Research - (2021) Volume 9, Issue 4
Efficacy of Kinesio Taping in Attenuating Work-Related Low Back Pain among Physiotherapy and Nursing Professionals
Mohammad Miraj1*, Mazen AlQahtani1, Msaad AlZhrani1, Ahmad Alanazi1, Zafar Hasan2 and Tanuj Garg3
*Correspondence: Mohammad Miraj, Department of Physiotherapy, College of Applied Medical Sciences, AlMajmaah University, Saudi Arabia, Email:
Abstract
Background: Work related low back pain (WRLBP) is one of the commonest problems classified under WMSDs. Among various healthcare professionals, Physiotherapists and Nurses are most prone for developing WRLBP by virtue of nature of their jobs. Among various physiotherapeutic treatment modalities, Kinesio taping (KT) is sought to be one of the most promising techniques to alleviate the symptoms of WRLBP.
Objectives: To measure the efficacy of kinesio taping (KT) along with conventional physiotherapy (moist heat plus lumbar stabilization exercises) on WRLBP.
Methodology: 42 male physiotherapy and nursing professionals, aged 25 to 55 years and experiencing WRLBP for more than 90 days with pain scores greater than 4 on Visual analogue Scale (VAS) were randomly assigned to an experimental and a control group. The Control Group A (n=20) were given conventional Physiotherapy treatment (moist heat along with lumbar stabilization exercises) whereas for the Experimental Group B (n=20) kinesiotaping (KT) was added to conventional physiotherapy. The outcome measures taken for assessment were VAS for pain measurement, Roland Morris Disability Questionairre (RMDQ) for functional disability, Tampa Scale for fear of movement (kinesiophobia) and Trunk ROM.
Results: Statistically significant improvement were recorded for all outcome variables in both groups (A and B) when compared within the group from baseline readings after 2nd and 4th weeks of intervention. both the patients’ groups, aged 36.5±8.45 years when measured within the groups on both 2nd and 4th week. However, for between groups comparison, the Experimental group B (KT+Conventional PT) recorded better clinical outcomes than the conventional physiotherapy with statistically significant differences measured for pain, forward flexion as well as side to side rotation of the trunk (p<0.05) at the end of 4th week.
Conclusion: Kinesiotaping is an effective treatment modality along with lumbar stabilization exercises for treating WRLBP patients.
Keywords
WRLBP, Kinesio taping, Lumbar stabilization exercises
Introduction
Work related Low back pain (WRLBP) is one of the major occupational health hazards across the globe affecting millions of workers worldwide. Previous literature suggests that the overall burden of LBP arising from these ergonomic exposures is responsible for 60.1 million disability adjusted life years (DALY) in 2015, witnessing a whooping increase by 54% since 1990’s [1]. It is responsible for causing 77% of the overall disabilities (the highest in the world) with major incidences reported from among low income and middle-income countries, including Asia, Africa, and Middle East in the last couple of years [2]. In one of the hallmark reports published after compilations from top 40 meaningful publications covering almost twothird of the world it was reported that prevalence of chronic LBP among the working class will be 2·5 times more (95% CI 1·21–4·10) than in non-working populations for reasons that were not clear [3]. WRLBP not only affects a person physically in terms of affecting mobility, causes long term disability as well as adversely affects quality of life but also adds to the economic burden because of the direct (health-care) costs, and indirect (work absenteeism or productivity loss) costs, associated with it [4].
Literature review suggests that some professions are susceptible for developing LBA quite early by the nature of their jobs. While some professions are more prone to develop low back ache as compared to others, vast number of studies have been published regarding association of various job factors including long working hours, prolonged sitting, standing, poor posture, frequent bending, stooping, repetitive strains etc. to develop into mechanical LBA. Among the various professionals, healthcare professionals and especially the physiotherapists and nurses have reported to have the highest prevalence of LBA. In some of the studies by published recently, Ibrahim et al. had reported prevalence of WRLBP among nurses was 74.8% in Malaysia, whereas Boukerma et al. reported that 66.6% nurses working in hospitals suffer from LBA in Algeria, with pain been significantly higher between age group of 30-49 years of age group and with 2-5 years of seniority in the hospital [5,6]. Similarly, in one of the other research studies conducted in India, a prevalence of 66% of LBA was reported among physiotherapists in India [7]. Likewise In KSA, a study by Gaowgzeh et al. reported 61.7% of nurses in Jeddah complained of LBP [8]. Though, studies with reference to various health professionals are quiet low but whatever literature is available, among them nurses anf physiotherapists are one of the most vulnerable groups exposed to LBA [9,10].
Physiotherapy which is among of the most sought pathies in the world especially with context to medical issues and problems concerned with movement disorders, it has been observed that different treatment modalities and techniques have been used from time to time to measure their effectiveness in managing the problems as well as addressing the various physical issues concerned with LBA. These methods range from using electrotherapeutic modalities to manual therapies (chropractic to kinesiology to exercises, spinal manipulations to various educational programs [11-14].
