Research Article - (2022) Volume 10, Issue 5
Effect of Resin Infiltrate Modified with Bioactive Glass on Hardness and Color Stability of White Spot Lesions
*Correspondence: Reem Ashraf, Department of Prosthodontic Dentistry, King Salman International University,El Tur, Egypt, Email:
Abstract
Introduction: Resin infiltration is now used in treatment of white spot lesion, the incorporation of bioactive particles in such procedure would favour remineralisation of the defect increasing the surface hardness that might be considered a breakthrough the minimally invasive treatment.Aim: To evaluate the effect of adding nano bioactive glass as a Re-mineralizing agent to ICON resin infiltrate on enamel micro hardness and color change without compromising depth of penetration.
Materials and methods: 20 sound human upper anterior teeth extracted due to grade III mobility were decapitated from their roots, all aspects of the crown were coated with varnish, leaving a 4 mm × 4 mm window and left in demineralizing solution to create demineralized lesions. Afterwards half of ICON resin infiltrate was mixed with 10% of nano bioactive glass dissolved in ethanol, teeth were then divided into two group. Group I: Treated with ICON containing 10% Nanobioactive glass. Group II: Treated with ICON only, the two groups were examined before and after treatments for hardness and color stability after staining.
Results and discussion: There was no significant change in hardness of enamel surface between the two groups and the bioactive glass was able to penetrate through the enamel surface, color stability as well was not compromised by addition of bioactive glass.
Conclusion: Addition of nano bioactive glass to resin infiltrate would not compromise hardening effect of resin or penetration of the lesion or color change.
Keywords
Resin infiltration, Bioactive glass, Color stability, Hardness, Penetration ability
Introduction
White spots of teeth are believed a source of embarrassment to many people especially while smiling. In most of the cases to resolve the problem, drilling of teeth and restoration would be considered, which now in the era of conservatism is no more accepted. In general, white spots involves demineralization process that may eventually create pores, progressive decline in enamel surface hardness and chalky white appearance. They are linked to a large form of etiologies including enamel genetic anomalies, metabolic conditions, exposure to trauma, drugs, and radiation. Post orthodontic brackets may also cause these lesions [1-3]. Treatment of white spot lesions irrespective of their etiology is crucial as these lesions are continuously exposed to plaque accumulation and may trigger caries progression. The esthetic treatment of white lesions in anterior teeth may be a frequent challenge for the dentists seeking conservation of tooth structure, multiple treatment modalities are validated as an efficient therapy including; topical fluoride agents, casein phosphopeptide amorphous phosphate agents and antimicrobial agents. These above mentioned modalities, aimed to arrest caries through enhancement of remineralization process, however, it doesn't manage the esthetic aspect. However, bleaching was also considered in treatment but multiple side effects were reported including tooth sensitivity, decrease in enamel microhardness and particular change within the shade of both white spot lesion and normal tooth surface [4].
Micro-abrasion is another alternative technique employed in treatment of white spot lesions but considered a comparatively invasive technique. It involves application of acid and pumice within the paste form (an abrasive and erosive materials) to the affected and normal enamel surfaces, which removes about 100 µ of the enamel and the polished enamel doesn't have the everyday enamel surface appearance as there is no interprismatic space in micro abraded enamel [5]. Moreover, resin infiltration is another minimal invasive approach. This breakthrough micro-invasive technology fills and reinforces demineralized enamel without drilling or anaesthesia by forming a barrier through surface tension instead of lesion masking. ICON resin infiltrate is a light-cured resin of low viscosity. It is used to fill the lesion pores after acid etching of the surface. Acid etching is done by 15% hydrochloric acid gel to expose lesion porosities which facilitates the penetration of ICON via capillary action; Low viscosity of resin improves the penetration into the porous enamel and prevents diffusion of the bacteria.
ICON infiltration is considered a revolutionary treatment modality for treatment of smooth surface and proximal carious lesions as it is quick, simple, and painless procedure. Instead of taking a “wait and see” approach, it can arrest the progress of incipient enamel lesions up to the first third of dentin in one simple procedure, without unnecessary loss of healthy tooth structure [6]. Furthermore, it can restore shade of the white spots as it works on the principle of the light scattering phenomenon. The sound enamel has a refractive index of 1.62, while the porosities of a white spot lesion are usually filled with either a watery or air medium, which have refractive indices of 1.33 and 1, respectively. The whitish appearance of the lesion is contributed to the difference in the refractive indices between the enamel crystals and the medium causing scattering of the light. By application of ICON, the refractive index of micro-porosities becomes 1.46 and the difference between them become negligible. Although, ICON infiltrates the lesion and arrests the progression of white spot lesions. Yet, it lacks the ability to remeneralize this lesion [7]. Incorporation of bioactive glass with its remineralization ability into several materials in the dental field is widely spreading and has proven effectiveness in restorative materials. Bioactive Glass 45S5 (BAG) composed of 45% SiO2, 24.5% Na2O, 24.5% CaO, and 6% P2O5 has been extensively studied regarding the remineralization of white spot lesions [8].
