Research - (2020) Advances in Dental Surgery
Efficacy of Topical Anaesthesia-Lignocaine vs. Emla in the Management of Needle Prick Pain in Children
Maria Anthonet Sruthi and Ganesh Jeevanandan*
*Correspondence: Ganesh Jeevanandan, Department of Paediatric and Preventive Dentistry, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, India, Email:
Abstract
Pain control is an integral part of modern dentistry. Needle injection of local anaesthetic itself proves to be painful for the child. Topical anaesthetic agents are widely used in the field of Paediatric dentistry to reduce pain and apprehension during administration of local anaesthesia. The aim of this study is to evaluate and compare the efficacy of two topical anaesthetic agents—Lignocaine 5% gel and EMLA 5% cream (Eutectic mixture of local anaesthetics—Lignocaine 2.5% and prilocaine 2.5%) in reducing pain during administration of local anesthetic injection in children. Children of the age group between 6 and 9 years of age were selected. The two selected topical anaesthetics were applied on the maxillary buccal vestibule following which the local anaesthetic was administered. The pain responses of the children were evaluated using the Wong Baker Faces Pain Rating Scale at the 5th min and 10th min. The results were then statistically analysed using Independent t-test and ƿ value <0.05 was considered statistically significant. EMLA 5% cream was more effective in pain reduction than Lignocaine 5% gel at the 5th and 10th min. EMLA 5% cream is comparatively better than Lignocaine 5% gel with regards to pain reduction during the administration of local anaesthetic injection in children.
Keywords
Eutectic mixture of local anaesthetics (EMLA), Lignocaine, Pain control, Topical anaesthesia, Topical anesthetic agents, Wong-Baker faces pain rating scale
Introduction
In modern dentistry, dental pain management is one of the most critical aspects which might affect a patient's quality of life. Dental anxiety is a major source of challenge amongst paediatric dentists because children tend to refuse dental treatment. The dentist can overcome the issue of injection pain by altering the pH and temperature of local anaesthetic solution and by reducing the speed of injecting the solution into the tissues [8]. Preparation of tissues before injection is another technique i.e., surface anaesthesia, which includes refrigeration [1], transcutaneous electronic nerve stimulation (TENS), [2]and desensitization of the oral site using topical anaesthetics.
To reduce or relieve painful stimulus caused by needle penetration leading to significant control of pain and anxiety of the patient, the topical anaesthesia is extremely important to a wide variety of dental procedures as the main purpose of using topical anesthetic drugs [3]. A randomized clinical trial by Courtney, et al. stated that higher pain scores were observed in highly anxious participants however, topical anaesthetic agents reduced the effect of anxiety on needle insertion pain [4]. Different kinds of anaesthetic agents are available such as: Gels, lotions, solutions, patches, and lozenges [5]. When administered topically even an ideal local anaesthetic agent should be effective. Topical anaesthesia can cross the oral mucosal membrane and produce analgesia [6]. Conduction of signals are blocked from the terminal fibers of the sensory nerves, thereby producing surface anaesthesia for a depth of 2–3 mm. This change takes place secondary to an alteration in transmission through voltagesensitive sodium channels, resulting in an increment in the action-potential threshold. This attribute of topical anaesthesia enables it to minimize needle insertion pain effectively.
Pioneering work by others on topical anaesthetics in the field of dentistry showed that simple mixtures drug combinations such as benzocaine with amethocaine protracted the duration of anaesthesia because of different latencies of action.
Eutectic mixture of local anaesthetics (EMLA) is a eutectic combination of local anaesthetic drugs- 2.5% prilocaine and 2.5% lidocaine which has gained aficionados for dental procedures, lately. It consists of a mixture 1:1 oil/water emulsion of two crystalline powders (2.5% lidocaine and 2.5% prilocaine), which has a melting point (17°C) compared with the respective individual melting points of the lidocaine base (66-69oC) and the prilocaine base (36-38oC). This new physical property permits the lidocaine/prilocaine eutectic blend to be liquid at mouth temperature and thus facilitate fast absorption of the bases. In this way, it would be able to penetrate intact skin or mucosa into a depth of 5 mm [7].