Kinesiotaping is one of the latest additions in the physiotherapist’s treatment kit and is a novel rehabilitation method for facilitating body’s natural healing process without causing any restriction to the joint’s ROM as well as providing support and stability to muscles and joints [15]. Developed by Japnese maverick Chiropractic, Kenzo Kase in the mid 70’s, Kinesiotaping is a technique used in the clinical management of people with chronic LBA or nonspecific LBP [16]. The technique advocates the use of these novel tapes, which claim to have properties same as skin and have more elasticity than the conventional bandage. While the tape could be stretched up to 120-140% of original length but for all practical purposes, Kase (2003) has recommended to use 25-50% of its original length [16,17]. The tape is attached to the skin, thereby elevating the epidermis causing decrease in nociceptive stimulus.
Literature review suggests that few numbers of clinical trials been performed worldwide regarding its efficacy and comparing it with Saudi Arabia, even lesser number of studies were conducted [18-20]. While few literatures suggest its effectiveness, some set of other studies, lacks proof or minimal evidence regarding its clinical effectiveness. Moreover, the above studies, were conducted among general patient population. Therefore, the present study has been conducted upon nursing professionals who suffer from mechanical low back pain of non-specific origin and effectiveness of KT application was evaluated with respect to certain clinical and functional outcomes namely, pain, functional disability, lumbar range of motion (LROM) and kinesiophobia.
Methodology
Study design
The study design was a randomized controlled trial (pretest-posttest experimental control group design), where the physiotherapy and nursing professionals were recruited from AIHMS, New Delhi as well as College of Applied Medical Sciences, Rehabilitation center located at AlMajmaah city which lies 200 kms away from the national capital, Riyadh. The study protocol and ethical clearance were approved from Research Ethical Committee. The study commenced from November 2019 and completed in March 2020.
Subjects
A total of 42 male physiotherapy and nursing professionals aged 23 to 55 years and experiencing WRLBP for more than 90 days with pain scores greater than 4 on Visual analogue Scale (VAS) were recruited for the study [21]. The exclusion criteria were prevalence of any medical conditions including Spondylolisthesis, , History of spinal surgeries, Osteoporosis, Psychiatric disorders, Serious Cardio-respiratory disease, Spinal tumor or Fracture, Active or recent malignancy, Spinal canal stenosis, Neuropathic pain Large herniated disc, Scoliosis [22]. Those who fulfilled the eligibility criteria and consented to participate were recruited for the study.
Methods
Using statistical power of 80%, effect size of 0.20 and level of significance set at 0.05, the minimum sample size of 36 participants was needed to detect difference of 2 cm in pain intensity between the groups on the VAS Index. Assuming a drop out of 20% due to some personal reason or developing allergy due to tape, a total of 42 subjects were required. The participants were then randomly assigned into experimental (n=21) and control group (n=21). The Conventional physiotherapy treatment group (Control group) were given moist heat pack along lumbar stabilization exercises whereas in the Experimental Group, patients were given conventional physiotherapy along with KT taping at the thoracolumbar fascia [23,24] (Figure 1). Thorough physical assessment of patient was done with pre-treatment recordings been made for various outcome variables namely VAS used to measure pain, Trunk flexion ROM measured via using Modified Schober’s Test, Roland-Morris Disability Questionnaires for measuring low back functional disability and Tampa Scale for measuring fear of movement among the LBP patients (Kinesiophobia), using the standard methods [25-28]. The lumbar stabilization exercises comprise of set of standardized exercise protocol including lunge, standing forward bend, kneeling forward bend, extended side stretch, warrior posture, standing lateral posture, kneeling lateral posture and chair posture to be performed thrice in a week for a month [29].
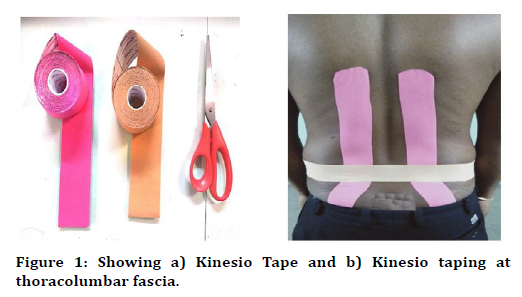
Figure 1. Showing a) Kinesio Tape and b) Kinesio taping at thoracolumbar fascia.
Application of kinesio taping
Before the application of Kinesio taping, skin allergy test was done mandatory for all participants included in experimental group. The test was conducted by application of a small patch of kinesio tape on patient’s abdomen and was left for a duration of 24 hours. All the patients were instructed to remove the tape immediately if any sort of irritation or itching is felt and report this to the research team as soon as possible. Such patients were examined next day at the site of application for any allergic reaction. Those participants who developed allergic were not included in the study.
