Research - (2022) Volume 10, Issue 4
Efficacy of Varnishes with: Bioactive Glass, Recaldent Technology and Silver Diamine Fluoride in Comparison with Sodium Fluoride on Tooth Surface Micro-hardness (an In Vitro Study)
Marwa B Jasim* and Muna S Khalaf
*Correspondence: Marwa B Jasim, College of Dentistry, University of Mosul, Iraq, Email:
Abstract
Background: The reduction in the tooth surface micro-hardness denotes enamel surface destruction due to loss of the mineral content after exposing to demineralization process or carious lesion, which could be reversed by creating a suitable remineralization environment via using different remineralizing agents. Aim of the study: Study the efficacy of remineralizing agents (varnishes) with different techniques: Bioactive Glass (BAG), Recaldent technology: Casein Phosphopeptide Amorphous Calcium Phosphate (CPP-ACP), Silver Diamine Fluoride (SDF), and Sodium Fluoride 5% (NaF) on the enamel surface micro-hardness of the maxillary deciduous canine teeth. Materials and Methods: Fifty sound deciduous maxillary canine teeth were used as the experimental samples, and randomly distributed into 5 groups with 10 teeth for each group. The groups were: Group 1 (SDF), Group 2 (BAG), Group 3 (CPP-ACP), Group 4 (NaF), Group 5 Control kept in prepared artificial saliva without any treatment. All teeth samples of the whole groups were kept for 72 hours in specifically prepared demineralizing agent to produce artificial enamel carious lesion, then treated with remineralizing agent and measured after 2 weeks. Results: The results revealed that there was a significant decrease in the surface micro-hardness for the whole samples after demineralization. Comparing to the control (Group 5), there was a significant increase in the surface micro-hardness in the groups 1, 2, 3. Conclusion: According to the outcomes of the current study, groups (BAG, CPP-ACP, and SDF) were significantly higher in effect when compared with artificial saliva, except NaF group that showed better effect but not significant difference.Keywords
Micro-hardness, Remineralization, SDF, CPP-ACP, BAG
Introduction
In recent years, there has been a lot of modernization in treatment methods led to conversion of dental caries treatment from a surgical to a non-surgical approach [1]. Dental caries is a chronic infectious disease and not just a continuous progressive disease. It starts with the initial loss of minerals in the teeth and eventually leads to complete tooth destruction and loss by time. It occurs when there is an imbalance between the demineralization and remineralization process when the minerals are lost from the tooth surface [2]. By improving tooth mineralization, tooth decay can be arrested or treated early [3]. The demineralization process of the tooth enamel is recognized as dissolution and eventually the minerals of the hydroxyapatite crystals (HAP) are lost from the tooth structure because of the dropping of the oral environmental pH [4]. The remineralization process is considered as a natural mechanism of teeth repair that transfers minerals from the environment (such as saliva, biofilm) to the partially demineralized tooth structure, so that the minerals in the crystal lattice of (HAP) return to ionic form [5]. The imbalance between remineralization and demineralization processes is considered to be the extremely important factor in the treatment and/ or prevention of teeth decay [6]. Silver diamine fluoride (SDF) is cariostatic agent, effective, easy to use and inexpensive that has been suggested as a suitable additional treatment for dental caries in high-risk groups [7]. Bioactive glass (BAG) is a kind of bio ceramic material, which is composed of inorganic compound with multiple ingredients such as silicon, sodium, calcium, phosphorus and other elements. Amorphous calcium-sodium phosphosilicate is considered as its active ingredient. It is composed of minerals naturally present in body fluids. It reacts in contact with water and saliva releases calcium, phosphorus, sodium and silicon ions, leading to the formation of hydroxyapatite crystals (HAP), which deposit on the tooth surface and improving the remineralization of demineralized enamel surface [8]. Casein Phosphopeptide Amorphous Calcium Phosphate (CPP-ACP) consists of Casein Phosphopeptide (CPP) complex, which is a "milk protein" that can form nanoclusters, and Amorphous calcium phosphate (ACP). CPPACP can stabilize calcium ions and phosphate ions in the solution. Consequently Calcium ions and phosphate ions that can maintain its super saturation and deposit on the enamel surface of the tooth, increasing the content of Calcium ions to promote the remineralization of dental plaque, and it can also buffer the pH value of dental plaque [9]. The role of fluoride is known for a long time and has been recognized to be one of the most effective methods of prevention and control of the tooth decay, and it is also an effective way to remineralize the teeth [3]. Since the micro hardness of the surface mainly depends on the mineral content, particularly the inorganic content of tooth enamel, such as free calcium and phosphorus ions, the micro hardness of the tooth surface is an efficient indicator of the total impact of tooth mineralization [10].