Kim HJ found that when demineralized enamel was treated with different types of BAG, surface microhardness of the enamel tissueincreased. This increase of microhardness was found to be higher in BAG group when compared to the application of other agents [9]. Soares R reported that the recovery rate of microhardness on demineralized enamel surface after treatment with BAG was 28.8%. Apart from assessing microhardness, the mean carious lesion depth in specimens treated with BAG was significantly lower than those of specimens without BAG treatment [10]. Prabhakar assessed the percentage of lesion depth after remineralisation and the experimental group with BAG had the highest percentage of lesion depth in enamel. In addition, Energy Dispersive X-ray spectroscopy (EDX) analysis indicated that Ca/P ratio was higher in the region treated with bioactive glass than in other regions not covered by BAG particles.
Since ICON resin infiltrate can penetrate through the white spot lesion and arrest the progression of caries but still has some concerns regarding its ability to demineralize demineralized lesions. To overcome this limitation this study suggests adding Nano-BAG demineralizing agent to ICON with 10% weight concentration aiming to increase the surface micro-hardness of demineralized enamel, prohibit demineralization and promote remineralisation. The null hypothesis of the study was that the addition of BAG to the resin infiltrate would affect enamel micro hardness, induce color change upon staining and compromise depth of penetration.
Materials And Methods
The total sample size in the two groups (ICON, ICON+10% BAG) was estimated to be 20 and were randomly allocated in two test groups.
Teeth selectionA total of 20 sound human upper anterior teeth extracted due to grade III mobility from patients with age above 50 years old were used in this study after their permission. The extracted teeth were washed by distilled water then cleaned by an ultrasonic scalar to remove hard and soft deposits and then examined to be free of any cracks or caries [11].
Specimens preparationThe crowns were decapitated from their roots under copious air-water coolant spray using a diamond stone with low-speed hand piece below the Cement Enamel Junction (CEJ); afterwards all aspects of the crown were coated with varnish, leaving a 4 mm × 4 mm window to allow the demineralizing solution to affect this window only. The decapitated crowns were then thoroughly rinsed with air water spray, coated with cotton tissues soaked in distilled water and placed in an incubator at 37°C.
Creation of demineralized (caries like lesions)Preparation of demineralizing solution: The demineralizing solution was prepared by mixing 2.2 mM calcium chloride, 2.2 mM monopotassium phosphate and 1 M potassium hydroxide. Then adding 0.05 mM acetic acid to provide acidic medium with pH 4.4. This prepared acidic solution was used to create carious like lesion in the specimens [12].
Specimen’s demineralization: Caries like lesions on the enamel were produced by placing the samples in a demineralizing solution for 4 days in the incubator at temperature 37 degrees. The solution was renewed daily to prevent the accumulation of materials produced by demineralization and the consequent pH change. After removal of samples from the demineralizing solution, samples were washed thoroughly and placed in artificial saliva that was previously prepared (NaCl (2/9 g), CaCl2 (0/12 g), NaH2PO4 (0/13 g), NaF (5 cc) (100 ppm), NaN3 (5 cc) (2% ww)) till time of testing [13-15].
Preparation of modified icon infiltrate with bioactive glassHalf of ICON resin infiltrates “15% Hydrochloric acid (HCl), pyrogenic silicic acid and surface reactive substances tube (22.5 mg) was mixed with 2.25 mg of nano bioactive glass dissolved in ethanol for dilution on an electromagnetic stirrer. The diluted mix was then added to ICON resin in a dark container. To ensure that the particles of nano bioactive glass were properly distributed, the whole mix was left in ultrasonic homogenizer for 6 hours [16].
Specimens groupingIn this study the samples were randomly allocated to one of two groups. Each group contains 10 samples.
Group I: Treated with ICON containing 10% nano-bioactive glass.
Group II: Treated with ICON only.
