stability was evaluated using periotest at time of loading, 3 months and 6 months later to show the early success of dental implants placed into low- density bone. Also, bone changes were evaluated by using digital periapical radiography with paralleling technique. Materials and methods: Following the split-mouth design, two implants were inserted in the mandible of 10 patients, the right side dental implants received LLLT ( laser side) with an output power of 0.5 UT and the continuous mode was used to receive a total dose of 30 J per implant over 60 seconds, while the other side was the control side. The soft laser treatment was performed immediately after the surgery, 3 days and a week after surgery, then evaluated for stability during the follow-up period (at time of loading, 3 months, and 6 months later) using periotest, and further bone height changes using digital radiograph. Results: Irradiated implants achieved higher stability compared with the control group during the entire follow-up period. At baseline and after 3 months, there was no statistically significant difference between implant stability quotient (ISQ) values on the two sides. After 6 months; the laser side showed statistically significantly higher mean ISQ values than the control side. Conclusion: Current study demonstrated that 6 months after soft laser application significantly progressively influenced implant stability and bone height around dental implants.
Keywords
Soft laser in dentistry, Dental implants, Mandibular over denture
Introduction
Treatment of the edentulous mandible has always been one of the most challenging matters in dentistry [1-5]. A traditional full denture is the most common treatment modality for these cases. The introduction of Osseo integrated implants has infinitely improved treatment consequences in patients with complete edentulism. Increased stability and retention of prostheses can be achieved by one of two means, either an implant-retained removable over denture or an implant-supported fixed prosthesis [6-11].
Implant-retained dental restorations have been verified to be a workable solution for the rehabilitation of edentulous patients. The outcome of implantsupported over denture treatment achieved a better prognosis than of conventional complete dentures, where stability, retention, ease of chewing, and comfort are remarkably improved [12]. Adding to this, greater occlusal awareness, allows for reducing the prosthetic flanges and palatal coverage, which are a great benefit for new denture wearers and gaggers, and thus tend to improve the facial esthetics [13]. Implants-supported overdentures are classified according to the type of support into either total implant-supported over denture or implant mucosa-supported overdenture [14].
Using computer-guided surgical stents made the diagnosis possible using 3D imaging and transferring the exact plan to the surgical area. They are manufactured to transfer the angulation, depth, and localization of the implants to the preparation area [15,16], however, using the flapless technique surgery could be achieved as it considers to be a minimally invasive surgical approach. The advantages of this technique are described as reducing operation time, postoperative complications e.g., pain and swelling, also patient comfort showing an increase after the operation. Disadvantages of this technique are also should be considered as a lack of visibility of anatomical features and critical structures e.g., blood vessels and nerves, in addition, uncontrolled removal of keratinized gingiva due to the use of mucotome was notified as a complication of the flapless implant approach [17,18].
Low-level laser therapy (LLLT) has been used for more than 30 years in the medical field and no adverse effects have been reported [19]. It is defined as a red beam or near-infrared laser therapy of low energy density and output power, with wavelengths between 500 and 1,200 nm, that do not increase normal tissue and body temperature. LLLT found to be effective as it stimulates fracture site vascularization and bone defect and stimulates osteoblasts which in turn can facilitate the recovery of hard tissues. Recently, it was reported that LLLT has a positive effect on ossification and Osseointegration of dental implants [20-22]. Research has been focused on the potential of LLLT in oral implantology to reduce the healing time following implant placement and improve the potential for bone regeneration. There are several studies suggesting that low-level laser treatment in the early postoperative period after implant placement may lead to a positive clinical effect [23]. Postoperative LLLT might have a potential beneficial influence on dental implant treatment in this area, making it more predictable [24,25].