Materials and Methods
Sample collection
Fifty maxillary primary canine teeth were collected and included in this study. Teeth extraction was done due to mobility, approaching the exfoliation time or for orthodontic causes. The inclusion criteria for teeth collection were lack of any caries, restorations, crack, fractures, white lesion, or any developmental anomalies [11]. The teeth were examined by magnifying lens with 10X to make sure of these criteria, then stored in 0.1% thymol solution [12].
Solutions preperation
1-Demineralizing solution: The demineralizing solution has been prepared to produce marked subsurface demineralization which analogous to enamel caries .
The following ingredients (50 mM acetic acid, 2.2 mMCa(NO3)2, 2.2 mM KH2PO4, 5.0 mM NaN3, 0.5 ppm NaF) have been mixed and incubated in shaker, at (37◦C, 50 rpm/min) for 72 hour and the pH was adjusted to 4.5, using portable pH meter to make sure of the specified pH of the prepared solution [13].
2-Artificial saliva: included several components with various concentrations which were: (10 gm. Sodium carboxymethyl cellulose, 1 gm Sodium chloride, 0.0002gm. Sodium fluoride, 0.05 gm Calcium chloride, 0.01gm Potassium thiocyanate, 1 gm Sorbitol, 1gm. Potassium chloride, 0.05 gm Magnesium chloride, and 0.04 gm Potassium phosphate)
They were dissolved in (985.5) ml of deionized water, then Sodium carboxymethyl cellulose was added, which was dissolved in 100 ml of boiling water and cooled later before its addition to the previous ingredients, and by portable pH meter, the pH was checked and adjusted to 7 [14].
Sample surface preparation
All teeth were washed with deionized water, cleaned and polished with non-fluoridated pumice by rubber cup and low speed handpiece By using double ended diamond disc bur with copious amount of water; to avoid enamel destruction and damaging, the crowns have been separated from the remaining roots at level 2mm below the cement-enamel junction [15]. For the purpose of making the teeth samples in a suitable and uniform design for hardness measure, cylindrical plastic tubes have been used and cut into equal rings with dimensions (20 mm diameter, 15 mm depth) in which the top and bottom sides parallel with each other and flat. Each ring was filled with cold cure acrylic resin and the teeth were embedded in the center of the ring so that the labial surface remained exposed and parallel to the floor. Then the exposed teeth surfaces were polished by grit paper fine silicon carbide (grit 600-800) in a single direction ten times to obtain flat surface for the required test [16]. Then the tooth surface was painted with (acid resistant nail varnish) (Figure 1) except the middle third of the exposed surface that have been covered with adhesive tape and removed later leaving a window 4×4mm.Which was the target area for measurements [11,17].
Figure 1. Teeth sample preparation and exposing of a labial window.
Grouping
The sample was divided randomly into 5 groups, with 10 teeth in each group for the microhardness.
Group 1: (SDF) group, each tooth sample in the group coated with thin layer of Silver Diamine Fluoride varnish (RivaStar) according manufacture instruction, carefully applied the solution from the first silver capsule by using its specified brush, then apply potassium iodide (KI) from the second green capsule and left to dry according to manufacture instructions.
Group 2: (BAG) group, all of the specimens were treated with (Fluoro dip Bioactive) varnish which was applied uniformly with micro brush as a thin film covering the entire surface area, then allowed to dry for 20 second following the material use instructions.
Group 3: (CPP-ACP) group, by using (CPP-ACP, MI varnish), instructions and time of the material setting was based on the manufacturer's leaflet in which each sample was coated with thin layer and left for 20 seconds for dryness and setting.
Group 4: (NaF) group, each tooth sample was painted with a thin layer coating of (NAF 5% Flurodose) varnish and left to dry according to the manufacture instructions.
Group 5:(Control) group, which act as control negative group without any remineralizing intervention. Samples were kept without any treatment just stored in the artificial saliva.
All the groups were kept in daily replaced artificial saliva (Figure 2).

Figure 2. Sample grouping were stored in daily replaced artificial saliva after treatment.