Application of icon infiltrate to the specimensAt first, rinsing and cleaning of the tooth, then ICON-etch was applied and let sit for two minutes (according to manufacturer instructions). Then, etch was rinsed off with water for 30 seconds, drying with oil-and water-free air, ICON dry was then applied and for 30 seconds. Finally, ICON infiltrate was applied and dispersed with air, let set for 3 mins, then light cured for 40 seconds. Same procedures will be followed in treatment of group II samples using BAG modified ICON. After application of ICON, the samples were incubated in artificial saliva for 7 days and the solution was renewed daily [17].
Testing of samplesHardness test: Surface micro hardness of the specimens was determined using digital display Vickers micro hardness tester with a Vickers diamond indenter and a 20 objective lens. A load of 100 g was applied to the surface of the specimens for 20 seconds. Three indentations, which were equally placed over a circle and not closer than 0.5 mm to the adjacent indentations, were made on the surface of each specimen. The diagonals length of the indentations was measured by built in scaled microscope and Vickers values were converted into micro-hardness values. Micro-hardness was obtained using the following equation: HV=1.854 P/d2 Where, HV is Vickers hardness in Kgf/mm2, P is the load in Kg and d is the length of the diagonals in mm [18].
Color stability measurement: OHIS interpretation. The data analysis was performed using SPSS software (version 23). The chi square test and Pearson correlation was done. The chi square test was used to compare the data and checked for the distributions at 0.05 level of significance for effect of statistical significance. The specimen’s colors were measured using a portable reflective spectrophotometer. The specimens were then immersed in hibiscus solution and incubated at 37°C for 14 days. The aperture size was set to 4 mm and the specimens were exactly aligned with the device. A white background was selected, and measurements were made according to the CIE L*a*b* color space relative to the CIE standard illuminate D65.
Scaning electron microscope: Teeth were sectioned in buccolingual direction then were coated with a layer of gold prior to SEM assessment in a Quick Coater vacuum evaporator to prevent build-up of electrostatic charge. Evaluation of ICON infiltration was done using Field Emission-Scanning Electron Microscope at × 2000 magnification.
Results
Data were explored for normality using Kolmogorov-Smirnov and Shapiro-Wilk tests. Data for the micro-hardness test showed parametric distribution. Independent T-test was used to compare between two groups. The significance level was set at P ≤ 0.05. Statistical analysis was performed with IBM® SPSS® Statistics Version 22 for Windows.
Vickers micro-hardness testNo statistically significant difference was found between the control group (ICON) and the modified ICON group where p=0.65. The highest mean value was recorded for modified ICON group (290.81 Kg/mm2). The micro-hardness test results are presented by Table 1.
Table 1: The Mean, standard deviation, maximum and minimum values of Vickers microhardness test in different groups.
| Variables | Vickers Microhardness (Kg/mm2) | ||||
|---|---|---|---|---|---|
| Mean | SD | Max | Mini | P-value | |
| Control | 288.75 | 16.06 | 318.99 | 269.86 | 0.65 ns |
| Modified ICON | 290.81 | 17.11 | 326.02 | 269.67 | |
Statistical analysis: Data were explored for normality using Kolmogorov-Smirnov tests. Data for the color change showed nonparametric distribution. Results were expressed as median and range and Mann Whitney U-test was used to compare between two groups. The significance level was set at P ≤ 0.05. Results are summarized in Table 2 and Figure 1. As regards ∆L, ICON group recorded a higher median value (-17.97, range -23.97 to -6.20), in comparison to (median -14.27, range -29.10 to -9.67) in ICON+BAG group. The difference between groups was not statistically significant (p=0.691). As regards ∆a, ICON+BAG group recorded a higher median value (2.17, range 0.23 to 7.7), in comparison to (median 1.07, range -5.7 to 4.47) in ICON group. The difference between groups was not statistically significant (p=0.145). As regards ∆b, ICON+BAG group recorded a higher median value (-19.13, range -21.87 to -8.23), in comparison to (median -7.57, range -15.17 to -0.97) in ICON group. The difference between groups was statistically significant (p=0.002). As regards ∆E, ICON+BAG group recorded a higher median value (25.52, range 14.94 to 35.53), in comparison to (median 20.71, range 10.05 to 25.31) in ICON group. The difference between groups was not statistically significant (p=0.122).
