Research - (2023) Volume 11, Issue 1
Effect of Topically Applied Vancomycin Powder in the Occurrence of Dry Socket after Surgical Removal of Impacted Mandibular Third Molar.
Hamid Ibrahim Mohammed1* and Rsul Natq Al-Khafaji2
*Correspondence: Hamid Ibrahim Mohammed, Department of Oral and Maxillofacial surgery, College of Dentistry, Iraq, Email:
Abstract
The major complication that follows tooth extraction is dry socket which is also referred to as fibrinolytic or alveolar osteitis, which is an acute inflammation of the alveolar bone that characterized by severe throbbing pain, empty socket with exposed wall due to absence or break down of blood clot with gingival swelling and tenderness. Many methods had been employed in the treatment of alveolar osteitis; one of them was topical use of antimicrobial agent such as topical antibiotic which is used in the prevention and treatment such as metronidazole, clindamycin and tetracycline. The aim of this study is to identify the effect topically applied Vancomycin powder in the occurrence of dry socket after surgical removal of impacted third molar, 80 patients was involved in this study was divided in tow groups (control and study), dry socket occurred in both group (9 in control and 11 in study) with no significant difference (P value=0.12), the study found high significant relation between the occurrence of dry socket with severity of impaction and increasing age (P value=0.000).
Keywords
Dry socket, Vancomycin, Impaction
Introduction
In 1896 the, dry socket was firstly described by Crawford [1]. Dry socket is an inflammation of the alveolar bone that limited to the lamina dura which occurs when the blood clot fails to form or is lost from the socket [2]. It is considered the most common complications that follows the tooth extraction [3] and it is one of the most studied complications in dentistry [4].The condition is also known as localized osteitis, alveolitis sicca dolorosa or fibrinolytic osteitis [5]. The incidence of dry socket is about 3% and reaches over 30% after surgical removal of impacted third molar [6].
Clinical manifestations include the following: constant, spontaneous radiating pain with inflammation signs around previously extracted socket like swelling gums, hyperemia with empty alveolus or filled with necrotic clot or food debris [7]. Antibiotic treatment involved in the management of dry socket in topical and systemic administration [8]. Lincomycin, clindamycin and tetracycline were used topically, penicillin, metronidazole and erythromycin were used as systemic antibiotics [9]. In many studies the use of topical antibiotic paste was found effective in the management of dry socket, gel form of tetracycline was used as local applied antibiotic, also powder and aqueous solution was found to be effective in the prevention and treatment modality [10].
Many factors are contributing in the incidence of dry socket including; difficult or traumatic extractions, pre-existing infection, tobacco use, female gender and oral contraceptives [11].The main etiological factor in fibrinolytic alveolitis is an increased local fibrinolytic activity which result in premature loss of the blood clot [12].
Plasminogen pathway activation leads to the fibrinolysis that can be accomplished either by physiologic (direct) or non-physiologic [indirect] activator substances, trauma to the alveolar bone cell result in releasing of direct activators while bacteria result in secretion of indirect activator [13].
Contact of the healing epithelium with the exposed bone may be hider by bacterial biofilm, the formation of toxins or antigens may irritate the exposed bone which produces the pain and an unpleasant taste or halitosis [14].
Multiple studies have showed the relation between specific bacteria and disease [15]. Bacterial infection associated with prolonged and difficult surgical procedures are often implicated in etiology of alveolar osteitis [9].
The presence of fibrinolytic microorganisms like Treponema denticola, Staphylococcus spp., Streptococcus spp., Prevotella spp. and Bacteroides spp., may induce a non-physiologic blood clot lysis that involved in alveolar osteitis [16].
Reducing the incidence of infection at surgical site by administration of local antibiotics is gaining popularity among many surgeons. Cardiac surgeons in 1989 were first used vancomycin topically by applying it after sternotomy [17]. Recently, topical use of vancomycin has been extended to the cranial surgery and vancomycin is a logical choice for a topical antibiotic in cranial wounds [18].
Vancomycin has the ability to kill penicillin resistant Staphylococcus aureus,it is highly effective bactericidal agent against most gram-positive bacteria and highly efficacious against S. aureus [19].
The selection of vancomycin as topical antibiotic because of its cost effectiveness, broad coverage effect against organisms such as MRSA and easy to use, vancomycin powder that is used topically is not readily absorbed by the systemic circulation, but it stays in the surgical site and prevent infection by locally action [20].
Methodology
The study was done in oral and maxillofacial department -College of Dentistry – Kerbala University –Iraq during 2021 and 2022.