Materials and Methods
10 individuals with mandibular completely edentulous ridge were selected from Outpatient Clinic, Prosthodontics Department, Faculty of oral and dental Medicine, Cairo University, according to the following criteria: All patients were apparently in good general health, they had angle’s class I maxilla-mandibular relationship. All patients were physically and psychologically able to tolerate conventional surgical protocol. All selected patients were non-smoking. Their ages ranged from 40-60 years. All patients had completely edentulous mandibular ridges (Figure 1) as opposed to maxillary dentition (natural mandibular teeth or restored with fixed and/or removable restoration). They had adequate inter-arch distance. All patients had sufficient bone height and width confirmed radiographically preoperatively. Patients with the following criteria were excluded from this study: Presence of acute and active infection or inflammation in areas intended for implant placement.
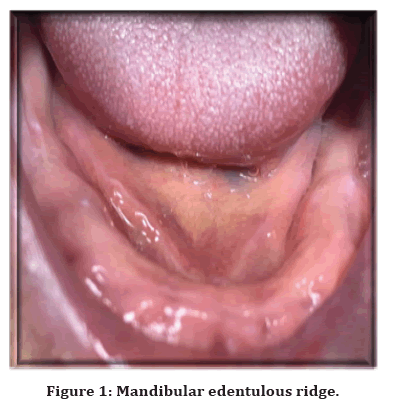
Figure 1. Mandibular edentulous ridge.
Patients with apparently T.M.J. troubles or Parafunctional habits such as bruxism, and clenching were excluded. And also the Presence of pathological findings in oral soft tissue diseases. Patients with poor oral hygiene. Only cooperative patients were included in the study to ensure their commitment to oral hygiene measures and regular follow-up visits.
Intraoral examinations included visual and digital assessment was done, also Digital examination was done, as well as mucosa overlying the area of prospective implants was examined. Radiographic examinations where Pre-operative cone-beam computed tomography (CBCT) was made to evaluate and plan the vertical bone height and Bucco-palatal dimension available for implant installation.
Following the Split-mouth technique, two implants of 4mm in diameter and 12mm in length were placed in the lower edentulous ridge (canine region), Patients will receive implants-supported mandibular overdenture retained with locator attachments using a computerguided surgical stent for the surgical procedure (flapless technique).
Prosthetic rehabilitation steps
Preliminary maxillary and mandibular impressions were made using alginate impression material (Cavex Holland B.V., P.O. Box 852-2006 RW Harlem, Holland) in a suitable stock tray and poured to obtain the diagnostic casts upon which self-cured acrylic resin (Peka Tray Acrostone, England) special tray was constructed.
The final maxillary impression was made using rubber base impression material (Gollene Speedex Dental Vertriebs Gmnbtt Konstan, Germany), boxed, and poured into dental stone.
Occlusion block is then constructed on the obtained master cast. Maxillary face bow record (Gnatus face bow Brazil), Was made to mount the upper cast on a semiadjustable articulator (Whip Mix # 8500 semi-adjustable articulator, Louisville, KY. U.S.A). the mandibular cast was mounted according to a centric relation record obtained from the patient using check bite technique, and finally, a protrusive record was essential to adjust the horizontal condylar guidance of the articulator.
Acrylic resin teeth (Vertex quint teeth. Vertexdental, Netherland) of appropriate shape and shade were arranged following the lingualized occlusion concept and then tried in the patient’s mouth. Processing the denture using heat-cured acrylic resin. The denture was finished and polished then inserted and checked intraorally for extension, stability, retention, vertical dimension, centric relation, and esthetics. Any necessary occlusal adjustment was performed to achieve harmonious occlusion (Figure 2).
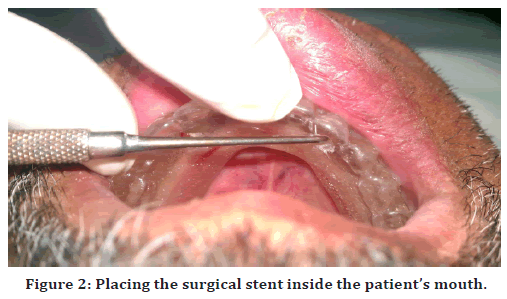
Figure 2. Placing the surgical stent inside the patient’s mouth.