EMLA provides adequate local anaesthesia in a variety of painful superficial procedures including superficial surgery, epilation,laser surgery, debridement of leg ulcers, cautery of condylomata,and venepuncture [8,9]. Accordingly, in the oral cavity, satisfactory outcome has been proven in biopsies [10], periodontal probes [11] and prior to local anaesthesia [8] EMLA represented a very favorable tolerability profile with transient and mild skin blanching. Adverse side effects of EMLA application on the skin resulted in erythema,but it can be overlooked [8,9].
Originally, EMLA is not indicated for the oral mucosa, however many have reported it as the most effective topical agent in dentistry [12,13]. Furthermore, Al-Asfour et al. [14] observed that EMLA does not meddle with wound healing. The oral mucosa is thinner than dermal tissue and has a more progressive blood supply that encourages rapid absorption of lipophilic drugs. In a study [7], observed whether the plasma concentration of EMLA, which was applied on oral mucosa, is below standard level of toxicity or not. They showed that 30 min application EMLA on oral mucosa produces safe plasma concentration for prilocaine (223 ng/ml) and lidocaine (418 ng/ml) which was considerably below the known toxic level of both prilocaine (4.4 μg/ml) and lignocaine (6.0 μg/ml). EMLA is available at the range dosage of 2.5–5%. Effective duration for 5% EMLA has been accounted to be of 2 min and 10 min [14,15] which is as effective as longer intraoral application times.
Our department is passionate about childcare, we have published numerous high-quality articles in this domain over the past 3 years [16- 34]. With this inspiration, we planned to pursue research on the various methods by which pain management in children can be established.
Therefore, the aim of this study is to compare and evaluate the effectiveness of two topical anaesthetic gels on needle insertion pain during administration of maxillary buccal infiltration at two-time intervals.
Materials and Methods
The randomized controlled trial compared the effectiveness of two topical anesthetic agents, i.e., 5% lignocaine gel (LIGNOSPAN-O) and 5% EMLA (emla, Astra Zeneca) cream. The study was conducted in the Department of Paediatric and Preventive Dentistry, Saveetha Dental College during the months Nov-Dec 2019. The Ethical clearance for the study was obtained from the Institutional Ethical Committee. Written informed consent was obtained from the parents of the participating children prior to the trial by explaining to them the boons and banes of the study. For sample size calculation, a sampling error of 5% was considered, the power was set to 80% and a minimum sample size of 26 was obtained. The study consisted of 30 healthy children in the age group of 6-10 years. Children of this age group were selected since the cognitive skills necessary to use the pain scale for pain assessment have not been developed in children less than 6 years [35]. Prior to the participation in this study, medical history was acquired from all the participants, and a brief oral examination and radiographic assessment was done.
Inclusion criteria
The children were required to present with at least one tooth indicated for pulpectomy in the maxillary arch.Children falling under the category of ASA I and ASA II were included in the trial.
Exclusion criteria
Children with a history of hypersensitivity reactions to anaesthetic agent.
Recent trauma to oral tissues.
Children who had systemic illness and those who were immune compromised.
Children who were unable to understand the numerical rating scale.
The children were randomly divided into two groups: Group A being 5% lignocaine gel and Group B being 5% EMLA cream. Randomization was done for the included participants using the lottery method.
A common anaesthetic agent such as Lignocaine was used in this study to duplicate the familiar practise in a clinical setup. The site of application of the topical anaesthetic agent was dried with 2 × 2-inch gauze. The topical anesthetic gel was applied to the test area using a cotton swab applicator that was completely dipped in the gel for 5 min. The site was then covered with dry gauze. After 5 min, using a short 30-gauge needle, 0.5 ml of local anaesthetic agent (2% Lignocaine HCl with 1:100,000 Adrenaline) was administered preceded by aspiration through infiltration into the buccal vestibule. The needle was concealed to not create an anxious situation that could alter the child’s pain perception. The child was advised to quantify the pain perception using Wong Baker Faces Pain Scale by choosing a face that best describes the pain experienced by him/her now of the needle prick (Figure 1). After 10 min, a concealed second needle prick was carried out at the same site without application of the test agent and pain perceived was again recorded. This was done to check the duration of efficacy of the test agent.