The exclusion criteria involved the following: patients had comorbid condition like diabetes mellitus, steroid therapy, chemotherapy, patients with osteoporosis, pregnant, pericoronitis, ingestion any antibiotic at least 4 days before surgery, history of allergy and patient who could not complete the session of follow up.
Ethical approval was obtained by scientific committee in oral and maxillofacial surgery department in College of Dentistry – University of Kerbala. Informed consent was obtained from all patients.
All patients were examined by maxillofacial surgeon and were sent for radiographic examination either by OPG or CBCT for determining and classification of the impaction as well as for helping in detection of difficulty of surgical procedure.
Impaction classification
Mandibular third molars impaction was classified according to Archer (1975) and Kruger (1984),which is depending on the angulation of the long axis of the impacted third molar with respect to the long axis of the adjacent second molar; Pell and Gregory classification (classes 1, 2, and 3) which is depending on the relationship of the crown of the impacted tooth to the anterior border of the ramus of mandible and Pell and Gregory classification (classes A, B and C), which is depending on the relation of occlusal surface of impacted tooth to the level of occlusal plane of second molar . Pederson scale was used to determine the difficulty of surgery [21].
All patients underwent the surgery under local anesthesia (2 % lidocaine with 1/100000 epinephrine) by inferior alveolar neve block and long buccal nerve block. Triangular or envelop flap according to the impaction type was done then mucoperiosteal flap was reflected. Osteotomy and tooth sectioning were used according to the need. After tooth extraction, the alveolar socket cleaningnd smoothening of the bone edges were done. The vancomycin was used as powder form which exists as vancomycin hydrochloride, 1 g of powder was used and applied directly in the alveolar socket after cleaning and dryness were obtained. Then the flap was sutured with 3/0 silk suture by interrupted technique. Patients were informed to revisit after 48 hours for follow up and examination the surgical site.
The diagnosis of dry socket was depended on the classical signs and symptoms which included: absence or necrotic of the blood clot, exposed walls of the alveolar socket, marginal inflammation and foul smell. Symptoms included sever pain that radiated to the ear, eye or temple. The X-ray was used to rule out the presence of bone or tooth fragments.
Results
There were 80 patients participated in this study (40 patients for each control and study group. Age groups were divided in to three groups (Tables 1-3).
| Age groups | Control group | Study group | ||
|---|---|---|---|---|
| Male | Female | Male | Female | |
| 18-23 years | 10 | 15 | 13 | 11 |
| 24-29 years | 7 | 3 | 5 | 4 |
| 30-35 years | 4 | 1 | 2 | 5 |
| Total | 21 | 19 | 20 | 20 |
Table 1: Age groups and gender distribution.
| Control group | |||||||
|---|---|---|---|---|---|---|---|
| Archer and Kruger | No. | Pell and Gregory | Pell and Gregory | ||||
| 1 | 2 | 3 | A | B | C | ||
| Mesioangular | 18 | 10 | 5 | 3 | 5 | 9 | 4 |
| Vertical | 10 | 4 | 4 | 2 | 3 | 5 | 1 |
| Horizontal | 7 | 2 | 4 | 1 | 4 | 3 | 0 |
| Distoangular | 5 | 0 | 4 | 1 | 1 | 3 | 1 |
| Study group | |||||||
| Archer and Kruger | No. | Pell and Gregory | Pell and Gregory | ||||
| 1 | 2 | 3 | A | B | C | ||
| Mesioangular | 17 | 8 | 7 | 2 | 7 | 6 | 4 |
| Vertical | 8 | 5 | 2 | 1 | 4 | 4 | 0 |
| Horizontal | 9 | 5 | 3 | 1 | 3 | 5 | 1 |
| Distoangular | 6 | 0 | 3 | 3 | 1 | 4 | 1 |
Table 2: Impaction classification.
| Control group | ||||
|---|---|---|---|---|
| Type | No. | Pederson scale | ||
| Easy | Moderate | Difficult | ||
| Mesioangular | 18 | 10 | 5 | 3 |
| Vertical | 10 | - | 4 | 6 |
| Horizontal | 7 | 2 | 4 | 1 |
| Distoangular | 5 | - | - | 5 |
| Total | 12 | 13 | 15 | |
| Study group | ||||
| Type | No. | Pederson scale | ||
| Easy | Moderate | Difficult | ||
| Mesioangular | 17 | 7 | 8 | 2 |
| Vertical | 8 | - | 5 | 3 |
| Horizontal | 9 | - | 8 | 1 |
| Distoangular | 6 | - | - | 6 |
| Total | 7 | 21 | 12 | |
Table 3: Pederson scale.
