Review Article - (2023) Volume 11, Issue 1
Effect of Post Preparation Dentinal Hypersensitivity Treatment by Fractional CO2 (10600 nm) Laser on Shear Bond Strength of Resin Cement to Dentin: In Vitro Study
Rusal Mohammed Mubarak* and Basima Mohammed Ali Hussein
*Correspondence: Rusal Mohammed Mubarak, Department of Dentistry, Institute of Laser for Postgraduate Studies, University of Baghdad, Baghdad, Iraq, Email:
Abstract
Background: After crown preparation of vital tooth, the tooth would be sensitive due to increased number of open dentinal tubules. Dentinal hypersensitivity described as severe and sharp pain evoked by thermal, tactile, osmotic and chemical stimuli. Laser was considered as an effective treatment of dentinal hypersensitivity of exposed root dentin.
Aim of this study: To evaluate the desensitization effect of fractional CO2 laser (1 W, 2.5 ms, 2.5 mJ) and (1 W, 2.5 ms, 2.5 mJ) on shear bond strength of dentin to resin cement.
Materials and methods: Sixty three sound maxillary premolars (n=21) were collected and prepared occlusally to expose dentin, these teeth were divided into three groups. Group A: Dentin surface was irradiated with fractional CO2 (1 W, 2.5 mJ, 2.5 ms), group B: Dentin surface was irradiated with fractional CO2 (1 W, 3 mJ, 3 ms), group C: Control group. SEM investigation was done to evaluate laser effect on dentinal tubules after irradiation with fractional CO2. For each group temperature in the pulp during lasing was measured, furthermore roughness was measured before and after laser treatment. Shear Bond Strength (SBS) between dentin and cement was measured for all groups by universal testing machine.
Result: SEM evaluation showed complete occluding of dentinal tubules in group B, with partial occluding of tubules in group A. Laser treatment caused a significant increase in roughness in group A, with no significant increase in roughness in group B. Shear bond strength significantly increased with group A.
Conclusion: From obtained results, we can conclude that fractional CO2 laser can be considered as an effective treatment option for dentinal hypersensitivity. Shear bond strength can be improved with group A (1 W, 2.5 mJ, 2.5 ms).
Keywords
Desensitization, Chemical stimuli, Shear bond strength, Laser, Hypersensitivity
Introduction
Dentinal hypersensitivity is one of the most common complications of post preparation of full coverage crown of vital tooth, in which most of the clinician reported that most of their patient suffers from dentinal hypersensitivity after crown preparation [1]. Dentinal hypersensitivity characterized by severs sharp pain due to thermal, osmotic, chemical stimulus [2]. Maxillary premolars are more susceptible to hypersensitivity than other teeth and it is more common in young patients, decrease over 40 due to tertiary dentine formation [3,4]. Many theories have been trying to explain the mechanism of dentinal hypersensitivity but the most excepted is the hydrodynamic theory which was proposed by barnstorm and storm, it stated that dentinal hypersensitivity is due to rapid movement of dentinal fluids inside dentinal tubule [5]. According to the type of the stimuli the direction of fluid movement changes this affect the response to sensitivity for example, cooling, drying, hypertonic chemical and evaporating stimuli lead to movement of fluids away from dentin pulp complex, which induce sensitivity, while heat stimuli cause movement of fluids toward the pulp [6]. The most stimuli that trigger pain are cold stimuli, about 75% of patients feeling pain due to cold stimuli [7]. Other theories, such as the neural theory which suggested that the dentin was innervated by unmyelinated nerve fibers extended for short distance in the inner dentin and direct stimuli to the dentin evoke pain [8]. Also, the odontoblast transducer theory which suggested that the odontoblast (which is the cell that is responsible for dentin formation and they form the outermost layer of the dentin pulp complex with their processes projecting through the dentinal tubules) act as a receptor cells that mediated dental pain sensation, via synaptic junctions with nerve endings that located on the border of the dentin pulp complex [9]. Dentinal hypersensitivity or pulp tissue reaction is a big concern in crown preparation due to the removal of