The Intervention group (n=20) was supposed to be treated with Kinesiotape (Kinesio Tex Gold, 2in x 103.3ft, Kinesio®, Albuquerque, New Mexico, USA) as instructed by Kenzo Kaser KT Manual [16,30]. The standard operational procedure required the patient to be instructed beforehand the steps for the application with patient at ease. The part where tape must apply (Thoracolumbar region) in the current condition, the skin of the back is cleaned with alcohol swabs to ensure the application part is devoid of any lotions, creams etc. Unwanted hairs have to be removed if any of it is present. The therapist stands behind the back of the patient. The initial anchor point of the tape (4-5 cm) was removed carefully from the paper backing and at the same time the patient was asked to perform maximal forward flexion. The base of tape was applied to the paraspinal muscles at T7, located at inferior angle level of scapula without any tension. Base of tape was stabilized, and pressure was applied in downward direction to increase tissue tension. The tape was then applied over the paraspinal muscles to the lumbosacral junction. At the Lumbosacral junction, the tape was directed at 45 degrees angle towards the sacroiliac joint. The patient was guided to return to original position to rest before applying the second piece. Second longitudinal part of kinesio tape was put along the paraspinals on other side. Patient was asked to extend the lumbar spine to 15 degree to apply the horizontal piece of kinesio tape. Holding the kinesio tape by its tail, it was pulled gently with mild tension and applied along Jacobs’s line (the line drawn between the right and left posterior superior iliac crests). The tails were applied to the iliac crests with minimal tension on the ends. The tape was gently rubbed to activate the glue. The method required skilled experienced PT practitioner who had trained and certified for kinesio taping for all 3 levels (KT 1, 2 and 3).
The treatment for both the groups went for one month with readings for the various outcome variables were measured on 2nd and 4th week respectively.
Statistical analysis
The data were verified for the assumptions of normality using Kolmogorov–Smirnov test using Statistical Package of Social Science (SPSS) version 22.0 (Chicago, IL). The normally distributed data were then assessed for mean, SDs, t-values and p values soas to draw inferences regarding comparison within and between the groups. Participant’s characteristics and demographic data were compared between groups with unpaired t test and Mann-Whitney U tests.
Results
The baseline characteristics values for the demographic characteristics for all the participants are depicted in (p>0.05). The sample comprised of both physiotherapy and nursing professionals suffering from WRLBP. In Experimental group B(C+KT) i.e conventional therapy given along with Kinesiotaping, most subjects were from nursing (60.8%) whereas in control group (Conventional Treatment group), majority of patients were from physiotherapy (52.1%). The final study sample comprised of 40 subjects(n=40) as 2 participants (1 from each group) dropped out. The treatment for both groups continued for 1 month with readings measured for all the outcome variables at 0 week (Baseline line), 2nd week and 4th week (Table 1).
| Variables | GroupA (Conv. Tt) (n=20) (M ± SD) |
Group B (Conv.+KT) (n=20) (M±SD) |
P value |
|---|---|---|---|
| Age | 38.21 ± 8.45 | 36.5 ± 6.51 | 0.19 |
| Weight | 64.66 ± 9.74 | 67.84 ± 7.72 | 0.21 |
| Profession | |||
| Physiotherapy | 12(52.18%) | 9(39.13%) | 0.47 |
| Nursing | 11(47.82%) | 14(60.8%) | 0.63 |
| Work Experience | |||
| 1–5 years | 8(40%) | 6(26%) | 0.43 |
| 6–10 years | 11(55%) | 12(52.13 %) | 0.27 |
| >10 years | 4(5%) | 5(21.73%) | 0.89 |
| Place of Work | |||
| General Hospital | 12(52.18%) | 13(65%) | 0.21 |
| Rehabilitation Center | 9(39.13%) | 6(26%) | 0.63 |
| University Department | 2(8.83%) | 4(9%) | 0.41 |
Table 1: Showing baseline characteristics of the participants in between Group A and Group B.
VAS Scores
Comparing VAS scores between the two groups, it was observed that both groups registered statistically significant differences in the pain scores compared to the baseline values both at week 2nd and 4th. Between groups comparison revealed that there was no significant change in the experimental group (C+KT) as compared to Control (t=1.6, p=0.74), however statistical difference was noted at week 4 in experimental group (1.73 ± 1.54) as compared to the control group (2.47 ± 1.42) (p<0.05*).
Trunk ROM Measurements
The groups were compared for the trunk movements using measurements for flexion, extension, side flexions (both right and left side) as well as trunk rotations (both right and left). For Within group comparison, both the Groups i.e. group A and B displayed significant difference in all the trunk movements from the baseline values measured at week 2 and week 4 (p**<0.05). For between group comparisons, it was noted though the mean ranges for all movements were better in experimental group (KT+ Conventional PT Therapy) at both week 2 and 4, but the difference was insignificant for majority of trunk movements, except trunk flexion and rotation of both sides but only at week 4 (p**<0.05) (Table 2 and Figure 3).