Table 2: Median, range, and results of Mann Whitney U test for comparison between groups regarding change in color parameters after immersion in staining solution.
| ICON | ICON+BAG | P value | |||||
|---|---|---|---|---|---|---|---|
| Median | Min | Max | Median | Min | Max | ||
| ∆L | -17.97 | -23.97 | -6.2 | -14.27 | -29.1 | -9.67 | 0.691 ns |
| ∆a | 1.07 | -5.7 | 4.47 | 2.17 | 0.23 | 7.7 | 0.145 ns |
| ∆b | -7.57 | -15.17 | -0.97 | -19.13 | -21.87 | -8.23 | 0.002 |
| ∆E | 20.71 | 10.05 | 25.31 | 25.52 | 14.94 | 35.53 | 0.122 ns |
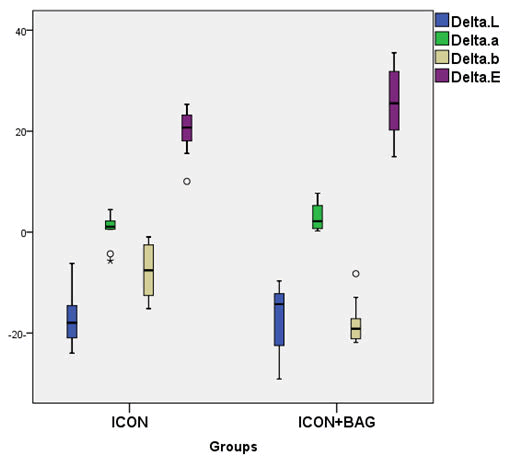
Figure 1:Box plot illustrating median and interquartile range of change in color parameters after immersion in staining solution.
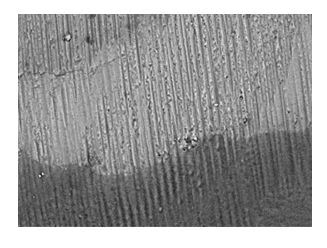
Figure 2:SEM indicating infiltration of icon into the enamel surface.
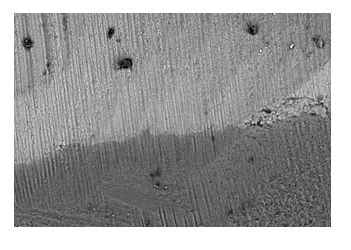
Figure 3:SEM indicating infiltration of modified icon into the enamel surface.
Discussion
Resin infiltration is now widely used in treatment of white spot lesions, where the resin can penetrate spaces and fill the gaps, modification of the resin might be considered, to enable not only filling the space, but also further remineralisation of enamel would be of great benefit. ICON resin infiltrate is mainly composed of TEGDMA which is well known for its low viscosity in comparison to Bis-GMA, this may benefit in better penetration of the resin into the microstructure of the enamel which is the main target of resin infiltration technique for treatment of white spot lesions [19]. Moreover, the use of ICON-dry for 30 seconds (Which contains 99% ethanol) in the application of the ICON infiltrate will remove any excess water and improves penetration ability by decreasing contact angle of enamel surface. Enamel micro-hardness was proven to increase by the use of ICON, Gurdogan in a study on bovine incisors, where values for demineralized enamel had significantly lower micro-hardness than the values of the sound enamel and the demineralized enamel treated by ICON. Moreover, Paris has proven that repeated application of ICON resin improved both micro-hardness and lesion resistance to demineralization [20-22].
Thus, incorporation of resin into the demineralized enamel strengthens the enamel structure and prevents further wear and that is something we would never choose to sacrifice upon ICON application through addition of nano sized bioactive glass. However, regaining the surface hardness of resin infiltrated WSLs similar to sound enamel are doubtful. On the other hand, Despite the proven benefits of ICON as easy accessibility, simplicity, and sufficient outcomes, Shaikh ZA discovered that remineralisation with ICON showed 2.1% decline when compared to the sound enamel samples. In the current study, and after incorporation of nano sized bioactive glass, the hardness test results showed that there was no statistically significant difference between ICON group, and ICON modified with bioactive glass in the two groups (I and II). That means the addition of bioactive glass did not affect the ability of ICON to infiltrate and strengthen the enamel structure. These findings agreed with El Meligy and Nabil AL again. However, more time is required to prove the formation of hydroxyapatite crystals [23].
