Research - (2022) Volume 10, Issue 9
Does Local Delivery of Simvastatin-Loaded Gelatin Sponge Accelerate Mandibular Fracture Healing?
Ahmad Albassal1, Nuraldeen Maher Al-Khanati1,2* and Munir Harfouch1
*Correspondence: Nuraldeen Maher Al-Khanati, Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Syrian Private University, Damascus, Syria, Email:
Abstract
Objective: The aim of this study was to assess the effect of local application of 10mg simvastatin on bone healing in mandibular fractures. Methodology: Participants with anterior mandibular fractures were randomly assigned into the two groups of this partially-blinded randomized clinical study. The mandibular fractures were managed via standard technique. Simvastatin-loaded gelatin sponge was locally applied along the fracture line after open reduction and internal fixation and before suturing in the study group. Only saline with gelatin sponge was used as a placebo in the control group. Participants were radiographically followed up after 1 week, 2 months, and 4 months. CBCT images were used to measure grey-scale values, and to indicate fracture union at the 2-month and 4-month follow-ups. Results: 24 anterior mandibular fractures (n=24) were included in all stages of this study. Mean participants age was 30.8 (± 11.7) years. Comparisons showed significant differences in mean grey-scale values at 2-month (P=0.022) and 4-month (P=0.009) follow-ups between the simvastatin and control groups. Differences regarding fracture union between the simvastatin and control groups were insignificant after 2 months (P=0.273), but significant after 4 months (P=0.003). Conclusion: It can be concluded that local application of 10mg simvastatin with gelatin sponge carrier along the fracture lines may hasten the bone healing in mandibular fractures.
Keywords
Mandibular fracture, Statins, Simvastatin, CBCT, Grey scale values
Introduction
The mandible is the largest and strongest facial bone, nevertheless it is more frequently fractured than any other part of the maxillofacial skeleton [1,2]. 40 to 62% of all facial fractures are mandibular fractures [3]. Anterior mandibular fractures were often reported to be the most common mandibular fracture sites [4]. Healing of these fractures in the best and fastest ways is the goal of every oral and maxillofacial surgeon when managing such cases. Many studies have been conducted to evaluate speeding-up the fracture healing by local and systemic use of a range of items, e.g., vitamin D, parathyroid hormone, growth factors, calcium sulfate and bone morphogenetic proteins (BMPs) [5-7]. Hyperbaric oxygen, mechanical, electrical and magnetic stimulating effects on increasing the speed of fracture healing were also studied [7,8]. Local application of BMPs has shown enhanced fracture healing process [9]. Simvastatin is a cholesterol-lowering drug that can induce bone morphogenetic protein 2 (BMP-2) [10,11]. BMP-2 is a growth factor with well-studied important bone regeneration and osteoinductive properties [12,13]. Hereby, this study aimed to assess the effect of local delivery of simvastatin on the bone healing quality in the management of anterior mandibular fractures.
Methods
A total of 24 participants with mandibular fractures were enrolled in this prospective partially-blinded randomized clinical trial. Patients were selected from the cases admitted to the Emergency department of a university hospital (Damascus, Syria) in the period between Apr 2019 to Dec 2020. The Research Ethics Committee of Damascus University granted its approval to conduct this clinical research (registration no. 2019- 1000). Before being included in this trial, all patients signed informed consent form. Inclusion criteria included the followings: 1) mandibular fracture at the symphysis or para symphysis; 2) no signs of infection at the fracture site; 3) age of more than 18 years. Comminuted fractures, edentulous fractures, pathological fractures, and gunshot injuries were excluded. Moreover, patients with medical contraindication, osteoporosis, any systemic problem that may interfere with bone healing, or patients currently under systemic lipid-lowering statin-class treatment were also excluded. Every patient had a comprehensive clinical examination as well as detailed history taking. A preoperative computed tomography (CT) imaging was acquired to demonstrate the extent of the fracture line, the degree and direction of displacement, and the relationship of teeth included in the fracture line. All surgeries were carried out by the same surgeon and operative team.