| TFROM | TEROM | RSTFROM | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Weeks | Gp.A | Gr.B | P Value | Gp.B | Gp.A | P value | Gp.A | Gp. B | P value |
| W0 | 4.57 ± 2.34 | 4.75 ± 1.98 | 0.93 | 1.68 ± 0.72 | 1.29 ± 0.93 | 0.74 | 13.45 ± 1.56 | 12.45 ± 1.37 |
0.67 |
| W2 | 5.62 ± 1.36 | 5.69 ± 1.45 | 0.68 | 2.37 ± 0.85 | 2.99 ± 0.57 | 0.95 | 13.63 ± 0.93 | 13.22 ± 0.71 |
0.53 |
| W4 | 6.42 ± 1.63 | 7.78 ± 1.52 | 0.038* | 3.76 ± 0.56 | 3.87 ± 0.76 | 0.61 | 15.36 ± 0.66 | 15.87 ± 0.93 |
0.79 |
| LSROM | RTRROM | LTRROM | |||||||
| Weeks | Gp.A | Gr.B | P Value | Gp.B | Gp.A | P value | Gp.A | Gp. B | P value (<0.05)* |
| W0 | 11.97 ± 0.63 | 12.36 ± 0.64 | 0.75 | 4.75 ± 0.83 | 4.97 ± 0.92 | 0.74 | 4.73 ± 0.98 | 4.56 ± 0.85 | 0.83 |
| W2 | 12.74± 0.67 | 13.94 ± 0.85 | 0.87 | 5.36± 0.62 | 5.92 ± 0.73 | 0.85 | 5.72 ± 0.67 | 5.95 ± 0.87 | 0.66 |
| W4 | 15.67 ± 0.61 | 15.03 ± 0.55 | 0.36 | 6.58 ± 0.87 | 7.02 ± 0.87 | 0.034* | 6.63 ± 0.65 | 6.69 ± 0.84 | 0.026** |
Table 2: Showing the within group comparison for all Trunk ROM for 0,2 and 4th week after intervention.
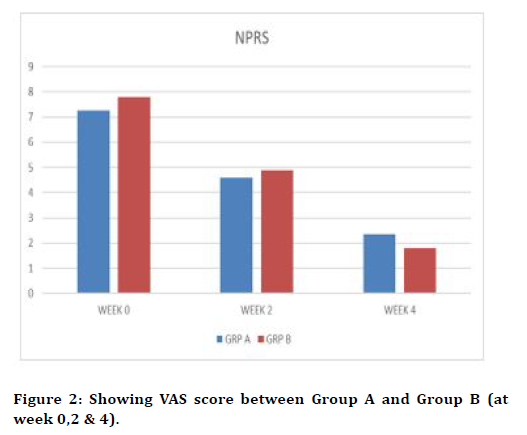
Figure 2. Showing VAS score between Group A and Group B (at week 0,2 & 4).
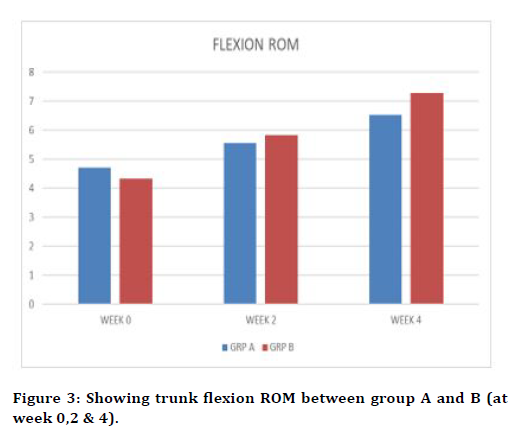
Figure 3. Showing trunk flexion ROM between group A and B (at week 0,2 & 4).
RM Disability Scores
Groups A & B, measured to have significant statistical different in their scores as compared to the baseline values both at week 2 and 4 (p*** <0.05). However, for intergroup comparison no statistical differences were observed both at week 2nd and 4th respectively (p=0.93 and p=0.77, P<0.05) (Figure 4).
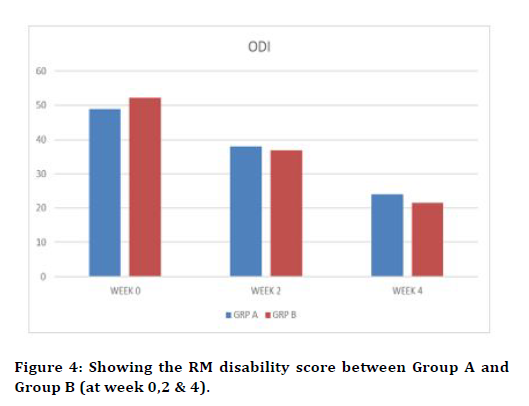
Figure 4. Showing the RM disability score between Group A and Group B (at week 0,2 & 4).
TAMPA kinesiophobia scores
For within group comparison, both groups, A and B measured significant statistical differences in their scores when compared to their baseline values at week 0 to week 2 and week 4(p***<0.05, p<0.005). When compared for between the groups, it was found that Group B i.e. the experimental group (KT+C) scored better than the conventional group (Control) both at week 2 and 4, found to be statistically significant (p*=0.025, p***=0.004, p<0.04) (Table 3 and Figure 5).
| VAS | RMDS | TAMPA | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Weeks | Gp.A | Gr.B | P Value | Gp.B | Gp.A | P value | Gp.A | Gp. B | P value |
| W0 | 7.53 ± 1.64 | 7.69 ± 1.53 | 48.56 ± 10.47 | 51.34 ± 11.43 | 47.56 ± 4.43 |
49.20 ± 4.78 |
|||
| W2 | 4.94± 1.36 | 4.25 ± 1.73 | P**<0.05 | 39.27 ± 10.35 | 36.87 ± 8.72 | P**<0.05 | 43.92 ± | 41.74 ± 5.07 |
P**<0.05 |
| W4 | 2.47 ± 1.42 | 1.73 ± 1.54 | P**<0.05 | 26.27 ± 9.44 | 19.95 ± 9.37 | P***<0.05 | 39.22 ± 4.85 | 34.88 ± 4.89 |
P***<0.05 |
Table 3: Showing the within group comparison for VAS, RM Disability Scores, TAMPA for 0,2 and 4th week after intervention.