Occurrence of dry socket
Dry socket was diagnosed in 20 patients, 11 patients in control group and 9 patients in experimental group. From all patients with dry socket there were 13 females and 7 males. Statically there is no difference in the occurrence of the dry socket between male and female (P value=0.76), also there was no difference in the use of vancomycin between study and control group (P value =0.12), but statically highly significant difference was shown in relation to the age group (30-35) and occurrence of dry socket verses with the severity of impaction (Pvalue=0.000) (Table 4, Figures 1 and 2).
| Control group | Dry socket | Gender | Pederson scale of severity | Age group in years | |||||
|---|---|---|---|---|---|---|---|---|---|
| 11 | Male | female | Easy | Moderate | Difficult | 18-23 | 24-29 | 30-35 | |
| 4 | 7 | 1 | 1 | 9 | 4 | 3 | 4 | ||
| Study group | Dry socket | Gender | Pederson scale of severity | Age group in years | |||||
| 9 | Male | female | Easy | Moderate | Difficult | 18-23 | 24-29 | 30-35 | |
| 3 | 6 | - | - | 9 | 2 | 2 | 5 | ||
Table 4: relation between the occurrence of dry socket with age, gender and severity of impaction.
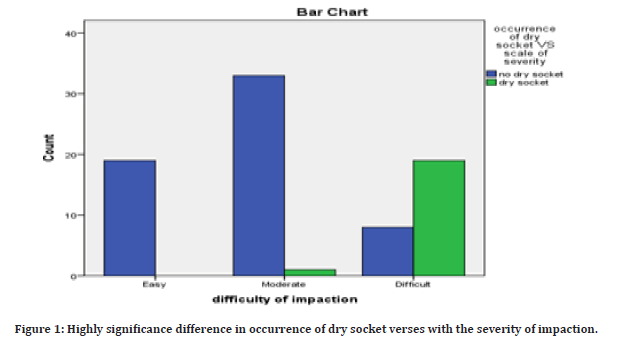
Figure 1: Highly significance difference in occurrence of dry socket verses with the severity of impaction.
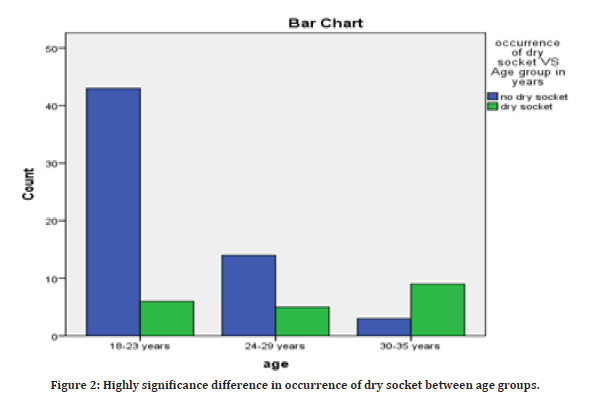
Figure 2: Highly significance difference in occurrence of dry socket between age groups.
Discussion
The occurrence of the dry socket had been showed by this study in 25% from all patients that compatible with other studies, the alveolar ostietis occurs in about 0.5– 5% of routine dental extractions, and in about 25–30% in mandibular third molar extraction [22].
In this study, dry socket was mainly occurred in female patients (13 females [65%) and 7 males (35%) and F/M ratio was 1.85:1], although it was not statically significant, the majority of females (10 patients were married and 7 patients of them were with history contraceptive drugs, another 3 female patients had poor oral hygiene without history of contraceptive drugs and 3 females with good oral hygiene and without history of contraceptive, in male patients of them were smokers, in spite of the contraceptive drugs, smoking and bad oral hygiene might be considered as risk factors, dry socket had been occurred in patients without these predisposing factors. In this study strong relationship had been showed between the incidence of fibrinolytic alveolitis and severity of the impaction with prolong time of surgery, high significant difference had been shown in the occurrence of dry socket in severe cases, although 2 cases of dry socket were reported in patients with mild and moderate impaction according to Pederson scale and might be related to the failure of patients to follow the post extraction instructions, which means the etiology of dry socket still subject to much debate. Several factors have been reported to be responsible for the occurrence of dry socket; which include difficult, traumatic and prolonged extraction, smoking, postoperative infection at surgical site, using of oral contraceptives drugs, and failure to obey post extraction instructions [9,23]. In the dental literature, there is uncertainty about the causes of the dry socket, in spite of some factors such as oral contraceptive, smoking and fibrinolytic activity presence in the post extraction socket which are related with increase in the incidence of dry socket, mechanism that definitively explains the pathogenesis of dry socket remains elusive [9].