Measurement periods
The measurements of the sample have been observed and recorded at 3 different periods:
1. Baseline measurements: performed initially when the samples were prepared at the beginning of the work before any experimental intervention
2. Demineralizing measurements: were carried out after placing the samples in the previously prepared demineralizing solution, in which the samples were immersed in the demineralizing solution for 72 hours (3 days), after that the specimens were washed with deionized water and then measured.
3. Remineralizing measurements: which was implemented after 2 weeks of applying the various used remineralizing agents? During this time the teeth sample were stored in artificial saliva.
Surface micro-hardness assessment
The enamel surface hardness gives an indication about the mechanical properties of the teeth sample, which was measured by using Vickers microhardness testing machine. This test was achieved in the Technical Institute/Northern Technical University at Mosul city. The measurements were accomplished by application of constant and fixed load of (500) gm for 15 second on the exposed labial window of the tooth surface (Figure 3). By this force the device indentation which was tetra pyramidal indentation produce an impression on the surface and lead to formation of a print which seem as diagonals that observed by scaled microscope with magnification 70X (Figure 4) [18]. The first reading was the baseline or initial measurement, then the second reading was done after the completion of the demineralization process which was after 72 hour, and the final measurement was taken after 2 weeks of the remineralizing treatment.
Figure 3. Teeth sample were measured by Vickers micro-hardness testing machine.
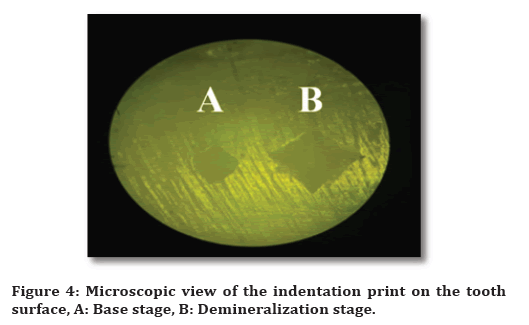
Figure 4. Microscopic view of the indentation print on the tooth surface, A: Base stage, B: Demineralization stage.
Vicker Hardness Number (VHN) was calculated via using the following equation: [19]
VHN=1.854 × F/d2 (Kg/mm2)
In which:
F: The load of the applied indentation (Kg)
D: THE diagonal length of the indentation impression ( in micron).
Statistical analysis
Data description, analysis and demonstration were achieved using (SPSS version 21) Statistical Package for social Science, (Chicago, Illinois, USA).
Repeated Measure One Way (ANOVA) test was used to identify the differences between (K) related means of the continuous quantitative variable thru Bonferroni post hoc test.
Level of significance: (P>0.05: Not significant), (P<0.05: Significant).
Results
Table 1 demonstrate a descriptive and statistical test of hardness among groups by stages, indicated that although micro-hardness in Bioactive and CPP-ACP were higher than other groups in base and demineralization phases but were statistically not significant. While there was statistical significant difference in remineralization stage.
| Levels | Statistics | Groups | F | P value | Partial eta square | ||||
|---|---|---|---|---|---|---|---|---|---|
| Control | SDF | Bioactive | CPP-ACP | NaF | |||||
| Base line Levene test=0.076 P value=0.989 NS |
Minimum | 239.3 | 241.28 | 256.9 | 241.8 | 249.6 | 0.36 | 0.836 | 0.031 |
| Maximum | 324.2 | 305.9 | 326 | 324.2 | 313.1 | ||||
| Mean | 285.4 | 276.444 | 287.17 | 287.49 | 281.5 | ||||
| ± SD | 26.72 | 22.907 | 22.731 | 25.995 | 24.159 | ||||
| Demineralization Levene test=0.462 P value=0.763 NS |
Minimum | 126.4 | 133 | 128 | 138 | 138.2 | 0.488 | 0.745 | 0.042 |
| Maximum | 241.8 | 211.3 | 242 | 233.4 | 224.2 | ||||
| Mean | 181.72 | 167.47 | 188.42 | 183.93 | 178.35 | ||||
| SD | 38.411 | 29.85 | 39.488 | 35.268 | 34.864 | ||||
| Remineralization Levene test=0.292 P value=0.881 NS |
Minimum | 132.9 | 195.9 | 204 | 202.5 | 179.4 | 60.847 | 0.000 * | 0.378 |
| Maximum | 256.2 | 296.2 | 305.8 | 307.8 | 269.2 | ||||
| Mean | 194.17 | 247.9 | 268.15 | 259.31 | 221.36 | ||||
| SD | 40.628 | 36.194 | 35.638 | 32.994 | 36.885 | ||||
Table 1: Descriptive and statistical test of hardness among groups by levels.