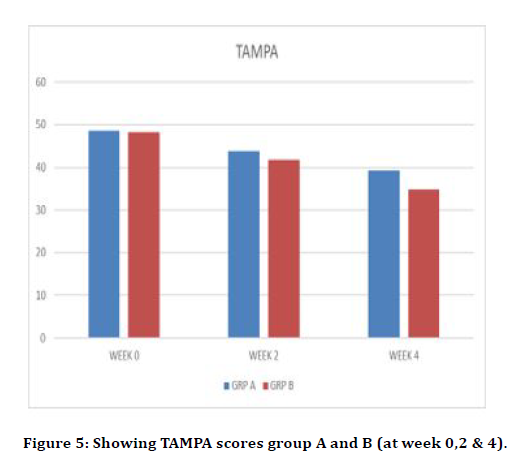
Figure 5. Showing TAMPA scores group A and B (at week 0,2 & 4).
Discussion
Our results demonstrated that Kinesiotaping along with lumbar stabilization exercises help in alleviating the symptoms of WRLBP better than the exercises alone. The findings were found to statistically significant as along with the subjective indexes of VAS, RM Disability Index and TAMPA Kinesiophobia scores, the range of motion especially forward flexion and side rotations of the trunk.
WRLBP is a type of pain having its origin from the musculoskeletal structures of the back and is mechanical in nature and are associated (major cause been repetiv with variation in clinical sign are observed depending upon the type of activities one is performing. It can be represented in various forms such as pain, muscle tension, stiffness, muscle heaviness likely to be located below the costal surface upto or over the gluteal folds inferiorly [31].
Though scanty but the previous published research in KSA regarding Kinesiotaping were focused on the general population. Kachanathu et al. [18] compared the effect of Kinesiotaping with traditional physical therapy treatment among the general WRLBP patients in Cairo. Likewise, another study conducted by Al- Shareef and Omar also conducted the study upon general patient population with treatment intervention been given for 2 weeks. Moreover, the study compared the effect of Kinesiotaping with placebo [19]. Similarly, another study recently published by Alghamdi and Shakwi [20] studied the effects of Kinesiotaping on balance control and functional performance in athletes with chronic ankle instability patients. It is probably for the first time, as far our knowledge goes, a study on healthcare professionals, with physiotherapists and nurses in focus has been conducted within the Kingdom.
Literature review states that among the various healthcare professionals, work related LBP is very very common, which may range from sometimes moderate to severe in character [31]. Physiotherapists and Nurses are most prone for WRLBP with incidences ranging from 35.6% to 67.6% respectively in KSA [32,33]. Being one of the formidable workforces of the healthcare system around the globe, addressing this concern is of extreme importance. Therefore, the focus of our study was to measure the effectiveness of novel treatment modality among the healthcare professionals.
Another interesting difference was that the earlier studies used mostly Kinesiotaping at around the lumbar area only. This is probably for the first time any research has been conducted in the kingdom where thoracolumbar fascial kinesiotaping has been performed. Some of the earlier studies were conducted by both Kachanathu et al. [18] and later by Alghamdi et al. [19] who used KT around the lumbar region only. However, in the current study, KT taping that was done upon patients was extended from the thoracic region below the costal margins upto gluteal folds. There were two important rationales behind using this technique as a treatment modality for the workrelated LBP patients. First reason being Nurses and Physiotherapists are prone to excessive wear and tear because of the nature of their jobs which requires lot of lifting, patient handling and other strenuous activities [32,34,35]. Literature review on biomechanical studies suggest that the continuous strain at the lumbar region adversely affect the other areas including the upper back (spillover effect) thereby causing pain, restricting movement as well as poor functional outcome [36]. But actually, are they better than lumbar taping, is beyond the scope of the present study?
We aimed to evaluate the use of Kinesiotaping (KT) along with conventional physiotherapy exercise treatment among healthcare professionals suffering from WRLBP and found them to be quite effective as compared to the just conventional exercise therapy suggested to the patienrt. The findings of our study find support from the earlier conducted studies where KT has been proven effective in WRLBP [17,36,37].
Secondly, the application of thoracolumbar Kinesiotaping covers a and wider area and thereby thought to bring better therapeutic effect given the nature of job the physiotherapists and nurses had to handle [17,32,37-39].