enamel and friction of the dentin, which leads to increase of opened dentinal tubules [10]. After crown preparation, about 1-2 million of dentinal tubules became liable and lacked of protection, this lead to subsequent dentinal sensitivity [11]. About 1.2–1.5 mm of the tooth structure removed during complete crown preparation to ensure proper adaptation and retention of the prosthesis [12]. Heat generation during preparation and bacterial byproduct formation induce pulpal irritation. Micro leakage of the provisional restoration into the dentinal tubules may induce hypersensitivity [13]. Cementation may also induce dentinal hypersensitivity to the prepared tooth due to impingement of cement into the opened tubules; this will cause changes in dentinal fluid movement and result in hydrostatic pressure [14]. Treatment of dentinal hypersensitivity of prepared teeth based on the occlusion of latent or open dentinal tubules and it should not interfere with crown retention [15]. Dentin desensitizing agents are commonly used in dental practice, but their effects on crown retention have been questionable [16]. On the other hand, many studies used different lasers for treatment of dentinal hypersensitivity and improved crown retention, or at least did not interfere with crown retention [17]. However, the consequence of desensitizing treatment by fractional CO2 on the retention of prosthesis has not been documented. Therefore, the aim of this study was to evaluate the effect of desensitizing by fractional CO2 on shear bond strength of zirconia to dentin cemented by self-adhesive resin cement.
Materials and Methods
Tooth collection and preparation
Sixty three sound maxillary premolars were collected from orthodontic clinics; patients ages ranged from (18-30). All the samples were preserved in a 1% thymol solution until use. The teeth were molded in a cylindrical cold cure acrylic mold, with the root embedded in the mold (Figure 1).
Figure 1: Maxillary premolars embedded in cold cure acrylic mold.
After tooth molding, cutting of the teeth is achieved with the help of a dental surveyor, a hand piece and a diamond disc. Each tooth was fixed on the surveyor with the use of a customized holder, while the hand piece with the disc could be moved in a horizontal line (Figure 2). The cutting was done perpendicular to the long axis of the tooth, on the occlusal side of the teeth [18]. The cutting was done to the central groove. Cooling by water was continuous throughout the cutting procedure.
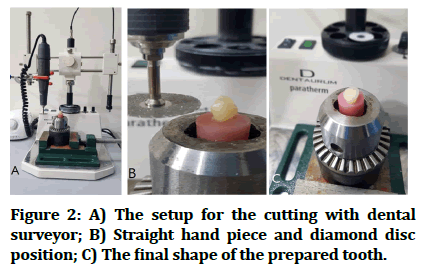
Figure 2: A) The setup for the cutting with dental surveyor; B) Straight hand piece and diamond disc position; C) The final shape of the prepared tooth.
After tooth preparation, the occlusal surface polished with non-fluoride polishing paste and a rubber cup for 15 sec. Then the teeth washed in ultrasonic cleaner for 15 min. Finally, teeth were divided randomly into three groups, group A, group B, both treated by laser and group C, which is the control group.
Group A: Fractional CO2 (1 W, 2.5 mJ, 2.5 ms).
Group B: Fractional CO2 (1 W, 3 mJ, 3 ms).
Group C: Is the control group.
Laser application
After tooth preparation, two groups (two different parameters) were treated with fractional CO2 laser (CO2 fractional laser brochure, JHC 1180, China) (Figure 3). Laser energy was delivered in the order mode and a circular area of 8 mm in diameter in the center of the dentin surface, the hand piece of the laser was held perpendicular to the dentin surface.

Figure 3: Fractional CO2 laser.
SEM examination
Effect of laser on dentinal tubules was evaluated by examination under scanning electronic microscope SEM (INSPECT F 50, FEI company, USA), (Figure 4).

Figure 4: Scanning electronic microscope.
Measurement of temperature
5 samples for each of the laser treated groups (groups A and B) were used to measure temperature rise during laser application with the use of thermometer (amprobe TMD-56). The teeth were prepared with Sx pro taper file to make path for the thermo couple wire (with a range of (-200°C to 1372°C), head diameter of 0.8 mm) to be inserted from the apical orifice of the root till reach the roof of the pulp chamber, fixed with thermal grease. The samples were placed in the water bath at 37°C; the root only was immersed in the water during testing (Figure 5).