Patients were randomly assigned into two groups i.e., study and control groups. Randomization was performed using a computer-generated random number list. All included fractures (in both groups) were managed by open reduction and internal fixation (ORIF) via standard technique under general anesthesia and nasotracheal intubation. Intraoral approach was mainly used to expose the fractured bone through vestibular incision. However, extraoral approach was performed only if trauma-related skin laceration existed. Patients were kept unaware to which group they were allocated. Simvastatin tablet (10 mg; Simvastatin Normon, Laboratorios Normon, S.A.- Madrid, Spain) was dissolved in 2 ml saline solution and dripped onto a piece (4x2x1cm) of sterile absorbable gelatin sponge (GelSpon® “Bovine Origin”, Eucare Pharmaceuticals Limited- Chennai, India) as a carrier. Local application of a simvastatin-impregnated gelatin sponge along the fracture line after internal fixation and just before suturing was done in the study group. While only saline with gelatin sponge was used as a control. For all patients, intermaxillary fixation was applied intraoperatively and left for 1 week after. Surgical wound was closed in layers using polyglactin suture material and with nylon suture material for the most superficial stitches on the mucosa or skin. Sutures were removed after 1 week for intraoral sutures, and 5 days for skin stitches. Duration of each surgery was measured from the moment of making the incision to the time of wound closure. Postoperative medical prescription consisted of antibiotics (intramuscular ceftriaxone 1g twice/day for 5 days), non-steroidal anti-inflammatory drugs (intramuscular diclofenac 75mg twice/day for 5 days), and chlorhexidine 0.12% mouthwash for 10 days. Postsurgical instructions also included strict instructions regarding oral hygiene and to follow soft diet for 3 weeks.
Patients’ follow-ups were 1 week, 2 months, and 4 months after surgery. In these follow-up visits, conebeam computed tomography (CBCT) images were made.
All images were taken using the same CBCT device (PaXi3D Green; Vatech Co. Ltd.) and exposure parameters (98 kVp, 11.4 mA, and FOV: 12x9 cm). CBCT data were extracted as digital imaging and communications in medicine (DICOM) files. DICOM data were transformed to Ez3D Plus software V 1.2.6 (Vatech Co. Ltd. Gyeonggido, South Korea). In order to measure grey-scale values, as an indicator for bone density, a profile line was drawn along the fracture line twice on two sequent thin (1 mm) slices of the axial plane. The mean value of these profile lines was used as indicator of fracture line’s bone density at each follow-up. Fracture union was another radiographic variable observed at the 2-month and 4-month follow-ups. This was identified by fracture line absence or the presence of anatomical continuous structure at the fracture site [14]. The process was standardized by measuring and fixing the distance and the angle of the profile line in relation to a reference line. All grey scale values measurements were done in standard fixed area of the fracture between the two ORIF mini-plates. The patient head position was also standardized in coronal, axial, and sagittal planes, so we ensure the reproducibility of image in the 3 follow-up timepoints.
Data were collected and presented as frequencies and mean ± standard deviation (SD). Statistical analyses were performed using t-tests and chi-square tests with SPSS version 19 (IBM Corp., Armonk, NY, USA). Statistical significance was set at P<0.05.
Results
Out of 53 patients with mandibular fractures that were initially evaluated, 36 patients were allocated to the study and control groups (Figure 1). After receiving the surgical intervention, 5 participants were lost to follow up and 7 were excluded from the study due to titanium plates proximity and/or screws angulation in ways that methodologically interfere with bone density measurements. Only 24 patients, 20 males and 4 females, with 24 anterior mandibular fractures (n=24) were included in all phases of this randomized clinical trial. Mean patients age was 30.8 ( ± 11.7) years. Patients’ demographics and fractures’ characteristics are presented comparing the two study groups (Table 1).