Table 2 Show multiple pairwise comparisons of microhardness among groups by stages using Bonferroni post hoc test, the results showed that when comparing the control group with each other, the findings were significant except when comparing the control group with NaF, and when comparing other groups with each other, the results were not significant.
| Groups | Mean Difference | p value | |
|---|---|---|---|
| Control | SDF | -53.73 | 0.020 * |
| Bioactive | -73.98 | 0.000 * | |
| CPP-ACP | -65.14 | 0.002 * | |
| NaF | -27.19 | 1 | |
| SDF | Bioactive | -20.25 | 1 |
| CPP-ACP | -11.41 | 1 | |
| NaF | 26.54 | 1 | |
| Bioactive | CPP-ACP | 8.84 | 1 |
| NaF | 46.79 | 0.064 | |
| CCP-ACP | NaF | 37.95 | 0.248 |
Table 2: Bonferroni post hoc test for hardness comparisons between groups by levels.
Discussion
Measuring of the surface micro-hardness is considered as a precise, practical and efficient tool for evaluation of the tooth surface alteration after de- and remineralization processes [20]. Within limitation of this study and when comparing each group with the other, the results revealed that the hardness tended to increase and regain higher in Bioactive and CPP-ACP groups followed by SDF with significant difference, while the lowest difference was in control followed by NAF group. The outcome of this study was in accordance with many previous researches which have proven that the bioactive glass is more effective in raising the tooth surface hardness compared to CPP-ACP and NaF as remineralizing agents [21]. The findings of this study came in agreement with Ma et al., [22] who revealed that CPP-ACP was observed to be more efficient in remineralization effect that reflected by elevation of the surface micro-hardness. Contrary to the results of this study, other found that CPP-ACP varnish was less effective in remineralizing efficiency and micro hardness restoring than NaF, moreover that considering it as a mere auxiliary, not a substitute for fluoride [23]. The findings of this study were confirmed by Farhadian et al. [24] who assessed that both SDF and NaF varnishes could enhance the reminerlizing potential and surface hardness improvement, with greater efficacy was found in SDF group. However, these results were contrary to Akyildiz et al. [25] who concluded that the remineralizing effect of NaF was more efficient significantly than SDF when measuring the hardness of the tooth surface.
Conclusion
Within limitation of this study, all of remineralizing agents that have been used have an efficacious and valuable effect on the tooth remineralization and surface hardness improvement. Generally Bioactive and CPPACP groups were higher than others. Furthermore, when comparing the groups with artificial saliva, the groups of (BAG, CPP-ACP, and SDF) were higher in effect, while NaF group showed better effect than artificial saliva, but the least efficiency comparing to the others.
References
- Bonchev A, Vasileva R, Dyulgerova E, et al. Self-assembling peptide P11-4: A biomimetic agent for enamel remineralization. Int J Pept Res Ther 2021; 27:899-907.
- Pitts NB, Zero DT, Marsh PD, et al. Dental caries. Nat Rev Dis Primers 2017; 3:1-6.
- Raghu TN, Ananthakrishna S. Remineralization potential of calcium sucrose phosphate on demineralized enamel: Results of an in vitro study. J Int Oral Health 2016; 8:704.
- Ajaj MT, Al-Khateeb SN, Al-Batayneh OB. Effect of different acid etchants on the remineralization process of white-spot lesions: An in vitro study. Am J Dent 2020; 33:43-7.
- Hemagaran G. Remineralisation of the tooth structure—the future of dentistry. Int J PharmTech Res 2014; 6:487–493.
- Chandru TP, Yahiya MB, Peedikayil FC, et al. Comparative evaluation of three different toothpastes on remineralization potential of initial enamel lesions: A scanning electron microscopic study. Indian J Dent Res 2020; 31:217.
- Duangthip D, Chu CH, Lo EC. A randomized clinical trial on arresting dentine caries in preschool children by topical fluorides—18 month results. J Dent 2016; 44:57-63.
- Arifa MK, Ephraim R, Rajamani T. Recent advances in dental hard tissue remineralization: A review of literature. Int J Clin Pediatr Dent 2019; 12:139.
- Indrapriyadharshini K, Kumar PM, Sharma K, et al. Remineralizing potential of CPP-ACP in white spot lesions–A systematic review. Indian J Dent Res 2018; 29:487.