Moreover, images obtained from SEM imaging indicated that both groups were able to infiltrate into the surface of enamel and that addition of bioactive glass did not compromise fluidity of ICON and could be a very promising materials for remineralisation of enamel. The two groups in the showed complete blockage and penetration ability of the surface of enamel as shown in Figures 2 and 3. Regarding color of demineralized enamel, this subsurface demineralization represents the first stage of caries formation. Which is then followed by bacterial infiltration of the enamel surface producing organic acids capable of dissolving the calcium and phosphate ions of the dental structure, thus causing lesions. Upon application of resin, the resin will reflect the same color as the surrounding tooth structure, thus color or shade matching is a resolved issue with ICON. With the incorporation of nano bioactive glass into the resin structure, that will eventually dissolve, the color matching would be questionable [24].
Much research approved maintaining color stability of the resin over time is mandatory. But it is generally accepted that all resin based dental materials degrade to some extent in the oral environment. Knosel proved resin infiltration improves the esthetic appearance of demineralized teeth with reported durability over 6 months [25]. Also, in agreement with Paris that evaluated the ability of resin infiltration to camouflage enamel white spot lesions immediately and after a staining period. According to ΔE and refractive index, all tested in filtrants showed significantly acceptable color match with sound enamel. Using the advantages of spectrophotometry and the CIE L*a*b* coordinate system, its repeatability, sensitivity, equitability and ability for the detection of small color variation. Color stability after staining was assessed in the current study to evaluate the effect of modification of ICON on the aesthetic aspect of the restoration. The spectrophotometric analysis revealed no significant differences between ΔE, ΔL and ΔA. Significant difference was only found in ΔB.
That is to proof that the maintained color was stable in both groups (I and II) after fourteen days of immersion in the staining solution and that degradation of bioactive glass did not affect the color stability of samples despite the significant difference found in ΔB that meant yellowish discoloration of samples that may be attributed to the yellowish color of the nano bioactive glass itself.
Conclusion
Addition of nano bioactive glass to resin infiltrate structure is promising in the remineralization capability of the resin infiltration technique and would not compromise hardening effect of resin or penetration of the lesion or color change by time even upon staining.
References
- Attal JP, Atlan A, Denis M, et al. White spots on enamel: Treatment protocol by superficial or deep infiltration (part 2). Int Orthodont 2014; 12:1-31.
[Crossref] [Google Scholar] [Pubmed]
- Shimizu A, Yamamoto T, Nakashima S, et al. Measurement of surface hardness of primary carious lesions in extracted human enamel-Measurement of Knoop hardness using Cariotester. Dent Mater J 2015; 34:252-256.
[Crossref] [GoogleScholar] [Pubmed]
- Knösel M, Attin R, Becker K, et al. External bleaching effect on the color and luminosity of inactive white-spot lesions after fixed orthodontic appliances. Angle Orthodont 2007; 77:646-652.
[Crossref] [Google Scholar] [Pubmed]
- Manoharan V, Kumar SA, Arumugam SB, et al. Is resin infiltration a microinvasive approach to white lesions of calcified tooth structures?: A systemic review. Int J Clin Pediatr Dentistr 2019; 12:53-58.
[Crossref] [GoogleScholar] [Pubmed]
- Thomas A, Maimanuku L, Mohammadnezhad M, et al. Presence of behavioural risk factors among periodontitis patients in Suva, Fiji. J Oral Hyg Health 2018; 6:2332-2702. [Crossref]
[GoogleScholar] [Pubmed]
- Skallevold HE, Rokaya D, Khurshid Z, et al. Bioactive glass applications in dentistry. Int J Mole Sci 2019; 20:5960.
[Crossref] [Google Scholar] [Pubmed]
- Kim HJ, Mo SY, Kim DS. Effect of bioactive glass-containing light-curing varnish on enamel remineralization. Materials 2021; 14:3745.
[Crossref] [GoogleScholar] [Pubmed]
- Soares R, De Ataide ID, Fernandes M, et al. Assessment of enamel remineralisation after treatment with four different remineralising agents: A scanning electron microscopy (SEM) Study. J Clin Diagn Res 2017; 11:ZC136-ZC141.
[Crossref] [GoogleScholar] [Pubmed]
- Prabhakar AR, Arali V. Comparison of the remineralizing effects of sodium fluoride and bioactive glass using bioerodible gel systems. J Dent Res Dent Clin Dent Prospect 2009; 3:117-121.
[Crossref] [GoogleScholar] [Pubmed]
- Kooshki F, Pajoohan S, Kamareh S. Effects of treatment with three types of varnish remineralizing agents on the microhardness of demineralized enamel surface. J Clin Experim Dentistr 2019; 11:e630-e635.