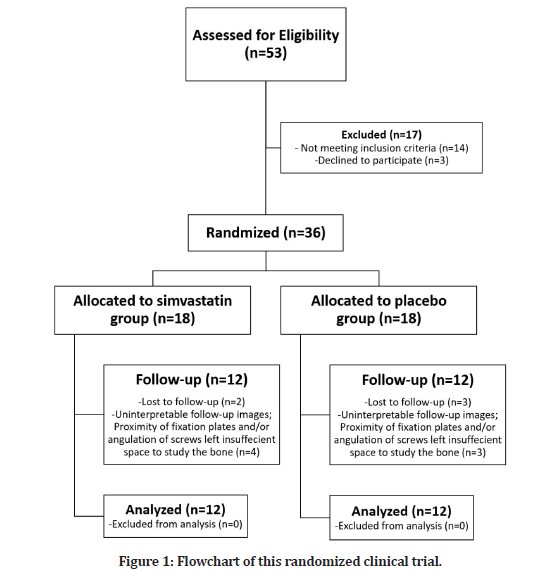
Figure 1: Flowchart of this randomized clinical trial.
| Characteristic | Simvastatin Group (n=12) | Control Group (n=12) | P-Value | Total (n=24) |
|---|---|---|---|---|
| Age (years) † | 30.3 ± 11.5 | 31.3 ± 12.3 | 0.826* | 30.8 ± 11.7 |
| Gender ‡ | 1.000** | |||
| Male | 10 | 10 | 20 | |
| Female | 2 | 2 | 4 | |
| Fracture type/side ‡ | 0.403** | |||
| Symphysial | 2 | 2 | 4 | |
| Right parasymphysial | 4 | 7 | 11 | |
| Left parasymphysial | 6 | 3 | 9 | |
| Fracture displacement ‡ | 0.219** | |||
| Displaced | 4 | 7 | 11 | |
| Non-displaced | 8 | 5 | 13 | |
| Etiology of fracture ‡ | 0.801** | |||
| Fall | 4 | 5 | 9 | |
| Road traffic accident | 6 | 6 | 12 | |
| Assault | 2 | 1 | 3 | |
| Surgical approach ‡ | 0.537** | |||
| Intraoral | 11 | 10 | 21 | |
| Extraoral | 1 | 2 | 3 | |
| Surgery duration (min) † | 65.3 ± 4.7 | 63.9 ± 5.4 | 0.525* | 64.6 ± 5.0 |
| Bone density measurements † | ||||
| Grey scale values- 1w | 896.9 ± 173.7 | 917.3 ± 265.8 | 0.826* | 907.1 ± 219.8 |
| Grey scale values- 2m | 1283.6 ± 310.2 | 1001.7 ± 245.6 | 0.022* | 1142.6 ± 309.2 |
| Grey scale values- 4m | 1587.4 ± 299.1 | 1220.1 ± 324.8 | 0.009* | 1403.8 ± 358.4 |
| Fracture union- 2m ‡ | 0.273** | |||
| Yes | 3 | 1 | 4 | |
| No | 9 | 11 | 20 | |
| Fracture union- 4m ‡ | 0.003** | |||
| Yes | 8 | 1 | 9 | |
| No | 4 | 11 | 15 | |
| †Expressed as mean ± SD; ‡Expressed as frequency; *Analyzed by independent t-tests; **Analyzed by Chi-square tests; SD=standard deviation; min=measured by minutes; 1w=baseline measurement at 1 week after surgery; 2m=2-month follow-up; 4m=4-month follow-up | ||||
Table 1: Participants characteristics and study results.
Inter-group comparison showed no significant differences in mean grey-scale values at baseline one week after ORIF surgery between the simvastatin and control groups (P=0.826). The differences in the bone density measurements between the two groups were statistically significant at 2-month (P=0.022) and 4-month (P=0.009) follow-ups. Differences regarding fracture union between the simvastatin and control groups were insignificant after 2 months (P=0.273), but significant after 4 months (P=0.003).
Discussion
Healing fractures in the shortest possible period of time is important in the context of providing better treatment services for every patient with maxillofacial trauma. Various methods have been used to promote early bone healing of mandibular fractures. The medical literature includes numerous articles regarding the applications of bone tissue engineering in the delivery of bone morphogenetic proteins (BMPs) and vascular endothelial growth factor (VEGF), two growth factors that have been extensively investigated for their use in bone regeneration [9,15-17]. However, these are costly agents with a relatively short half-life, and they are not easy to be processed in appropriate scaffolds and carriers as required for bioactivity [18]. Therefore, small-molecule less-expensive drugs that can be applied and released with aid of long-lasting carriers to stimulate production of BMPs and VEGF are highly valuable in the fields of tissue engineering. These include simvastatin, a lipophilic statin that can easily permeate cells and make its effects at tissue levels [10].