Figure 1: Pain assessment scale given by donna wong and connie baker.
The data acquired was analysed using SPSS Software version 23.0. For intergroup analysis (Lidocaine x EMLA), the Independent t-test was applied. Æ¿ value less than 0.05 was statistically significant.
Results
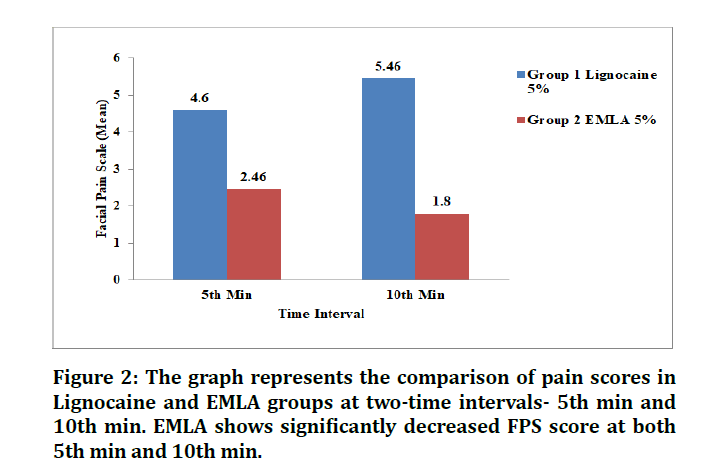
The study group consisted of 14 males and 16 females with an age ranging from 6- 10 years (Mean=7.033 ± 0.25). Results of FPS scores for Group A and Group B were analysed using Independent t-test. The Mean FPS score for Group A and Group B was 4.60 and 2.46 at the 5th min respectively and 5.46 and 1.80 for the 10th min (Table 1). A graphical representation of the differences in mean pain scores among Group A and Group B is depicted in Figure 2. Difference of scores for pain during needle insertion for lignocaine 5% and EMLA 5% were found to be statistically significant (Æ¿<0.05) (Table 2).
Figure 2: The graph represents the comparison of pain scores in Lignocaine and EMLA groups at two-time intervals- 5th min and 10th min. EMLA shows significantly decreased FPS score at both 5th min and 10th min.
| Groups | N | Mean Pain Score | Mean Pain Score |
|---|---|---|---|
| 5th min | 10th min | ||
| Group A- Lignocaine 5% | 15 | 4.60 ± 0.62 | 5.46 ± 0.50 |
| Group B- EMLA 5% | 15 | 2.46 ± 0.66 | 1.80 ± 0.50 |
Table 1: Mean FPS Scores for Group A and Group B at two-time intervals.
| Time point | Ç· value | |
|---|---|---|
| Lignocaine vs. EMLA | 5th min | Ç·=0.04 |
| 10th min | Ç·=0.05 |
Table 2: Sensitivity to needle pain Lignocaine vs. EMLA.
Discussion
In dental offices, dental anaesthesia is among the main procedures associated with patient phobia and due to the fear of anaesthetic puncture it is leading a considerable number of individuals to avoid dental treatments [36].
Topical anaesthesia can be defined as loss of sensation on the mucous membrane that is produced by direct application. Topical anesthetic, that is cocaine was the first local anesthetic which was discovered in 2013 by Heatonet al. [37]. Topical anaesthesia targets the free nerve-endings that reversibly blocks nerve conduction close to the site of administration, which in turn induces a brief loss of sensation in that area. The permeability of cell membrane to sodium ions is decreased, and therefore, nerve conduction is blocked. This ultimately decreases the depolarization and increases excitability threshold until the capability to result action potential is completely lost [38]. Topical anesthetic agents do not incorporate vasoconstrictor as it weakens the mucosal permeability. In addition, topical anaesthetics are more concentrated than injectable ones to promote diffusion within the mucosa [39].