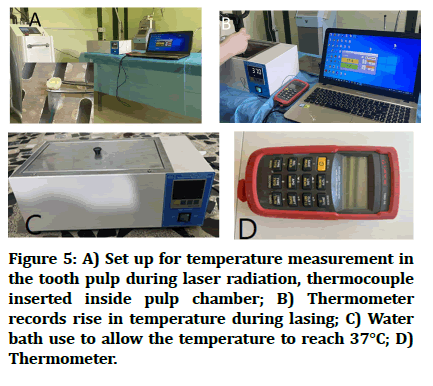
Figure 5: A) Set up for temperature measurement in the tooth pulp during laser radiation, thermocouple inserted inside pulp chamber; B) Thermometer records rise in temperature during lasing; C) Water bath use to allow the temperature to reach 37°C; D) Thermometer.
Roughness assessment
For all samples treated by laser, roughness was measured before and after laser application, was done with a profile meter (surface roughness tester SRT-6210, China) (Figure 6). Three measurements from different points of the dentin surface were done and the mean of the three reads was calculated.
Figure 6: A) Profile meter for roughness assessment; B) During measurement.
Cementation of the zirconia to the dentin
The first step is to fabricate zirconia cylinders (KATANATM Zirconia, Ht, Japan) with 3 mm diameter and 5 mm height. They were fabricated with CAD\CAM. For cementation, self-adhesive resin cement (breeze, pentron clinical, CA92867, USA) was used, it was auto mixed, using disposable mixing tips supplied with the cement kit and applied directly to tooth surface. Silicon mold was fabricated with a central hole of 3 mm in diameter, 3 mm in height divided from the internal surface into 1 mm for cement and 2 mm for the disc to insure proper curing. To avoid any air bubbles and proper cementation, a load of 2 Kg was used during the cement setting with the use of dental surveyor (Figure 7) [19]. After 4 minutes the load removed after curing. The samples left on the table for one hour to ensure complete curing. After that, the cemented samples immersed in the water bath at 37°C for 24 hours before shear bond strength testing.
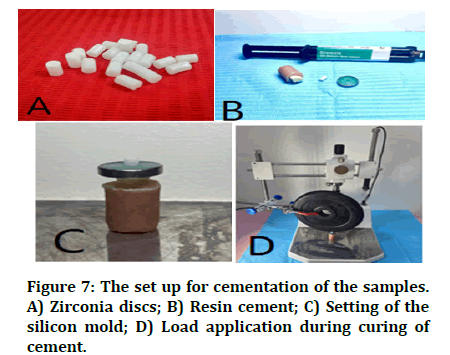
Figure 7: The set up for cementation of the samples. A) Zirconia discs; B) Resin cement; C) Setting of the silicon mold; D) Load application during curing of cement
Measuring shear bond strength
Measuring shear bond strength was done using instron universal testing machine (ARYEE, WDW-50, and 50 KN. China). The tooth was fixed in a horizontal plane and a stainless steel chiseled shaped blade would pass through the tooth resin cement interface till complete separation. It shows the universal testing machine (Figure 8).
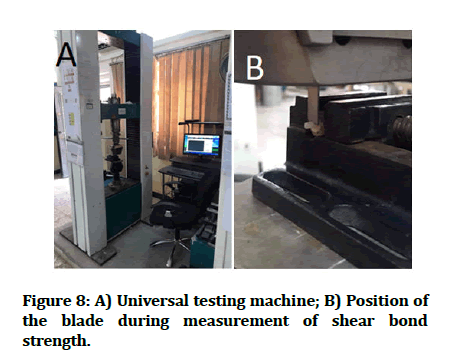
Figure 8: A) Universal testing machine; B) Position of the blade during measurement of shear bond strength.
Results
In this chapter, the results obtained from evaluation of the laser effect on occluding of open dentinal tubules, measurement of temperature and roughness, examination of shear bond strength will be maintained. Statistical analysis using descriptive statistics, paired T test, independent samples T test and two way ANOVA analysis using SPSS.