Regarding the mechanism of action it has been postulated that since the nature of this tape which was highly stretchable (reported to be almost 120- 140% of its original length) but for all practical purposes, the founder of Kinesiotaping, Dr. Kase has recommended to apply stretching the tape between 25-50% [17]. The tape when applied to the chronically weak muscles, especially from the muscle origin to insertion facilitates muscle action [16,40]. Taking cue from the explanation, it can postulate that thoracolumbar fascia which is like a blend of sheet like fibrous membrane covering the muscles of torso as well as sacral region paraspinally, is an especially important structure of the myofascial system and plays an eminent role in maintaining posture, transferring of load as well as in respiration [41-43]. Sitting long hours, overloading of the back muscles with continuous strenuous activities has been found to be associated with altered pattern of superficial trunk muscles activation, which in a long run because of stress, poor posture, unhealthy lifestyle, lack of physical activity, prolonged unaccustomed or strenuous activity etc. [37,44-47].
Therefore, application of Kinesio taping at the affected structure along the line of the paraspinal muscles (thoracolumbar fascia) by means of applying pressure as well as stretching might stimulate the cutaneous mechanoreceptors, causing increased proprioceptive stimuli and thereby activating the paraspinal muscles by causing increased recruitment of the motor units, thereby correcting the postural pathway [48,49].The second mechanism of action might be because of the pain gate pathway, explained by Melzack & Wall pain gate pathway [50]. Here, the taping technique might have stimulated the large diameter afferent fibers mitigating the nociceptive pathway and thereby suppressing pain [37]. Thus, KT might influences sensorimotor function causing change in muscle tone causing stimulation of mechanoreceptors resulting in reflexive activation of motor unit in the same muscle that was the source of the neural stimulus, causing movement enhancement [19]. Therefore, the improvements measured in pain and range of motion in our study can be viewed within the contextual framework of such an explanation.
With reference to the improvements measured in Functional Index and Tampa Kinesiophobia scores it can be correlated to the vicious cycle of inflammation where it has been stated that injury/alteration may cause pain which leads to the amplification of the nociceptive stimulus which enhances pain thereby restricting movement and enhancing further perception of pain, which might cause fear of movement. Some of the studies published recently reported that cognitive model of kinesiophobia originally proposed causes individuals with musculoskeletal pain develop chronic pain syndrome which further reinforces thought and epsouses fear of pain, or more specifically, fear that physical activities may cause pain and/or injury recurrence [51-53]. This vicious feedback might be responsible for disruption of the functional indexes as measured by RM Disability Score in our study.
It is therefore postulated that Kinesiotaping seems to alter all these phenomena by breaking the pain–inflammation–pain–restriction of movement–pain cycle along with providing support and to the weak muscles. The proven benefits of core stabilization exercise (CSE) for the WRLBP patients have been established earlier in large number of studies, where it has been postulated that CSE tend to enhance activation of local trunk muscles, thereby improving coordination which may lead to stability of the lumbar segments, reducing spinal overload [45,54,55]. Usage of different exercises such as lunge, standing forward bend, kneeling forward bend, extended side stretch, warrior posture, standing lateral posture, kneeling lateral posture and chair posture that were incorporated in our study as a control group tend to facilitate cocontraction which might cause improvement in joint reposition sense thereby improving all the clinical outcomes undertaken in our study. The addition of Kinesio taping along with core stabilization exercises in the experimental group might help to develop specific motor control by means of kinesthetic restoration and enhancing thoraco-lumbo-pelvic joint position sense causing improvements in patients of WRLBP.
The study had certain limitations in terms of small sample size and taking single gender (males) only for the study. The inability to blind participants and therapists was another limitation of this study. The other limitation been the duration of the study which was short (only a month) and no follow up could be done to assess the sustained or the long-term effects of kinesio taping. Similarly, different age group analysis or effect of pain duration on therapeutic parameters were not done. Future research could be conducted to measure the effects of different techniques of kinesiotaping on WRLBP or by using more objective parameters such as EMG to support our hypothesis.
Conclusion
Therefore, it is concluded that kinesiotaping is an important adjunct to core stabilization exercises for treating WRLBP among work related back pain problems. The usage may enhance early recovery and help the healthcare professionals to adapt better to their working environments.
Acknowledgements
The authors are grateful to the Deanship of Scientific Research, AlMajmaah University for funding through Vice Deanship of Scientific Research Chairs via ref. no. RGP-2019-35.
Conflict of Interests
None.
References
- Hartvigsen J, Hancock MJ, Kongsted A,et al. What low back pain is and why we need to pay attention. Lancet 2018; 391:2356-2367.
- Hoy DG, Smith E, Cross M, et al. Reflecting on the global burden of musculoskeletal conditions: lessons learnt from the global burden of disease 2010 study and the next steps forward. Ann Rheumat Dis 2015; 74:4-7.
- Jackson T, Thomas S, Stabile V, et al. Chronic pain without clear etiology in low-and middle-income countries: A narrative review. Anesthesia Analgesia 2016; 122:2028-2039.
- Kim LH, Vail D, Azad TD, et al. Expenditures and health care utilization among adults with newly diagnosed low back and lower extremity pain. JAMA 2019; 2:e193676.
- Ibrahim MI, Zubair IU, Yaacob NM, et al. Low back pain and its associated factors among nurses in public hospitals of Penang, Malaysia. Int J Environ Res Public Health 2019; 16:4254.
- Boukerma Z, Behlouli AL, Reggad M. Epidemiology of low back pain among nurses of the hospital of Sétif (Algeria). Occup Environ Med 2014; 71:A113.