A CT image was produced for the lower jaw using a cone beam CT machine (CBCT). While wearing the radiographic stent, the resultant image was obtained in a Dicom format file on a compact disc.
Computer-guided surgical stent construction was done using the Dicom files from the CT scan loaded into the mimics 10.01 software (Materialize Incorporation, Belgium) to perform implant planning. The raw stent produced by the 3D printing machine and metallic sleeves were fitted into the designed holes of the fabricated stent.
A pre-surgical medication was instructed to be under the umbrella of antibiotics to control the infection. Amoxicillin clavulanate 625mg (Amoxicillin clavulanate, Galaxo-Smith Kline, Beecham, Great Britain) was taken24 hours before surgery as one tablet every 8 hours. Patients were asked to continue the antibiotic for one week after surgery to guard against any possible infection. They were also given an anti-inflammatory and an analgesic drug. After checking the retention and stability of the stent, infiltration anesthesia was given. The surgical stent was chemically disinfected by Cidex (Cidex Activated Dialdehyde Solution. J and J Medica). Stabilize the stent in place using three fixation screws (one anteriorly and two posteriorly on both sides).
Osteotomy was performed using the classical drilling sequence (pilot, intermediate and final drill). A specially designed “drill guide” was used for every surgical drill. They are cylinders with a short handle the outer diameter of the drill guide fits accurately within the stent’s metal sleeves, the inner diameter of the drill guide was 2.5,3, and 3.5 for the 2.3, 2.8, and 3.4 drills respectively to prevent friction between the sleeve and the stent and also to allow the irrigation to penetrate with the up and down motion of the drill. The drilling procedure was started with a pilot drill 2.3 in diameter to the predetermined depth (10mm or 12mm) followed by two successive drills, an intermediate 2.8mm and a final drill of 3.4mm in diameter. The implant (PITT-EASY, Screw-Vent Tapered, Germany) was inserted manually through the stent till manual tightening met resistance (Figure 3).
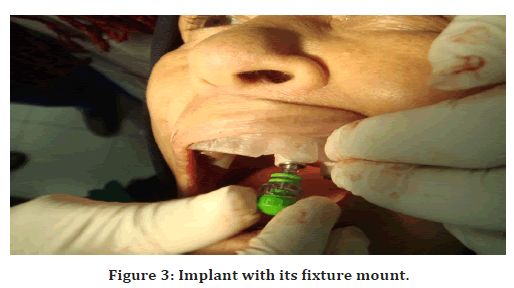
Figure 3. Implant with its fixture mount.
The fixture mount was removed, and threading was then continued using a ratchet until the implant top flashed completely with the bone. The fixture mount was then unscrewed using the 1.25mm screw driver. The same procedure was repeated for all implants. Finally, the fixation screws were unscrewed and the stent was removed, and the covering screws were threaded to the implants.
Patients were instructed to continue the pre-surgical medication in addition to the anti-edematous drug starting the day of surgery 3 times per day and continued for one week and follow oral hygiene measures. The analgesics for 5 days rinse with a mouthwash starting the day after the surgical operation and continue for 10 days, and to eat only soft food for one month.
A post-operative digital panoramic x-ray was taken to insure the actual sites and the parallelism between the installed implants. Low-Level Laser Therapy (LLLT) For only two implants on the right side of the arch was applied as follows; a Diode laser device (Dio Dent Micro 980, USA), with an output power of 0.5 ut, and the continuous mode was used to receive a total dose of 30 J per implant over 60 seconds (Figure 4).

Figure 4. Dio Dent Micro 980 laser device.
The dose was divided into two applications, one toward the apex of the implant and the other at the crest (mesiodistally and Bucco-palatally). Wearing protective eye goggles by both the patients and the operator as laser safety measures was mandatory. The handpiece of the device was positioned perpendicular to the long axis of each implant and 2-3mm away from the mucosa (Figure 5). Each patient received three sessions of LLLT, after implant insertion, 3 days, and a week after surgery.