Measurement of temperature
According to Table 1, the mean of rise in temperature for each group samples was recorded. The maximum rise in temperature was 1.7°C in group B (CO2, with 3 mJ), while in group A (CO2, 2.5 mJ), the maximum temperature rise was 1.3°C (Table 1).
| Groups | Mean | Standard Deviation (SD) |
|---|---|---|
| Group A | 1.02 | 0.16 |
| Group B | 1.58 | 0.08 |
Table 1: The mean and standard deviation of the experimental groups.
SEM evaluation
Examination of dentinal tubules was done by Scanning Electronic Microscope (SEM) (INSPECT F50, FEI company, USA) (Figure 9). SEM evaluation showed open dentinal tubules in group C, the control group, while in group A with CO2 2.5 mJ laser treated dentin there was partial occlusion of dentinal tubules with no cracks. Group B CO2 laser treated dentine (3 mJ) clear surface with complete occlusion of dentinal tubules and no cracks or carbonization found.
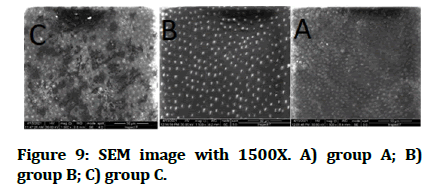
Figure 9: SEM image with 1500X. A) group A; B) group B; C) group C.
Roughness assessment
Statistical analysis of changes in roughness in group A and group B was measured. The mean of roughness before and after laser irradiation maintained (Figure 10). Descriptive and statistical analysis using paired T test results shows a significant increase in roughness in group A (2.5 mJ), while in group B no significant increase in roughness (Table 2).
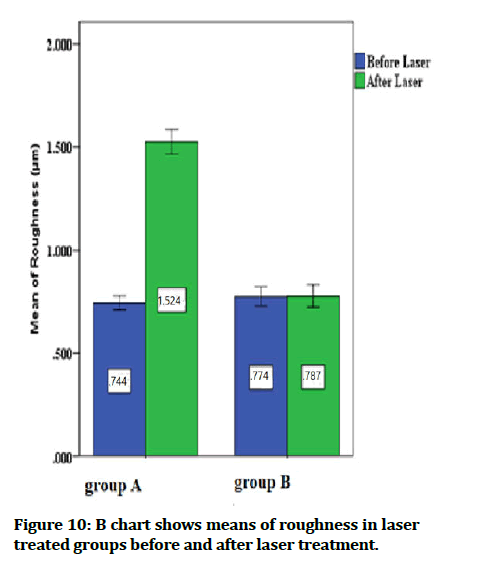
Figure 10: B chart shows means of roughness in laser treated groups before and after laser treatment.
| Groups | Before laser | After laser | Paired T test | P value | |
|---|---|---|---|---|---|
| Group A | Minimum | 0.662 | 1.393 | 34.519 | 0.000 Sig. |
| Maximum | 0.830 | 1.656 | |||
| Mean | 0.744 | 1.524 | |||
| ± SD | 0.050 | 0.082 | |||
| Group B | Minimum | 0.684 | 0.651 | 0.484 | 0.640 NS |
| Maximum | 0.913 | 0.917 | |||
| Mean | 0.774 | 0.787 | |||
| ± SD | 0.066 | 0.078 | |||
| Statistics | T test | 1.157 | 20.865 | ||
| P value | 0.262 NS | 0.000 Sig. | |||
Table 2: Descriptive and statistical analysis for roughness measurement in group A and B.
Shear bond strength
Shear bond strength measurements for the three groups (Table 3). It shows that the highest mean value was in group A (CO2 laser with 2.5 mJ) with (104.4) and the lowest mean with the control group (group C) with (93.500). Statistical analysis between groups using ANOVA indicated a significant difference (Table 4).
| Groups | Mean | ± SD | ± SE | Minimum | Maximum |
|---|---|---|---|---|---|
| 2.5 mj CO2 laser | 104.440 | 9.263 | 2.929 | 90.000 | 115.000 |
| 3 mj CO2 laser | 96.000 | 9.661 | 3.055 | 85.000 | 115.000 |
| Control | 93.500 | 7.835 | 2.478 | 85.000 | 105.000 |
Table 3: Descriptive and statistical analysis of the shear bond strength for all groups.
| Sum of squares | DF | Mean square | F | P value | |
|---|---|---|---|---|---|
| Between groups | 657.224 | 2 | 328.612 | 4.099 | 0.028 sig. |
| Within groups | 2164.724 | 27 | 80.175 | ||
| Total | 2821.948 | 29 |
Table 4: Statistical comparison between groups using (one way ANOVA) shows significant deference between groups.