Local anaesthetics are classified into ester linkage agents (benzocaine) and amide linkage agents (lignocaine) and are the most predominantly used topical anesthetic agents. Lignocaine is the most widely used local anesthetic agent and is an antiarrhythmic drug. Peripheral nociceptor sensitization and central hyperexcitability slows down by the topical application of lidocaine [40].
A clinical study of 510 extractions (Grade II and III) were carried out with lignocaine hydrochloride gel 5% and bupivacaine hydrochloride gel 5% as topical agents, and it was reported that 5% lignocaine hydrochloride gel was better than 5% bupivacaine hydrochloride gel [41].
Holst et al. [42] was the first to study using EMLA by comparing its pain reduction effect during a needle insertion to a placebo and it was found that EMLA was amazingly effective in reducing pain experience. Since then several studies have been conducted to investigate its efficacy for pain reduction during injection.
Vickers et al. [43] evaluated the efficacy of 5% EMLA cream, 5% xylocaine and NUM (lignocaine 5%, amethocaine 1.7%) and found EMLA to be the most effective topical anesthetic agent in reducing the pain experienced during needle insertion. Another study evaluated the efficacy of 5% EMLA cream, 10% benzocaine and 10% lidocaine, and found EMLA 5% cream significantly reduced the pain threshold and was superior in performance to all other topical anesthetics [44].
Nayak compared EMLA 5%, lignocaine 5% and benzocaine 18%, in 6–12 years aged children and found out that EMLA 5% was the most effective agent in pain reduction than lignocaine and benzocaine. Franz compared the efficacy of liposome-encapsulated 2% ropivacaine, liposome-encapsulated 1% ropivacaine, a eutectic mixture of 2.5% lidocaine and 2.5% prilocaine (EMLA), and liposomal placebo gel and found that EMLA to be superior to other agents. Another clinical trial revealed that 2.5% lignocaine+2.5% prilocaine gave better results than 20% benzocaine in reducing needle insertion pain in maxillary vestibule [45].
The present study was conducted among 30 children (14 males and 16 females) in the age range of 6- 10 years to evaluate the efficacy of 5% lignocaine and 5% EMLA as a topical anesthetic agent. To standardize the protocol, only maxillary arch and therefore buccal infiltration was included. This study showed a significant difference between the mean pain scores in Group A and Group B which was in support with the above studies but contradictory to the study done by Meechan et al. [46] who stated that lignocaine 5% and 5% EMLA were equally effective.
The superior surface anesthetic property of EMLA could be attributed to its high pH (pH 9.6). This is in accordance with who stated that an increase in the pH increases the potency of the topical anesthetic agent.
It was seen that EMLA had a low viscosity due to which localization of this topical anaesthetic to the desired site on the oral mucosa was troublesome. To overcome this difficulty, Svensson, et al. [47] supported the use of orahesive bandages to localize this drug. However, Tulga, et al. [15] have reported difficulty in sticking these bandages onto the oral mucosa. In our study, a dry gauze piece was placed at the site (buccal vestibule) to overcome the low viscosity of the cream. However, the same will not be possible at other sites in the oral cavity.
When we correlated the repercussions of the anesthetic effect over the evaluated times (5 and 10 min) statistically significant outcomes were attained in favour of EMLA for the 5th as well as the 10th min whereas lignocaine showed effective results at the the 5th min after the application of the topical anaesthetic. This fact is corroborated by other studies that reveal the duration of anaesthetic effect over 20 minutes for EMLA [48, 49].
Lignocaine 5% ointment indicated the mean time of onset of action of 105s as against the 15s suggested in literature. Roghani et al. suggested 1-2 minutes of contact with the mucosa for lignocaine since it has a relatively weak surface anaesthetic activity. EMLA cream had the slowest onset of action (138s ± 15.49). The slow onset of action of this preparation can be ascribed to its low viscosity and consequent difficulty in localizing it to the site of application [44].