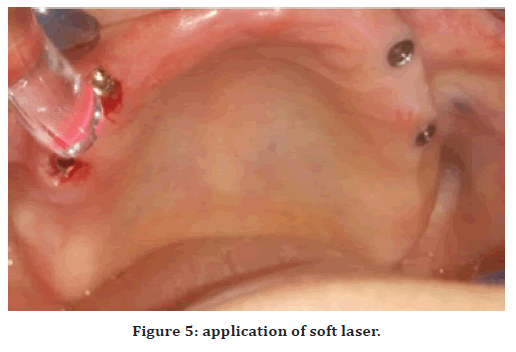
Figure 5. application of soft laser.
Second stage surgery
Three months following surgical implant installation, patients were recalled for the second stage of surgery and prosthetic phase, and the implants were relocated using the surgical template, implants cover screws were exposed by short, crested incisions under local anesthesia guided by the surgical stent. The cover screws were loosened using the hex driver followed by healing abutments which were installed for two weeks (Two weeks later the healing abutments were replaced with the appropriate extension abutments).
For using locator attachments, a direct pick-up procedure was done, Relief holes corresponding to each Locator were made on denture bases using a #8 round bur to make sufficient room for the male part of the Locator attachments through the application of a white marker over the metal housing.
The denture should be assured for proper seating as proved by the absence of rocking and proper occlusion. The self-cure acrylic resin was mixed according to the manufacturer’s instruction and applied in the relieved areas of the denture then seated inside the patient’s mouth, the patients were asked to bite in centric occlusion with minimal pressure. After polymerization of the resin, the denture is removed, trimmed, and polished with the metal housings picked up in its fitting surface. The plastic sleeves were removed using different parts of the locator tool, the black processing caps were removed using the male removal tool (front part) of the locator core tool. The pink retentive cap was held using the male seating tool (middle part) of the locator core tool and firmly pushed into the metal housing, a click sound was confirming the full seating of the male part.
Implant stability evaluation Implant mobility was evaluated using periotest (Periotest M, Medizintechnik Gulden e.k. Eschenweg, Germany) at the time of loading, 2 months, and 4months later. Patients were instructed to sit in an upright position and the tapping head was used to perform percussion on the implant; the mean value was calculated from three same consecutive measures obtained from the periotest.
Follow-up All patients were evaluated radiographically at the time of loading, three months, and six months thereafter. Radiographic evaluation Standardized periapical radiographs were achieved using digital periapical radiography with paralleling technique utilizing a specially innovated radiographic guide for this purpose. Radiographs were recorded all with the same radiographic machine and exposure parameters. The radiographs were compared regarding the marginal bone height.
Results
Implant stability quotient (ISQ) results
Comparison between ISQ values at the buccal, palatal, mesial, and distal directions within each side
Laser side
There was no statistically significant difference between ISQ values at the buccal, palatal, mesial, and distal directions through all periods.
Control side
There was no statistically significant difference between ISO values at the buccal, palatal, mesial, and distal directions through all periods. The mean of the four directions was used for further comparisons because there was no statistically significant difference between the four directions on each side (Table 1).
| Side | Direction Period | B | P | M | D | P-value | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| mean | SD | mean | SD | mean | SD | mean | SD | |||
| Laser | Baseline | 64 | 2.4 | 63 | 3.3 | 63 | 4.1 | 62 | 6.3 | 0.475 |
| 3 months | 68 | 4.5 | 68.2 | 3.5 | 67 | 5.5 | 67.4 | 4.9 | 0.664 | |
| 6 months | 71.8 | 3.7 | 70.8 | 5.1 | 71 | 4.9 | 71.4 | 3.9 | 0.785 | |
| Control | Baseline | 63.6 | 4.5 | 62.8 | 7.1 | 63.2 | 6 | 64 | 5.9 | 0.651 |
| 3 months | 66.4 | 3.7 | 66 | 6 | 65.8 | 4.5 | 65.6 | 4.8 | 0.793 | |
| 6 months | 69.2 | 5.1 | 68.8 | 4.6 | 68.8 | 4.5 | 68.8 | 5.2 | 0.8 | |
| *: Significant at P≤ 0.05 | ||||||||||
Table 1: The mean, standard deviation (SD) values, and results of repeated measures ANOVA test for comparison between ISQ values at the B, P, M, and D directions within each side.