Further analysis between every two groups was done using tukey HSD test (Table 5). Only significant difference between group A (CO2 laser with 2.5 mJ) and group C (control).
| Multiple comparisons | |||
|---|---|---|---|
| Dependent variable: Shear bond strength Tukey HSD |
|||
| (I) Groups | (J) Groups | Mean difference (I-J) | P value |
| 2.5 mj CO2 laser | 3 mj CO2 laser | 8.440 | 0.107^ |
| Control | 10.940 | 0.029* | |
| 3 mj CO2 laser | 2.5 mj CO2 laser | -8.440 | 0.107^ |
| Control | 2.500 | 0.808^ | |
Table 5: Tukey HSD test, to make comparison between every two different groups.
Discussion
Before the preface of implant to dental practice, the only treatment or the restoration of edentulous area was fixed partial denture, which still very popular and effective treatment approach till present time [20]. An invasive treatment approach required removal of tooth structure, in some instants, vital or even sound tooth, to be used as an abutment for fixation of the bridge. The removal of tooth structure generates open dentinal tubules that susceptible to sensitivity. The best treatment of this postoperative complication is the occluding of dentinal tubules without adverse effects on the retention of the prosthesis. CO2 laser is one of the lasers used in dental practice and many clinical trials found that it can be used safely on dental hard tissue without necrosis or pulp damage and had pleasing result especially with dentin conditioning and desensitizing [21]. Considering laser's effect on temperature change, it was concluded that temperature rise within groups A and B was within or even blow the accepted degree of temperature rise that causes pulp damage. The maximum temperature rise that will not affect the vitality of the dental pulp is 5.5 [22]. In group A, the maximum temperature rise was 1.3℃, while in group B it was 1.7°C. This may be attributed to the interval times (time between pulses), which was 1.0 ms, also low energy was used for both experimental groups, in which 2.5 mJ and 3 mJ reduced thermal effect on pulp tissue. Many studies approve the effect of CO2 laser on the obliteration of open dentinal tubules, CO2 laser have low penetration depth, maximum hydroxyapatite absorption and high water absorption, all these factors result in its ability to modify dentin structure safely [23,24]. These results agree with those of Golami, et al. who used different lasers to study their effects on occluding of dentinal tubules, one of these lasers was CO2 with 50 W, 2.5 mj, ultra pulse mode that resulted with successful melting of dentinal tubules leading to partial occlusion of the tubules, with no carbonization or cracks [25]. Study used continuous mode CO2 with 1 W, 50 Hz, 20 mJ and also got complete obliteration of dentinal tubules without hazard effect on dental pulp [26]. These support the results in this study, according to SEM evaluation, group A 2.5 mJ, showed partial occluding to the tubules, while group B 3 mJ showed greater effect with complete occluding of dentinal tubules and both groups have no cracks or carbonization to dentin surface. Occluding of dentinal tubules is the first part of laser treatment; the other part is to make sure that treatment of hypersensitivity will not affect adversely the bonding strength. During laser application, roughness of tooth surface shows a significant increase in group A and marginal increase in group B and this refer to the laser interaction with the water and hydroxyapatite that result in melting and recrystallization of dentin and producing fungi form projection on the dentin surface [27]. Considering laser effect on roughness, it is clear that lower energy induces higher roughness, while with higher energy and complete occluding of dentinal tubules; this will lead to a non-significant increase in roughness. On the other hand, SEM evaluation of the effect of CO2 of this study showed dentin debris produced from lasing process deposited on the orifice of tubules as well as overlapping of the debris deposition this will increase the roughness of the irradiated dentin surface even with complete occluding of dentinal tubules. Increase in dentin surface roughness will improve bonding to dentin by increasing shear bond strength [28]. Another study also supports that increase spatial overlap between pulses will increase the roughness caused by the laser and this will increase shear bonding strength to dentin [29]. According to authors knowledge no previous study that discusses the effect of desensitization of dentin by fractional CO2 on shear bond strength to cement, but uses of fractional CO2 for dentin surface treatment or conditioning found that 0.8 W, 10 Hz, 80 mJ will reduce shear bond strength of resin cement to dentin, this supports our results in which increase energy irradiation to dentin surface, reduce shear bond strength [30]. In this study, group A with 2.5 mJ had significantly higher shear bond strength than group B (3 mJ) and group C (control). This could be attributed to the significant increase in surface roughness in group A and no significant increase in roughness in group B.