Systemic administration of simvastatin affects the entire body, and its bioavailability rapidly decreases due to hepatic metabolization with low concentration reaching the target tissue [19]. Only less than 5% of statin oral dose reaches circulation and therefore its distribution into bone microenvironment is negligible [20]. Local administration avoids simvastatin hepatic metabolism and reduces risks of drug toxicity [21]. Administration of simvastatin via carriers, such as gelatinous sponges, allows for gradual release of the drug maintaining its bioavailability at the fracture site for a longer period of time. It was observed that locally applied statins were 50 times more active than oral administration and had worthwhile osteo-inductive effect [22]. However, and to the best of our knowledge, no previous clinical studies have examined the effect of topical simvastatin application on mandibular fractures healing.
There are no ideal synthetic or biological carriers for local administration because they can be affected by the surrounding microenvironments, and inflammatory reactions leading to rejection can be developed [23]. Nevertheless, many scaffolds or carriers have been used for local application and releasing of statins including: gelatin sponge [24,25], collagen matrix [26], methylcellulose gel [27], and hydroxyapatite/poly(lacticco- glycolic acid) microspheres [28]. In the present study, gelatin sponge was chosen because it is highly biocompatible, bioabsorbable, and easily adaptable [25]. Slow releasing of simvastatin via this carrier is also very important to eliminate clinical signs of the potential inflammatory reaction. Stein et al. found less inflammation was associated with reduced simvastatin dose [29].
In this study, CBCT imaging was used to assess bone healing at the fracture line as it was considered safe, accurate and reproducible imaging technique [30]. CBCT clearly outperforms other dental imaging techniques, and is considered an excellent tool for viewing anatomical bony structures in three dimensions [31,32]. It also provides high image resolution and good pixel/noise ratio [33]. It was not recommended to use grayscale values of CBCT to assess bone density as an absolute value [34,35]. CBCT was known to be unable to provide Hounsfield unit (HU) measurements [33,34]. However, several authors have argued that the grayscale values of CBCT could be similar to HU [36,37]. In the present study, the gray scale values of the fracture line on standardized CBCT images were compared between the study and control groups. This eliminated the need for absolute values. Comparison of grayscale values in CBCT is suitable and safe alternative to histological study to assess the amount of new formed bone [38].
It is known that the bone healing process and the related post-operative symptoms can greatly be influenced by many factors such as the experience of the surgeon, surgery duration, patient’s characteristics and medical prescription [39,40]. In this study, the surgical procedure was performed by the same surgical team for all patients, no significant differences were found between the two groups in age and gender variables, and the same antibiotic was prescribed to all participants in order to control and neutralize the effect of these factors on the study results. Moreover, no significant differences were found in fracture type, etiology, surgical approach and duration (Table 1).
This study was conducted due to the increasing incidence and prevalence of maxillofacial injuries and fractures worldwide and especially in Syria [41,42]. This necessitated finding easy, inexpensive and safe ways to speed up bone healing. The results showed that there were statistically significant differences in the gray scale values of the fracture line after two months and after four months between the two study groups. Moreover, significant differences were found in fracture union after four months between the two groups. These results indicate a positive effect of local administration of simvastatin (10 mg) in accelerating the healing of mandibular fractures.
Here, we agree with a previous randomized clinical study concluding that the application of 10mg simvastatin via gelatin sponge has a positive effect in the healing of periapical lesions [43]. The results were also in line with Degala and Bathija, et al. who conducted a splitmouth randomized clinical trial, and found that local application of simvastatin was effective in stimulating and accelerating bone regeneration after surgical extraction of impacted third molars [13]. Furthermore, Saifi, et al. found that simvastatin promoted healing of premolar extraction sockets [24]. This, to our knowledge, is the first clinical study showing the effect of topical simvastatin application on mandibular fractures healing.