Holst et al. [42] recommended an application time of 5 minutes to be the tolerable limit of practical usefulness for EMLA cream. Others recommended a four-minute application and found that the maximum analgesic effect is reached at 13±8 minutes. Vickers et al. [43] used a 2-minute application time and observed a significant reduction of pain on needle penetration.
In the present study, a topical application for a minimum of 5 minutes was observed to be essential for obtaining reasonably good surface anesthesia for both Group A and Group B. However, this study did not evaluate the onset of action of anaesthesia.The unpleasant taste was one of the complaints of the participants, and the addition of flavour would facilitate their acceptance, especially in paediatric dentistry. No adverse effects were observed with any of the agents during the present study. Also, it was observed that no subject gave a zero-pain score for any of the agents.
There are various alternatives to topical anesthesia, but they are much more sensitive, for example computer-controlled local anesthetic delivery (CCLAD) and TENS. CCLAD works on the idea of slow delivery of local anesthesia. In a clinical trial, comparing CCLAD with traditional methods in pediatric patients showed that CCLAD gave excellent results than the traditional technique. TENS device stimulates the neurons that in turn activates the descending inhibitory system, and hence, hyperalgesia is reduced [50].
Conclusion
Based on the results obtained in the present study, it can be inferred that EMLA 5% cream is comparatively better than Lignocaine 5% gel at both the time intervals with regards to pain reduction during the administration of local anesthetic injection in children.
Acknowledgement
I would like to express my gratitude to Dr. Ganesh.J for guiding me in this study.
Conflict of Interest
The authors of this study confirm that there is no conflict of interest in the publication of this paper.
References
- Ghaderi F, Banakar, S, Rostami S. Effect of pre-cooling injection site on pain perception in pediatric dentistry: A randomized clinical trial. Dent Res J 2013; 10:790.
- Choudhari SR, Solanki PJ, Vispute GK, et al. Efficacy of transcutaneous electronic nerve stimulation in alleviating pain during inferior alveolar nerve block injections in pediatric dentistry. Int J Pedodontic Rehab 2017; 2:69.
- Meechan JG. Intra-oral topical anaesthetics: A review. J Dent 2000; 28:3-14.
- Courtney DJ, Agrawal S, Revington PJ. Local anaesthesia: To warm or alter the pH? A survey of current practice. J Royal College Surgeons Edinburgh 1999; 44:167-171.
- Chan SK, Karmakar MK, Chui PT. Local anaesthesia outside the operating room. Hong Kong Med J 2002; 8:106-113.
- Ship II, Williams AF, Osheroff BJ. Development and clinical investigation of a new oral surface anesthetic for acute and chronic oral lesions. Oral Surg Oral Med Oral Pathol 1960; 13:630-636.
- Vickers ER, Marzbani N, Gerzina TM, et al. Pharmacokinetics of EMLA cream 5% application to oral mucosa. Anesthesia Progress 1997; 44:32.
- Parker JF, Vats A, Bauer G. EMLA toxicity after application for allergy skin testing. Pediatrics 2004; 410-411.
- Buckley MM, Benfield P. Eutectic lidocaine/prilocaine cream. Drugs 1993; 46:126-151.
- Meechan JG. The use of EMLA for an intraoral soft-tissue biopsy in a needle phobic: A case report. Anesthesia Progress 2001; 48:32.
- Friskopp J, Nilsson M, Isacsson G. The anesthetic onset and duration of a new lidocaine/prilocaine gel intra-pocket anesthetic (oraqixr) for periodontal scaling/root planing. J Clin Periodontol 2001; 28:453-458.
- Meechan JG, Thomason JM. A comparison of 2 topical anesthetics on the discomfort of intraligamentary injections: A double-blind, split-mouth volunteer clinical trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 1999; 87:362-365.
- McMillan AS, Walshaw D, Meechan JG. The efficacy of Emla® and 5% lignocaine gel for anaesthesia of human gingival mucosa. Br J Oral Maxillofac Surg 2000; 38:58-61.