Conclusion
According to the result we can concludes the following:
• CO2 laser is an effective treatment approach for dentinal hypersensitivity with partial occluding, or complete occluding of dentinal tubules without any side effects like carbonization, cracks, or inducing damage to the pulp tissue.
• Increase in dentin surface roughness induces an increase in shear bond strength to resin cement.
• Shear bond strength between dentin and resin cement was improved significantly when dentin was treated with CO2 laser at (1 W, 2.5 mJ, 2.5 ms, 1 ms interval time).
References
- Abdollahi A, Jalalian E. Effectiveness of two desensitizer materials, potassium nitrate and fluoride varnish in relieving hypersensitivity after crown preparation. J Contemp Dent Pract 2019; 20:489-493. [Googlescholar][Indexed]
- Trushkowsky RD, Oquendo A. Treatment of dentin hypersensitivity. Dent Clin 2011; 55:599-608. [Crossref][Googlescholar][Indexed]
- Al-khafaji ZR, Awazli LG, Al-Maliky MA. Effects of diode laser 940 nm with and without 5% sodium fluoride white varnish with tri calcium phosphate on dentin permeability (in vitro study). Iraqi J Laser 2018; 17:17-25. [Googlescholar]
- Splieth CH, Tachou A. Epidemiology of dentin hypersensitivity. Clin Oral Investig 2013; 17:3-8. [Crossref][Googlescholar][Indexed]
- Brannstrom M, Astrom A. A study on the mechanism of pain elicited from the dentin. J Dent Res 1964; 43:619-625. [Crossref][Googlescholar][Indexed]
- Roberson T, Heymann HO, EJ Swift Jr. Sturtevant’s art and science of operative dentistry. Elsevier health sciences. 2006. [Googlescholar]
- Miglani S, Aggarwal V, Ahuja B. Dentin hypersensitivity: Recent trends in management. J Conserv Dent 2010; 13:218. [Crossref][Googlescholar][Indexed]
- West NX, Lussi A, Seong J, E Hellwig, et al. Dentin hypersensitivity: Pain mechanisms and aetiology of exposed cervical dentin. Clin Oral Investig 2013; 17:9-19. [Crossref][Googlescholar][Indexed]
- Magloire H, Couble ML, Romeas A, et al. Odontoblast primary cilia: Facts and hypotheses. Cell Biol Int 2004; 28:93-99. [Crossref][Googlescholar][Indexed]
- Davis GR, Tayeb RA, Seymour KG, et al. Quantification of residual dentine thickness following crown preparation. J Dent 2012; 40:571-576. [Crossref][Googlescholar][Indexed]
- Richardson D, Tao L, Pashley DH. Dentin permeability: Effects of crown preparation. Int J Prosthod 1991; 4. [Googlescholar][Indexed]
- Shillingburg H, Hobo S, Whitsett L. Fundamentals of fixed prosthodontics. Chicago: Quintessence, 1981; 401-417.