- Karlinsey RL, Mackey AC, Walker TJ, et al. In vitro remineralization of human and bovine white-spot enamel lesions by NaF dentifrices: a pilot study. J Dent Oral Hyg 2011; 3:22.
- https://codental.uobaghdad.edu.iq/wp-content/uploads/sites/14/2021/03/Effect-of-Discoloration-and-Simulated-Tooth-Brushing-on-Color-Stability-and-Surface-Roughness-of-Artificial-White-Spot-Lesions-Treated-with-Resin-Infiltration-Technique.pdf
- DS WS. Effect of water Clove extract on the microhardness and microscopic features of initial caries-like lesion of permanent teeth, compared to fluoridated agent. Scientific J Published College Dent 2011; 110.
- Yang Y, Lv XP, Shi W, et al. 8DSS-promoted remineralization of initial enamel caries in vitro. J Dent Res 2014; 93:520-4.
- Björklund M, Ouwehand AC, Forssten SD. Improved artificial saliva for studying the cariogenic effect of carbohydrates. Curr Microbiol 2011; 63:46-9.
- Farooq I, Khan AS, Moheet IA, et al. Preparation of a toothpaste containing theobromine and fluoridated bioactive glass and its effect on surface micro-hardness and roughness of enamel. Dent Mater J 2021; 40:393-8.
- Al-Sayyab M. The potential effect of combined CO2 laser and fluoride on acid resistance of human dental enamel and root surface in vitro 2000. Careis Res 2007; 41:74-76.
- Mohammadi N, Far MH. Effect of fluoridated varnish and silver diamine fluoride on enamel demineralization resistance in primary dentition. J Indian Soc Pedod Prev Dent 2018; 36:257.
- Mushashe AM, Coelho BS, Garcia PP. Effect of different bleaching protocols on whitening efficiency and enamel superficial microhardness. J Clin Exp Dent 2018; 10:e772.
- Dominguez-Nicolas SM, Wiederhold P. Indentation image analysis for Vickers hardness testing. In2018 15th International Conference on Electrical Engineering, Computing Science and Automatic Control (CCE) 2018; 1-6.
- El-olimy GA. In-vitro evaluation of remineralization efficiency of chicken eggshell slurry on eroded deciduous enamel. Egypt Dent J 2020; 2519-28.
- Taha AA, Patel MP, Hill RG, et al. The effect of bioactive glasses on enamel remineralization: A systematic review. J Dent 2017; 67:9-17.
- Ma X, Lin X, Zhong T, et al. Evaluation of the efficacy of casein phosphopeptide-amorphous calcium phosphate on remineralization of white spot lesions in vitro and clinical research: a systematic review and meta-analysis. BMC Oral Health 2019; 19:1-1.
- Shahmoradi M, Hunter N, Swain M. Efficacy of fluoride varnishes with added calcium phosphate in the protection of the structural and mechanical properties of enamel. BioMed Res Int 2017.
- Farhadian N, Farhadian M, Borjali M, et al. The effect of silver diamine fluoride versus sodium fluoride varnish on the microhardness of demineralized enamel: An in vitro study. Avicenna J Dent Res 2020; 12:13-8.
- Akyildiz M, Sönmez IS. Comparison of remineralising potential of nano silver fluoride, silver diamine fluoride and sodium fluoride varnish on artificial caries: an in vitro study. Oral Health Prev Dent 2019; 17:469-77.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Marwa B Jasim* and Muna S Khalaf
College of Dentistry, University of Mosul, Iraq1Department of Pedodontic and Preventive Dentistry, College of Dentistry, University of Baghdad, Iraq
Citation: Marwa B Jasim, Muna S Khalaf, Efficacy of Varnishes with: Bioactive Glass, Recaldent Technology and Silver Diamine Fluoride in Comparison with Sodium Fluoride on Tooth Surface Micro-hardness (an In Vitro Study), J Res Med Dent Sci, 2022, 10 (4):57-62.
Received: 07-Mar-2022, Manuscript No. JRMDS-22-51581; , Pre QC No. JRMDS-22-51581 (PQ); Editor assigned: 09-Mar-2022, Pre QC No. JRMDS-22-51581 (PQ); Reviewed: 23-Mar-2022, QC No. JRMDS-22-51581; Revised: 28-Mar-2022, Manuscript No. JRMDS-22-51581 (R); Published: 04-Apr-2022