- Al–Asfour A, Al–Melh M, Andersson L, et al. Healing pattern of experimental soft tissue lacerations after application of novel topical anesthetic agents-An experimental study in rabbits. Dent Traumatol 2008; 24:27-31.
- Tulga F, Mutlu Z. Four types of topical anaesthetic agents: Evaluation of clinical effectiveness. J Clin Pediatr Dent 1999; 23:217–220.
- Ravikumar D, Gurunathan D, Gayathri R, et al. DNA profiling of streptococcus mutans in children with and without black tooth stains: A polymerase chain reaction analysis. Dent Res J 2018; 15:334.
- Dhanalakshmi Ravikumar SN, Ramakrishna M, Sharna N, et al. Evaluation of McNamara’s analysis in South Indian (Tamil Nadu) children between 8-12 years of age using lateral cephalograms. J Oral Biol Craniofac Res 2019; 9:193–97.
- Ravikumar D, Jeevanandan G, Subramanian EM. Evaluation of knowledge among general dentists in treatment of traumatic injuries in primary teeth: A cross-sectional questionnaire study. Europ J Dent 2017; 11:232–237.
- Ravindra V, Rekha V, Annamalai S, et al. A comparative evaluation between dermatoglyphic patterns and different terminal planes in primary dentition. J Clin Exp Dent 2018; 10:1149–1154.
- Ravindra V, Rekha CV, Annamalai S, et al. A comparative evaluation between cheiloscopic patterns and the permanent molar relationships to predict the future malocclusions. J Clin Exp Dent 2019; 11:553–557.
- Govindaraju L, Jeevanandan G, Subramanian EM. Comparison of quality of obturation and instrumentation time using hand files and two rotary file systems in primary molars: A single-blinded randomized controlled trial. Europ J Dent 2017; 11:376–379.
- Govindaraju L, Jeevanandan G, Subramanian EM. Knowledge and practice of rotary instrumentation in primary teeth among Indian dentists: A questionnaire survey. J Int Oral Health 2017; 9:45.
- Nair M, Jeevanandan G, Vignesh R, et al. Comparative evaluation of post-operative pain after pulpectomy with k-files, kedo-s files and mtwo files in deciduous molars -A randomized clinical trial. Brazilian Dent Sci 2018; 21:411.
- Jeevanandan G, Ganesh S. Kedo file system for root canal preparation in primary teeth. Indian J Dent Res 2019; 30:622–624.
- Panchal V, Jeevanandan G, Subramanian EM. Comparison of instrumentation time and obturation quality between hand k-file, h-files, and rotary kedo-s in root canal treatment of primary teeth: A randomized controlled trial. J Indian Society Pedodont Preventive Dent 2019; 37:75–79.
- Subramanyam D, Gurunathan D, Gaayathri R, et al. Comparative evaluation of salivary malondialdehyde levels as a marker of lipid peroxidation in early childhood caries. Europ J Dent 2018; 12:67–70.
- Vignesh R, Ditto Sharmin C, Annamalai S, et al. Management of complicated crown-root fracture by extra-oral fragment reattachment and intentional reimplantation with 2 years review. Contemporary Clin Dent 2019; 10:397–401.
- Ramadurai N, Gurunathan D, Samuel AV, et al. Effectiveness of 2% articaine as an anesthetic agent in children: Randomized controlled trial. Clin Oral Investigations 2019; 23:3543–3550.
- Panchal V, Gurunathan D, Shanmugaavel AK. Smartphone application as an aid in determination of caries risk and prevention: A pilot study. Europ J Dent 2017; 11:469–474.
- Panchal V, Jeevanandan G, Subramanian EM. Comparison of post-operative pain after root canal instrumentation with hand k-files, h-files and rotary kedo-s files in primary teeth: A randomised clinical trial. Europ Archives Paediatr Dent 2019; 20:467–472.
- Jeevanandan G, Govindaraju L. Clinical comparison of kedo-s paediatric rotary files vs manual instrumentation for root canal preparation in primary molars: A double blinded randomised clinical trial. Europ Archives Paediatr Dent 2018; 19:273–278.