Comparison between ISQ values on the two sides
At baseline, after 3 months; there was no statistically significant difference between ISQ values on the two sides. After 6 months; the laser side showed statistically significantly higher mean ISQ values than the control side (Table 2).
| Side period | laser | Control | P-value | ||
|---|---|---|---|---|---|
| mean | SD | mean | SD | ||
| Baseline | 63 | 4.7 | 63.4 | 3.8 | 0.784 |
| 3 months | 67.7 | 4.3 | 65.9 | 5.1 | 0.519 |
| 6 months | 75.5 | 4.6 | 71.9 | 5.2 | 0.040* |
Table 2: The mean, standard deviation (SD) values, and results of paired t-test for comparison between ISQ values on the two sides.
Change by time within each side
Laser side
There was a statistically significant increase in mean ISQ value after 3 and 6 months.
Control side
There was a non-statistically increase in mean ISQ value after 3 months but there was a statistically significant increase in mean ISQ value after 6 months (Tables 3 and 4).
| Period | Mean difference | SD | P-value |
|---|---|---|---|
| Baseline-3months | 4.7 | 1.4 | 0.010* |
| Baseline-6months | 8.3 | 2.3 | <0.001* |
Table 3: The mean, standard deviation (SD) values, and results of paired t-test for changes by time in mean ISQ values of laser side.
| Period | Mean difference | SD | P-value |
|---|---|---|---|
| Baseline-3months | 2.5 | 1.1 | 0.061 |
| Baseline-6months | 5.5 | 2.4 | <0.008* |
Table 4: The mean, standard deviation (SD) values, and results of paired t-test for changes by time in mean ISQ values of the control side.
Bone loss
Comparison between bone losses in the two sides
There was a statistically significant difference between bone losses on the two sides through all periods (Table 5).
| Side period | Laser | Control | P-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Baseline-4months | 0.2 | 0.1 | 0.3 | 0.2 | 0.827 |
| Baseline-6months | 0.3 | 0.1 | 0.5 | 0.2 | 0.732 |
Table 5: The mean, standard deviation (SD) values, and results of the Wilcoxon signed-rank test for comparison between bone losses on the two sides.
Discussion
For implants installation, using the flapless technique provides a reduced amount of tissue trauma and allows for a greater chance to preserve alveolar bone levels by not disturbing the periosteum layer and by improving blood supply to the implant site, these benefits were suggested to overcome the delayed mucosal wound healing side, also it was reported that this technique tends to be more difficult due to the inability of the surgeon to visualize anatomical landmarks and vital structures directly [26-28].
Clinical results showed that low laser level therapy (LLLT) has a positive effect on inflamed areas as well as on wound healing and neo angiogenesis by stimulating the production of endothelial cells and also on the integration of implants [29].
Implant stability measurements using periotest were evaluated and the results were concluded as a favorable effect of LLLT on healing and attachment of bone to titanium dental implants. The implants lased showed overall higher periotest measurements of “ISQ” values of implant stability thus LLLT has got the potential of beneficial effects on the initial establishment of the implant-bone interface.
These results suggest that LLLT could broaden and strengthen attachment to titanium dental implants, accelerate soft tissue-implant interactions, and reduce healing time which agrees with other results [29-31] that indicates that this therapy enhances the initial attachment and proliferation of HGF. Therefore, LLLT has a beneficial effect on the establishment of the implant-soft tissue interface. By the end of the follow-up period, a significant decrease of the crestal bone for the unused side was noticed to be about 0.3 mm-0.5mm which were accepted for implant success [32-34].