- Shishira KB, Pavana. Prevalence of low back pain among physiotherapy interns and post graduate students in Bangalore. Int J Physical Educ Sports Health 2018; 5:171-177.
- Gaowgzeh RA. Low back pain among nursing professionals in Jeddah, Saudi Arabia: Prevalence and risk factors. J Back Musculoskelet Rehab 2019; 32:555-560.
- Homaid MB, Abdelmoety D, Alshareef W, et al. Prevalence and risk factors of low back pain among operation room staff at a tertiary care center, Makkah, Saudi Arabia: A cross-sectional study. Ann Occup Environ Med 2016; 28:1-8.
- Aldera MA, Alexander CM, McGregor AH. Prevalence and incidence of low back pain in the kingdom of saudi arabia: A systematic review. J Epidemiol Global Health 2020; 10:269-75.
- Rajfur J, Pasternok M, Rajfur K, et al. Efficacy of selected electrical therapies on chronic low back pain: a comparative clinical pilot study. Medical science monitor. Int Med J Exp Clin Res 2017; 23:85.
- Hidalgo B, Detrembleur C, Hall T, ety al. The efficacy of manual therapy and exercise for different stages of non-specific low back pain: An update of systematic reviews. J Manual Manipulative Therapy 2014; 22:59-74.
- Abbott A, Schröder K, Enthoven P, et al. Effectiveness of implementing a best practice primary healthcare model for low back pain (BetterBack) compared with current routine care in the Swedish context: an internal pilot study informed protocol for an effectiveness-implementation hybrid type 2 trial. BMJ Open 2018; 8.
- Navid MS, Lelic D, Niazi IK, et al. The effects of chiropractic spinal manipulation on central processing of tonic pain-a pilot study using standardized low-resolution brain electromagnetic tomography (sLORETA). Scientific Reports 2019; 9:1-2.
- Trobec K, Peršolja M. Efficacy of kinesio taping in reducing low back pain: A comprehensive review. J Health Sci 2017; 7:1-8.
- Kase K. Clinical therapeutic applications of the kinesio taping method. 2nd Edn. Kinesio Taping Association, New York 2003.
- Taylor RL, Brown T, O'Brien L. Using and prescribing kinesiotape as a treatment modality for musculoskeletal disorders. Int J Therapy Rehab 2015; 22:408-409.
- Kachanathu SJ, Alenazi AM, Seif HE, et al. Comparison between Kinesio taping and a traditional physical therapy program in treatment of nonspecific low back pain. J Phy Therapy Sci 2014; 26:1185-1188.
- Al-Shareef AT, Omar MT, Ibrahim AH. Effect of kinesio taping on pain and functional disability in chronic nonspecific low back pain. Spine 2016; 41:e821-8.
- Alghamdi A, Shawki M. The effect of kinesio taping on balance control and functional performance in athletes with chronic ankle instability. MOJ Orthop Rheumatol 2018; 10:114-20.
- Chen HM, Wang HH, Chen CH, et al. Effectiveness of a stretching exercise program on low back pain and exercise self-efficacy among nurses in Taiwan: A randomized clinical trial. Pain Management Nurs 2014; 15:283-91.
- Nachemson AL, Jonsson E. Neck and back pain: The scientific evidence of causes, diagnosis and treatment. 4th Edn. Philadelphia: Lippincott Williams & Wilkins 2000; 339–354.
- Hayden JA, van Tulder MV, Malmivaara A, et al. Exercise therapy for treatment of non-specific low back pain. Cochrane Database Syst Rev 2005; 3:CD000335.
- Costa LO, Maher CG, Latimer J, et al. Motor control exercise for chronic low back pain: a randomized placebo-controlled trial. Physical Therap 2009; 89:1275-86.
- Downie WW, Leatham PA, Rhind VM, et al. Studies with pain rating scales. Ann Rheumat Dis 1978; 37:378-81.
- Roland M, Fairbank J. The roland–morris disability questionnaire and the oswestry disability questionnaire. Spine 2000; 25:3115-24.
- Malik K, Sahay P, Saha S, et al. Normative values of modified-modified schober test in measuring lumbar flexion and extension: A cross-sectional study. Int J Health Sci Res 2016; 6:177-187.
- Comachio J, Magalhães MO, Marques AP. A cross-sectional study of associations between kinesiophobia, pain, disability, and quality of life in patients with chronic low back pain. Adv Rheumatol 2018; 58.
- Magalhaes MO, França FJ, Burke TN, et al. Efficacy of graded activity versus supervised exercises in patients with chronic non-specific low back pain: Protocol of a randomised controlled trial. BMC Musculoskelet Disorders 2013; 14:1-6.
- Pijinapple H. Handbook of Medical Taping Concept 1. Madrid: Aneid Press 2007.
- Astfalck RG, O'Sullivan PB, Straker LM, et al. A detailed characterisation of pain, disability, physical and psychological features of a small group of adolescents with non-specific chronic low back pain. Manual Therapy 2010; 15:240-247.
- Alghadir A, Zafar H, Iqbal ZA, et al. Work-related low back pain among physical therapists in Riyadh, Saudi Arabia. Workplace Health Safety 2017; 65:337-345.