- Samuel SR, Acharya S, Rao JC. School interventions-based prevention of early-childhood caries among 3-5-year-old children from very low socioeconomic status: Two-year randomized trial. J Public Health Dent 2020; 80:51–60.
- Ramakrishnan M, Dhanalakshmi R, Subramanian EM. Survival rate of different fixed posterior space maintainers used in paediatric dentistry-A systematic review. Saudi Dent J 2019; 31:165–172.
- Vishnu Prasad S, Kumar M, Ramakrishnan M, et al. Report on oral health status and treatment needs of 5-15 years old children with sensory deficits in Chennai, India. Special Care Dent 2018; 38:58–59.
- Barcohana N, Duperon DF, Yashar M. The relationship of application time to EMLA efficacy. J Dent Children 2003; 70:51-54.
- Krane JE, Tyler DC. Post-operative pain management in children. Anaesth Clin North America 1989; 7:159-160.
- Heaton LJ, Leroux BG, Ruff PA, et al. Computerized dental injection fear treatment. J Dent Res 2013; 92:37-42.
- Wulf H, Biscoping J, Beland B, et al. Ropivacaine epidural anesthesia and analgesia versus general anesthesia and intravenous patient-controlled analgesia with morphine in the perioperative management of hip replacement. Ropivacaine hip replacement multicenter study group. Anesthesia Analgesia 1999; 89:111–116.
- Kumar M, Chawla R, Goyal M. Topical anesthesia. J Anaesthesiol Clin Pharmacol 2015; 31:450–456.
- Jorge LL, Feres CC, Teles VE. Topical preparations for pain relief: Efficacy and patient adherence. J Pain Res 2011; 4:11.
- Bhushan NS, Nayak RN. A comparison of the efficacy of topical application of lignocaine hydrochloride 5% gel and bupivacaine hydrochloride 5% gel for extraction of teeth. J Maxillofa Oral Surg 2010; 9:119-126.
- Holst A, Evers H. Experimental studies of new topical anaesthetics on the oral mucosa. Swedish Dent J 1985; 9:185-191.
- Vickers ER, Punnia–Moorthy A. A clinical evaluation of three topical anaesthetic agents. Australian Dent J 1992; 37:266-270.
- Roghani S, Duperon DF, Barcohana N. Evaluating the efficacy of commonly used topical anesthetics. Pediatr Dent 1999; 21:197–200.
- Andersson L, Behbehani E. Reduction of pain from needle stick in the oral mucosa by topical anesthetics: A comparative study between lidocaine/prilocaine and benzocaine. J Clin Dent 2005; 16:53-56.
- Meechan JG, Donaldson D. The intraoral use of EMLA cream in children: A clinical investigation. ASDC J Dent Children 1994; 61:260-262.
- Svensson P, Petersen JK. Anesthetic effect of EMLA occluded with orahesive oral bandages on oral mucosa. A placebo-controlled study. Anesthesia Progress 1992; 39:79.
- List T, Mojir K, Svensson P, et al. A new protocol to evaluate the effect of topical anesthesia. Anesthesia Progress 2014; 61:135-144.
- Oʼneill R. Monheimʼs local anaesthesia and pain control in dental practice. Pain 1985.
- Mittal M, Kumar A, Srivastava D, et al. Pain perception: Computerized versus traditional local anesthesia in pediatric patients. J Clin Pediatr Dent 2015; 39:470-474.
Author Info
Maria Anthonet Sruthi and Ganesh Jeevanandan*
Department of Paediatric and Preventive Dentistry, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, IndiaCitation: Maria Anthonet Sruthi, Ganesh Jeevanandan,Efficacy of Topical Anaesthesia-Lignocaine vs. Emla in the Management of Needle Prick Pain in Children, J Res Med Dent Sci, 2020, 8 (7): 186-192.
Received: 15-Sep-2020 Accepted: 16-Oct-2020 Published: 23-Oct-2020