The alveolar bone height on the lased side (right side of all patients) was preserved, while the unused side showed a decrease in bone height. Therefore, these findings could be related to the laser application since both sides are in the same patient and have been subjected to equal functional factors and equal distribution of loading forces.
Conclusion
Based on the results of this study, the following can be concluded, the present investigation demonstrated that 6 months of soft laser application significantly positively influenced implant stability and bone height around dental implants. Further studies of the exact mechanism of soft laser on bone metabolism should be held out on larger sample sizes with further histopathological and morphometric studies in animals.
References
- Zembic A, Kim S, Zwahlen M, et al. Systematic review of the survival rate and incidence of biologic, technical, and esthetic complications of single implant abutments supporting fixed prostheses. Int J Oral Maxillofac Implant 2014; 29.
- Paleari AG, Presoto CD, Vasconcelos JA, et al. An alternative technique for fabrication of frameworks in an immediate loading implant fixed mandibular prosthesis. Case Rep Dent 2015; 2015.
- Nokar S, Naini RB. The effect of superstructure design on stress distribution in peri-implant bone during mandibular flexure. Int J Oral Maxillofac Implant 2010; 25.
- Attard NJ, Zarb GA. Immediate and early implant loading protocols: A literature review of clinical studies. J Prosthet Dent 2005; 94:242-258.
- Becker W. Immediate implant placement: Treatment planning and surgical steps for successful outcomes. Br Dent J 2006; 201:199-205.
- Bernardes SR, de Araújo CA, Neto AJ, et al. Photoelastic analysis of stress patterns from different implant-abutment interfaces. Int J Oral Maxillofac Implant 2009; 24.
- Blanes RJ. To what extent does the crown–implant ratio affect the survival and complications of implant-supported reconstructions? A systematic review. Clin Oral Implant Res 2009; 20:67-72.
- Law C, Bennani V, Lyons K, et al. Influence of implant framework and mandibular flexure on the strain distribution on a Kennedy class II mandible restored with a long-span implant fixed restoration: A pilot study. J Prosthet Dent 2014; 112:31-37.
- Fischman B. The rotational aspect of mandibular flexure. J Prosthet Dent 1990; 64:483-485.
- Zarone F, Apicella A, Nicolais L, et al. Mandibular flexure and stress build-up in mandibular full-arch fixed prostheses supported by osseointegrated implants. Clin Oral Implant Res 2003; 14:103-114.
- Capelli M, Zuffetti F, Del Fabbro M, et al. Immediate rehabilitation of the completely edentulous jaw with fixed prostheses supported by either upright or tilted implants: A multicenter clinical study. Int J Oral Maxillofac Implant 2007; 22.
- Awad MA, Lund JP, Shapiro SH, et al. Oral health status and treatment satisfaction with mandibular implant overdentures and conventional dentures: a randomized clinical trial in a senior population. Int J Prosthod 2003; 16.
- Sadowsky SJ, Caputo AA. Effect of anchorage systems and extension base contact on load transfer with mandibular implant-retained overdentures. J Prosthet Dent 2000; 84:327-334.
- Arisan V, Karabuda ZC, Özdemir T. Accuracy of two stereolithographic guide systems for computer-aided implant placement: A computed tomography-based clinical comparative study. J Periodontol 2010; 81:43-51.
- Van Assche N, Van Steenberghe D, Quirynen M, et al. Accuracy assessment of computer-assisted flapless implant placement in partial edentulism. J Clin Periodontol 2010; 37:398-403.
- Ozan O, Turkyilmaz I, Ersoy AE, et al. Clinical accuracy of 3 different types of computed tomography-derived stereolithographic surgical guides in implant placement. J Oral Maxillofac Surg 2009; 67:394-401.
- D'haese J, Van De Velde T, Komiyama AI, et al. Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: A review of the literature. Clin Implant Dent Related Res 2012; 14:321-335.