This study had few methodological limitations. First, complete investigator blinding was not possible because simvastatin-loaded gelatin sponge can easily be detected by the surgical team during surgery. However, this trial was partially blinded via patient and statistician blinding to reduce risk of bias. Also, many patients with mandibular fractures could not be included in this study as shown in the flow chart. Those mainly had war-related injuries and comminuted fractures that were left out of the study eligibility criteria. Thus, our results may not necessarily be generalizable to all types of mandibular fractures.
Conclusion
Within the limitation of this study, it seems that local delivery and sustained release of simvastatin along the fracture line may hasten the bone healing in mandibular fractures.
References
- Rashid S, Kundi JA, Sarfaraz A, et al. Patterns of mandibular fractures and associated comorbidities in Peshawar, Khyber Pakhtunkhwa. Cureus 2019; 11.
- Barde D, Mudhol A, Madan R. Prevalence and pattern of mandibular fracture in Central India. Natl J Maxillofac Surg 2014; 5:153-156.
- Dell' Aversana Orabona G, Iaconetta G, Abbate V, et al. Bifocal mandibular fractures: Which should be treated first? J Craniofac Surg 2012; 23:1723-1727.
- Jha SG, Sinha V, Samanth TU, et al. Management of mandible fracture by plating and wiring: An otolaryngologist perspective at teritiary care center. Indian J Otolaryngol Head Neck Surg 2019; 71:417-424.
- Hong H, Song T, Liu Y, et al. The effectiveness and safety of parathyroid hormone in fracture healing: A meta-analysis. Clinics 2019; 74:e800.
- Heyer FL, de Jong JJ, Willems PC, et al. The effect of bolus Vitamin D3 supplementation on distal radius fracture healing: A randomized controlled trial using HR-pQCT. J Bone Miner Res 2021; 36:1492-1501.
- Einhorn TA, Gerstenfeld LC. Fracture healing: Mechanisms and interventions. Nat Rev Rheumatol 2015; 11:45-54.
- Buettner MF, Wolkenhauer D. Hyperbaric oxygen therapy in the treatment of open fractures and crush injuries. Emerg Med Clin North Am 2007; 25:177-188.
- FaÃ?bender M, Minkwitz S, Strobel C, et al. Stimulation of bone healing by sustained bone morphogenetic protein 2 (BMP-2) delivery. Int J Mol Sci 2014; 15:8539.
- Rosselli JE, Martins DM, Martins JL, et al. The effect of simvastatin on the regeneration of surgical cavities in the femurs of rabbits. Acta Cir Bras 2014; 29:87-92.
- Maeda T, Matsunuma A, Kurahashi I, et al. Induction of osteoblast differentiation indices by statins in MC3T3-E1 cells. J Cell Biochem 2004; 92:458-471.
- Halloran D, Durbano HW, Nohe A. Bone morphogenetic protein-2 in development and bone homeostasis. J Dev Biol 2020; 8:19.
- Degala S, Bathija NA. Evaluation of the efficacy of simvastatin in bone regeneration after surgical removal of bilaterally impacted third molars-A split-mouth randomized clinical trial. J Oral Maxillofac Surg 2018; 76:1847-1858.
- Kawai T, Murakami S, Hiranuma H, et al. Radiographic changes during bone healing after mandibular fractures. Br J Oral Maxillofac Surg 1997; 35:312-318.
- Street J, Bao M, deGuzman L, et al. Vascular endothelial growth factor stimulates bone repair by promoting angiogenesis and bone turnover. Proc Natl Acad Sci 2002; 99:9656-9661.
- Young S, Patel ZS, Kretlow JD, et al. Dose effect of dual delivery of vascular endothelial growth factor and bone morphogenetic protein-2 on bone regeneration in a rat critical-size defect model. Tissue Eng 2009; 15:2347-2362.
- Patel ZS, Young S, Tabata Y, et al. Dual delivery of an angiogenic and an osteogenic growth factor for bone regeneration in a critical size defect model. Bone 2008; 43:931-40.