- Langeland K, Langeland LK. Pulp reactions to crown preparation, impression, temporary crown fixation and permanent cementation. J Prosthet Dent 1965; 15:129-143. [Crossref][Googlescholar][Indexed]
- Rosenstiel SF, Rashid RG. Post cementation hypersensitivity: Scientific data versus dentists perceptions. J Prosthod 2003; 12:73-81. [Crossref][Googlescholar][Indexed]
- Kumar S, PL Rupesh, SG Daokar, et al. Effect of desensitizing laser treatment on the bond strength of full metal crowns: An in vitro comparative study. J Int Oral Health 2015; 7:36. [Googlescholar][Indexed]
- Mapkar MA, Jagtap A, Asadullah SRS. Effect of two different types of desensitizing agents on crown retention using glass ionomer cement. Int J Oral Care Res 2018; 6:12. [Crossref][Googlescholar]
- Sipahi C, Cehreli M, Ozen J, et al. Effects of pre-cementation desensitizing laser treatment and conventional desensitizing agents on crown retention. Int J Prosthodont 2007; 20:289-292. [Googlescholar][Indexed]
- Dawood RM. Evaluation of shear bond strength of zirconia to tooth structure by resin cement after zirconia different surface treatment techniques. A master thesis, Department of conservative dentistry, University of Baghdad, 2014. [Crossref][Googlescholar]
- Beuer F, Schweiger J, Edelhoff D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br Dent J 2008; 204:505-511. [Crossref][Googlescholar][Indexed]
- Scurria MS, Bader JD, Shugars DA, et al. Meta-analysis of fixed partial denture survival: Prostheses and abutments. J Prosthet Dent 1998; 79:459-464. [Crossref][Googlescholar][Indexed]
- WALSH LJ. Clinical evaluation of dental hard tissue applications of carbon dioxide lasers. J Clin Laser Med Surg 1994; 12:11-15. [Crossref][Googlescholar][Indexed]
- Van Gemert M, Niemz M. Laser tissue interactions: Fundamentals and applications. Springer Berlin Heidelberg. 2013. [Googlescholar]
- Freitas PM, Simoes A. Lasers in dentistry: Guide for clinical practice. Wiley, 2015. [Googlescholar]
- Coluzzi DJ, Parker SPA. Lasers in dentistry current concepts. Springer international publishing. 2017. [Crossref][Googlescholar]
- Gholami GA, et al. An evaluation of the occluding effects of Er; Cr: YSGG, Nd: YAG, CO2 and diode lasers on dentinal tubules: A scanning electron microscope in vitro study. Photomed Laser Surg 2011; 29:115-121. [Crossref][Googlescholar][Indexed]
- Saluja M, Grover HS, Choudhary P. Comparative morphologic evaluation and occluding effectiveness of Nd: YAG, CO2 and diode lasers on exposed human dentinal tubules: An in vitro SEM study. J Clin Diagn Res 2016; 10:ZC66. [Crossref][Googlescholar][Indexed]
- Silberman JJ, Dederich DN, Vargas M, et al. SEM comparison of acid etched, CO2 laser irradiated and combined treatment on dentin surfaces. Lasers Surg Med 1994; 15:269-276. [Crossref][Googlescholar][Indexed]
- Hossain M, Y Nakamura, Y Yamada, et al. Analysis of surface roughness of enamel and dentin after Er Cr: YSGG laser irradiation. J Clin Laser Med Surg 2001; 19:297-303. [Crossref][Googlescholar][Indexed]
- Gardner AK, Staninec M, Fried D. The influence of surface roughness on the bond strength of composite to dental hard tissues after Er: YAG laser irradiation. In lasers in dentistry XI. International society for optics and photonics. 2005. [Crossref][Googlescholar]
- Al-Jeaidi Z. Influence of fractional carbon dioxide laser in comparison to ErCr-YSGG on the dentin bond integrity of bioactive materials. Pak J Med Sci 2020; 36:526. [Crossref][Googlescholar][Indexed]
Author Info
Rusal Mohammed Mubarak* and Basima Mohammed Ali Hussein
Department of Dentistry, Institute of Laser for Postgraduate Studies, University of Baghdad, Baghdad, IraqReceived: 07-Oct-2022, Manuscript No. JRMDS-22-52837; , Pre QC No. JRMDS-22-52837; Editor assigned: 14-Oct-2022, Pre QC No. JRMDS-22-52837; Reviewed: 24-Oct-2022, QC No. JRMDS-22-52837; Revised: 26-Dec-2022, Manuscript No. JRMDS-22-52837; Published: 04-Jan-2023