- Sunitha RV, Sapthagiri E. Flapless implant surgery: A 2-year follow-up study of 40 implants. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116:e237-243.
- Harris DM. Editorial comment biomolecular mechanisms of laser biostimulation. J Clin Laser Med Surg 1991; 9:277-280.
- Khadra M, Rønold HJ, Lyngstadaas SP, et al. Low-level laser therapy stimulates bone–implant interaction: an experimental study in rabbits. Clin Oral Implant Res 2004; 15:325-332.
- Gomez N, Schmidt CE. Nerve growth factor-immobilized polypyrrole: Bioactive electrically conducting polymer for enhanced neurite extension. J Biomed Material Res 2007; 81:135-149.
- Jakse N, Payer M, Tangl S, et al. Influence of low-level laser treatment on bone regeneration and osseointegration of dental implants following sinus augmentation: An experimental study on sheep. Clin Oral Implant Res 2007; 18:517-524.
- Mandic B, Lazic Z, Markovic A, et al. Influence of postoperative low-level laser therapy on the osseointegration of self-tapping implants in the posterior maxilla: A 6-week split-mouth clinical study. Vojnosanitetski Pregled 2015; 72:233-240.
- Lekholm U. Patient selection and preparation. Tissue-integrated prosthesis: Osseointegration in clinical dentistry. 1985; 199-209.
- Bischof M, Nedir R, Szmukler-Moncler S, et al. Implant stability measurement of delayed and immediately loaded implants during healing. A clinical resonance-frequency analysis study with sandblasted-and-etched ITI implants. Clin Oral Implant Res 2004; 15:529-539.
- Scherer MD, Ingel AP, Rathi N. Flapped or flapless surgery for narrow-diameter implant placement for overdentures: Advantages, disadvantages, indications, and clinical rationale. Restorative Dent 2014; 34:s89-95.
- Cassetta M, Stefanelli LV, Giansanti M, et al. Depth deviation and occurrence of early surgical complications or unexpected events using a single stereolithographic surgi-guide. Int J Oral Maxillofac Surg 2011; 40:1377-1187.
- Lamster IB, Lalla E, Borgnakke WS, et al. The relationship between oral health and diabetes mellitus. J Am Dent Assoc 2008; 139:19S-24S.
- Petermann U. Die Wirkung der Laserakupunktur in der Wundheilung. Zeitschrift für Ganzheitliche Tiermedizin 2013; 27:50-57.
- Huang HH, Chuang YC, Chen ZH, et al. Improving the initial biocompatibility of a titanium surface using an Er, Cr: YSGG laser-powered hydrokinetic system. Dent Material 2007; 23:410-414.
- Chiapasco M, Abati S, Romeo E, et al. Implant-retained mandibular overdentures with Brånemark System MKII implants: A prospective comparative study between delayed and immediate loading. Int J Oral Maxillofac Implant 2001; 16.
- Cox JF, Zarb GA. The longitudinal clinical efficacy of osseointegrated dental implants: A 3-year report. Int J Oral Maxillofac Implant 1987; 2.
- Aoki A, Ando Y, Watanabe H, et al. In vitro studies on laser scaling of subgingival calculus with an erbium: YAG laser. J Periodontol 1994; 65:1097.
- Berglundh T, Abrahamsson I, Lang NP, et al. De novo alveolar bone formation adjacent to endosseous implants: a model study in the dog. Clin Oral Implant Res 2003; 14:251-262.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
College of Dentistry, National University of Science and Technology, Dhi Qar, IraqReceived: 20-Nov-2022, Manuscript No. jrmds-22-80499; , Pre QC No. jrmds-22-80499(PQ); Editor assigned: 22-Nov-2022, Pre QC No. jrmds-22-80499(PQ); Reviewed: 07-Dec-2022, QC No. jrmds-22-80499(Q); Revised: 12-Dec-2022, Manuscript No. jrmds-22-80499(R); Published: 19-Dec-2022