[Crossref] [GoogleScholar] [Pubmed]
- Sideridou I, Tserki V, Papanastasiou G. Effect of chemical structure on degree of conversion in light-cured dimethacrylate-based dental resins. Biomaterials 2002; 23:1819-1829.
[Crossref] [GoogleScholar] [Pubmed]
- Subramaniam P, Babu KG, Lakhotia D. Evaluation of penetration depth of a commercially available resin infiltrate into artificially created enamel lesions: An in vitro study. J Conserv Dentistr 2014; 17:146.
[Crossref] [GoogleScholar] [Pubmed]
- Gurdogan EB, Ozdemir‐Ozenen D, Sandalli N. Evaluation of surface roughness characteristics using atomic force microscopy and inspection of microhardness following resin infiltration with icon®. J Esthet Restorat Dentistr 2017; 29:201-208.
[Crossref] [Google Scholar] [Pubmed]
- Paris S, Schwendicke F, Keltsch J, et al. Masking of white spot lesions by resin infiltration in vitro. J Dentistr 2013; 41:e28-e34.
- Zakizade M, Davoudi A, Akhavan A, et al. Effect of resin infiltration technique on improving surface hardness of enamel lesions: A systematic review and meta-analysis. J Eviden Based Dent Pract 2020; 20:101405.
[Crossref] [GoogleScholar] [Pubmed]
- Shaik ZA, Rambabu T, Sajjan G, et al. Quantitative analysis of remineralization of artificial carious lesions with commercially available newer remineralizing agents using SEM-EDX-in vitro study. J Clin Diagn Res 2017; 11:ZC20-ZC23. [Crossref]
[GoogleScholar] [Pubmed]
- El Meligy OA, Alamoudi NM, Ibrahim ST, et al. Effect of resin infiltration application on early proximal caries lesions in vitro. J Dent Sci 2021; 16:296-303.
[Crossref] [Google Scholar] [Pubmed]
- White spots on enamel: Treatment protocol by superficial or deep infiltration (part 2).
- Cazzolla AP, De Franco AR, Lacaita M, et al. Efficacy of 4-year treatment of icon infiltration resin on postorthodontic white spot lesions. Case Report 2018; 2018:225639.
[Crossref] [Google Scholar] [Pubmed]
- Paris S, Meyer-Lueckel H. Masking of labial enamel white spot lesions by resin infiltration-a clinical report. Quintessen Int 2009; 40. [Crossref]
[GoogleScholar] [Pubmed]
- Paris S, Meyer-Lueckel H. Inhibition of caries progression by resin infiltration in situ. Caries Res 2010; 44:47-54.
[Crossref] [GoogleScholar] [Pubmed]
- Poggio C, Ceci M, Beltrami R, et al. Color stability of esthetic restorative materials: A spectrophotometric analysis. Acta Biomater Odontol Scandin 2016; 2:95-101.
[Crossref] [Google Scholar] [Pubmed]
- Knösel M, Eckstein A, Helms HJ. Durability of esthetic improvement following Icon resin infiltration of multibracket-induced white spot lesions compared with no therapy over 6 months: A single-center, split-mouth, randomized clinical trial. Am J Orthodont Dentofac Orthoped 2013; 144:86-96.
[Crossref] [Google Scholar] [Pubmed]
- Hammad SM, El Banna M, El Zayat I, et al. Effect of resin infiltration on white spot lesions after debonding orthodontic brackets. Am J Dent 2012; 25:3-8. [Crossref]
[Google Scholar] [Pubmed]
- ElEmbaby AE. The effects of mouth rinses on the color stability of resin‐based restorative materials. J Esthet Restorat Dentistr 2014; 26:264-271.
[Crossref] [Google Scholar] [Pubmed]
Author Info
1Department of Prosthodontic Dentistry, King Salman International University,El Tur, EgyptCitation: Reem Ashraf, Effect of Resin Infiltrate Modified with Bioactive Glass on Hardness and Color Stability of White Spot Lesions, J Res Med Dent Sci, 2022, 10(5): 66-71.
Received: 21-Feb-2022, Manuscript No. 47175; , Pre QC No. 47175; Editor assigned: 23-Feb-2022, Pre QC No. 47175; Reviewed: 09-Mar-2022, QC No. 47175; Revised: 22-Apr-2022, Manuscript No. 47175; Published: 04-May-2022
Sources of funding : GB´s PhD-project on ethical challenges and decision-making in nursing homes has been financially supported by the Norwegian Extra Foundation for Health and Rehabilitation through EXTRA funds (grant no. 2008/2/0208).