The study found, statically highly significant [Pvalue=0.000] relation between increase in the occurrence of dry socket with increase in the age of the patients, we explained that was due to the changes in the bone density and vascularity with aging. Decrease in the bone elasticity and increase in the bone density made the surgical extraction more difficult and prolong surgery time. Porosity of the bone increases as aging increases while the toughness of the bone and fibers decreases, the porosity of the bone increases through micro factors, these micro factor allows a smooth floor for channels and the flow of the blood flow and prevents blood clot from occurring [24]. Hypo vascularity due to the density of bone is considered as main etiological factor that implicated in the occurrence of dry socket [25].
Multiple methods have been used in the treatment of dry socket, one of them was topical applied of antibiotic. In the alveolar ostetitis, pathological bacteria play critical role by fibrinolytic enzymatic activities. Bacteria have been suggested to play a role in alveolar osteitis, the fact that the bacteria share most of the risk factors of postoperative infections supports this suggestion [26].
Because of alveolar oseitis is an infection that provoked by bacteria, so that assessment of prevention and treatment guidelines and prescription of antibiotic and antiseptic might be essential, several clinical trials have shown that both topical and systemic antibiotics and antiseptics significantly reduce the occurrence of alveolar oseitis [27].
Different preventive measures have shown efficacy in the prevention of dry socket, these include local application of tetracycline, lincomycin gel foam, clindamycin and topical using of pencilline [28,29].
In this study we used vancomycin as topically applied powder after surgical removal of impacted third molar. The application of topical powdered antibiotic is the main aim to obtain substantially long lasting and higher concentrations of antibiotic at surgical site and prevent the systemic circulation to the toxic drugs levels [20].
The topical using of vancomycin in orthopedic, spine and cranial surgery also in recent year an increase in MRSA infection and efficacy of this antibiotic against gram positive bacteria encouraged us to used it in trial to know it effect in the prevention of dry socket after surgical removal of impacted third molar. Topical application of vancomycin was widely used in orthopedic and neurosurgery for prevention of surgical site infection. Recently, topical use of vancomycin has been extended to the cranial surgery, vancomycin is a logical choice for a topical antibiotic in cranial wounds [19].
The study found there was no effect of topically used of vancomycin powder in the occurrence of dry socket statistically was not significant [P value=0.12], that may be explained by that different types of microorganisms that participated in the occurrence of dry socket like Treponema dentiloca, Bacteriod spp. and Prevotella spp., which are considered gram negative anaerobic bacteria and not effected by vancomycin. The presence of fibrinolytic microorganisms such as Treponema denticola, Staphylococcus spp., Streptococcus spp., PeptoStreptococcus spp, Prevotella spp. and Bacteroides spp., may induce a non-physiologic blood clot lysis, and may be another etiological factor that involved in alveolar osteitis [16].
Conclusion
Dry socket occurrence was common after third molar surgery, severity of impaction, patient age and female gender were the main factors determined the occurrence. Topically used of vancomycin powder was not effective in the occurrence of dry socket.
References
- Rood JP, Murgatroyd J. Metronidazole in the prevention of ‘dry socket’. Br J Oral Surg 1979; 17:62-70.
- Jesudasan JS, Wahab PA, Sekhar MM. Effectiveness of 0.2% chlorhexidine gel and a eugenol-based paste on postoperative alveolar osteitis in patients having third molars extracted: A randomised controlled clinical trial. Br J Oral Maxillofac Surg 2015; 53:826-830.
- Burgoyne CC, Giglio JA, Reese SE, et al. The efficacy of a topical anesthetic gel in the relief of pain associated with localized alveolar osteitis. J Oral Maxillofac Surg 2010; 68:144-148.
- Cardoso CL, Rodrigues MTV, Ferreira O, et al. Clinical concepts of dry socket. J Oral Maxillofac Surg 2010; 68:1922-1932.
- Blum IR. Contemporary views on dry socket (alveolar osteitis): A clinical appraisal of standardization, aetiopathogenesis and management: A critical review. Int J Oral Maxillofac Surg 2002; 31:309-317.
- Bowe DC, Rogers S, Stassen FA. The management of dry socket/alveolar osteitis. J Dent Assoc 2011; 57:305-310.
- Mamoun J. Dry socket etiology, diagnosis, and clinical treatment techniques. J Korean Assoc Oral Maxillofac Surg 2018; 44:52-58.
- Noroozi AR, Philbert RF. Modern concepts in understanding and management of the “dry socket” syndrome: Comprehensive review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont 2009; 107:30-35.
- Blum IR. Contemporary views on dry socket (alveolar osteitis): A clinical appraisal of standardization, aetiopathogenesis and management: A critical review. Int J Oral Maxillofac Surg 2002; 31:309-317.