- Attar SM. Frequency and risk factors of musculoskeletal pain in nurses at a tertiary centre in Jeddah, Saudi Arabia: A cross sectional study. BMC Res Notes 2014; 7:1-6.
- Nordin NA, Leonard JH, Thye NC. Work-related injuries among physiotherapists in public hospitals: A Southeast Asian picture. Clin 2011; 66:373-8.
- Aldera MA, Alexander CM, McGregor AH. Prevalence and incidence of low back pain in the kingdom of saudi arabia: A systematic review. J Epidemiol Global Health 2020; 10:269-75.
- Tu SJ, Woledge RC, Morrissey D. Does ‘Kinesio tape’alter thoracolumbar fascia movement during lumbar flexion? An observational laboratory study. J Bodywork Movement Therapies 2016; 20:898-905.
- Paoloni M, Bernetti A, Fratocchi G, et al. Kinesio taping applied to lumbar muscles influences clinical and electromyographic characteristics in chronic low back pain patients. Eur J Phys Rehabil Med 2011; 47:237-244.
- Castro-Sánchez AM, Lara-Palomo IC, Matarán-Peñarrocha GA, et al. Kinesio taping reduces disability and pain slightly in chronic non-specific low back pain: a randomised trial. J Physiotherap 2012; 58:89-95.
- Kalron A, Bar-Sela S. A systematic review of the effectiveness of kinesio taping--fact or fashion. Eur J Phys Rehabil Med 2013; 49:699-709.
- Ellis RF. The use and treatment efficacy of kinaesthetic taping for musculoskeletal conditions: a systematic review. N Zealand J Physiother 1980; 38:56.
- Brumagne S, Cordo P, Lysens R, et al. The role of paraspinal muscle spindles in lumbosacral position sense in individuals with and without low back pain. Spine 2000; 25:989-994.
- Panjabi MM. Clinical spinal instability and low back pain. J Electromyograp Kinesiol 2003; 13:371-379.
- Willard FH, Vleeming A, Schuenke MD, et al. The thoracolumbar fascia: anatomy, function and clinical considerations. J Anatomy 2012; 221:507-536.
- Dankaerts W, O'Sullivan P, Burnett A, et al. Altered patterns of superficial trunk muscle activation during sitting in nonspecific chronic low back pain patients: Importance of subclassification. Spine 2006; 31:2017-2023.
- Roland MO, Morris RW. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine 1983; 8:141–144.
- Ruhe A, Fejer R, Walker B. Is there a relationship between pain intensity and postural sway in patients with non-specific low back pain?. BMC musculoskelet Disorders 2011; 12:1-8.
- Balagué F, Mannion AF, Pellisé F, et al. Non-specific low back pain. Lancet 2012; 379:482-491.
- Shields CA, Needle AR, Rose WC, et al. Effect of elastic taping on postural control deficits in subjects with healthy ankles, copers, and individuals with functional ankle instability. Foot Ankle Int 2013; 34:1427-1435.
- Nakajima MA, Baldridge C. The effect of kinesio® tape on vertical jump and dynamic postural control. Int J Sports Phys Therapy 2013; 8:393.
- Mendell LM. Constructing and deconstructing the gate theory of pain. Pain 2014; 155:210-216.
- Vlaeyen JW, Kole-Snijders AM, Boeren RG, et al. Fear of movement/(re) injury in chronic low back pain and its relation to behavioral performance. Pain 1995; 62:363-372.
- Silva AN, Martins MR. Pain, kinesiophobia and quality of life of low back pain patients. Revista Dor 2014; 15:117-120.
- Ishak NA, Zahari Z, Justine M. Kinesiophobia, pain, muscle functions, and functional performances among older persons with low back pain. Pain Res Treatment 2017; 2017.
- Boucher JA, Preuss R, Henry SM, et al. The effects of an 8-week stabilization exercise program on lumbar movement sense in patients with low back pain. BMC Musculoskelet Disorders 2016; 17:1-8.
- Puntumetakul R, Chalermsan R, Hlaing SS, et al. The effect of core stabilization exercise on lumbar joint position sense in patients with subacute non-specific low back pain: A randomized controlled trial. J Phys Therapy Sci 2018; 30:1390-1395.
Author Info
Mohammad Miraj1*, Mazen AlQahtani1, Msaad AlZhrani1, Ahmad Alanazi1, Zafar Hasan2 and Tanuj Garg3
1Department of Physiotherapy, College of Applied Medical Sciences, AlMajmaah University, AlMajmaah, Saudi Arabia2Saudi Arabia
3Department of Research, College of Nursing, King saud university, Saudi Arabia
4Department of Health Sciences, Athar Institute of Health and Management Studies, New Delhi, India
Citation: Mohammad Miraj, Mazen AlQahtani, Msaad AlZahrani, Ahmad Alanazi, Zafar Hasan, Tanuj Garg, Efficacy of Kinesio Taping in attenuating Work-Related Low Back Pain among Physiotherapy and Nursing Professionals, J Res Med Dent Sci, 2021, 9 (4): 415-424.
Received: 24-Mar-2021 Accepted: 16-Apr-2021