- Sorensen DC, Preisch JW. The effect of tetracycline on the incidence of postextraction alveolar osteitis. J Oral Maxillofac Surg 1987; 45:1029-1033.
- Nusair YM, Goussous ZM. Quantifying the healing of dry socket using a clinical volumetric method. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101:e89-95.
- Noroozi A-R, Philbert RF. Modern concepts in understanding and management of the “dry socket” syndrome: Comprehensive review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009; 107:30-35.
- Kolokythas A, Olech E, Miloro M. Alveolar osteitis: A comprehensive review of concepts and controversies. Int J Dent 2010; 2010:249073.
- Tarakji B, Saleh LA, Umair A, et al. Systemic review of dry socket: Aetiology, treatment and prevention. J Clin Diagn Res 2015; 9:10-13.
- Shen LH, Xiao E, Wang EB, et al. High-throughput sequencing analysis of microbial profiles in the dry socket. J Oral Maxillofac Surg 2019; 77:1548-1556.
- Riba-Terés N, Jorba-García A, Toledano-Serrabona J, et al. Microbiota of alveolar osteitis after permanent tooth extractions: A systematic review. J Stomatol Oral Maxillofac Surg 2021; 122:173-181.
- Vander Salm TJ, Okike ON, Pasque MK, et al. Reduction of sternal infection by application of topical vancomycin. J Thorac Cardiovasc Surg 1989; 98:618–622.
- Ghobrial GM, Thakkar V, Singhal S, et al. Efficacy of intraoperative vancomycin powder use in intrathecal baclofen pump implantation procedures: Single institutional series in a high risk population. J Clin Neurosci 2014; 21:1786–1789.
- Levinson W. Review of medical microbiology and immunology. 13th Ed. New York: The McGraw-Hill Companies; 2012.
- Singh G, Passi D, Daga D, et al. Study of antibiotic efficacy of topical vancomycin powder in treatment of infected mandibular fractures and soft tissue surgical site infections. J Family Med Prim Care 2019; 8:3340-3344.
- Pederson GW. Oral Surgery. Philadelphia: WB Saunders, 1988.
- Khalifah MA. Risk factors, etiology and treatment modalities for localized alveolar ischemia (The so-called alveolar osteitis): A comprehensive critical review. Surgery 2018; 7:32.
- Betts NJ, Makowski G, Yee-Hsiung S, et al. Evaluation of topical viscous 2% lidocaine jelly as an adjunct during the management of alveolar osteitis. J Oral Maxillofac Surg 1995; 53:1140-11444.
- Xu JL, Xia R. Efficacy of plasma rich in growth factor used for dry socket management: A systematic review. Med Oral Pathol 2019; 24:e704.
- Kruger G. Textbook of oral surgery. 3rd Ed. St Louis, MO, CV Mosby, 1968; 128.
- Cho H, David MC, Lynham AJ, et al. Effectiveness of irrigation with chlorhexidine after removal of mandibular third molars: A randomised controlled trial. Br J Oral Maxillofac Surg 2018; 56:54-59.
- Ren YF, Malmstrom HS. Effectiveness of antibiotic prophylaxis in third molar surgery: A meta-analysis of randomized controlled clinical trials. J Oral Maxillofac Surg 2007; 65:1909-1921.
- Goldman DR, Kilgore DS, Panzer JD, et al. Prevention of dry socket by local application of lincomycin in Gelfoam. Oral Surg Oral Med Oral Pathol 1973; 35:472-474.
- MacGregor AJ, Addy A. Value of penicillin in the prevention of pain, swelling and trismus following the removal of ectopic mandibular third molars. Int J Oral Surg 1980; 9:166-172.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Hamid Ibrahim Mohammed1* and Rsul Natq Al-Khafaji2
1Department of Oral and Maxillofacial surgery, College of Dentistry, Kerbala University, Iraq2Department of Prosthodontic, College of Dentistry, Kerbala University, Iraq
Citation: Hamid Ibrahim Mohammed, Rsul Natq Al-Khafaji, Effect of Topically Applied Vancomycin Powder in the Occurrence of Dry Socket after Surgical Removal of Impacted Third Molar, J Res Med Dent Sci, 2023, 11 (1):33-38.
Received: 12-Dec-2022, Manuscript No. jrmds-22-83139; , Pre QC No. jrmds-22-83139(PQ); Editor assigned: 14-Dec-2022, Pre QC No. jrmds-22-83139(PQ); Reviewed: 29-Dec-2022, QC No. jrmds-22-83139(Q); Revised: 02-Jan-2023, Manuscript No. jrmds-22-83139(R); Published: 09-Jan-2023