- Shah SR, Werlang CA, Kasper FK, et al. Novel applications of statins for bone regeneration. Natl Sci Rev 2015; 2:85-99.
- Moshiri A, Sharifi AM, Oryan A. Role of simvastatin on fracture healing and osteoporosis: A systematic review on in vivo investigations. Clin Exp Pharmacol Physiol 2016; 43:659-684.
- Jadhav SB, Jain GK. Statins and osteoporosis: new role for old drugs. J Pharm Pharmacol. 2006; 58(1):3-18. doi: 10.1211/jpp.58.1.0002
- Zhang J, Wang H, Shi J, et al. Combination of simvastatin, calcium silicate/gypsum, and gelatin and bone regeneration in rabbit calvarial defects. Sci Rep 2016; 6:23422.
- Gutierrez GE, Lalka D, Garrett IR, et al. Transdermal application of lovastatin to rats causes profound increases in bone formation and plasma concentrations. Osteoporos Int 2006; 17:1033-1042.
- Castillo-Cardiel G, López-Echaury AC, Saucedo-Ortiz JA, et al. Bone regeneration in mandibular fractures after the application of autologous mesenchymal stem cells, a randomized clinical trial. Dent Traumatol 2017; 33:38-44.
- Saifi AM, Giraddi GB, Ahmed N. Healing of extraction socket following local application of simvastatin: A split mouth prospective study. J Oral Biol Craniofac Res 2017; 7:106-112.
- Ozeç I, Kiliç E, Gümüs C, et al. Effect of local simvastatin application on mandibular defects. J Craniofac Surg 2007; 18:546.
- Wong RW, Rabie AB. Early healing pattern of statin-induced osteogenesis. Br J Oral Maxillofac Surg 2005; 43:46-50.
- Lee Y, Schmid MJ, Marx DB, et al. The effect of local simvastatin delivery strategies on mandibular bone formation in vivo. Biomaterials 2008; 29:1940-1949.
- Tai IC, Fu YC, Wang CK, et al. Local delivery of controlled-release simvastatin/PLGA/HAp microspheres enhances bone repair. Int J Nanomed 2013; 8:3895-904.
- Stein D, Lee Y, Schmid MJ, et al. Local simvastatin effects on mandibular bone growth and inflammation. J Periodontol 2005; Â 76:1861-70.
- Fuster-Torres MÃ, Peñarrocha-Diago M, Peñarrocha-Oltra D, et al. Relationships between bone density values from cone beam computed tomography, maximum insertion torque, and resonance frequency analysis at implant placement: A pilot study. Int J Oral Maxillofac Implants 2011; 26:1051-1056.
- Albassal A, Al-Khanati NM, Harfouch M. Could a digital panoramic X-ray not detect a displaced fracture of the mandible?. Quant Imaging Med Surg 2021; 11:3890-3892.
- Albassal A, Al-Khanati NM, Harfouch M. Traumatic genial tubercle fracture: A case description with 9-month radiographic follow-up and a literature analysis. Quant Imaging Med Surg 2021; 12:2579.
- Al-Zahrani MS, Elfirt EY, Al-Ahmari MM, et al. Comparison of cone beam computed tomography-derived alveolar bone density between subjects with and without aggressive periodontitis. J Clin Diagn Res 2017; 11:ZC118-ZC121.
- Pauwels R, Jacobs R, Singer SR, et al. CBCT-based bone quality assessment: are Hounsfield units applicable? Dentomaxillofac Radiol 2015; 44:20140238.
- Cassetta M, Stefanelli LV, Pacifici A, et al. How accurate is CBCT in measuring bone density? A comparative CBCT-CT in vitro study. Clin Implant Dent Relat Res 2014; 16:471-478.
- Parsa A, Ibrahim N, Hassan B, et al. Bone quality evaluation at dental implant site using multislice CT, micro-CT, and cone beam CT. Clin Oral Implants Res 2015; 26:e1-7.
- Reeves TE, Mah P, McDavid WD. Deriving Hounsfield units using grey levels in cone beam CT: A clinical application. Dentomaxillofac Radiol 2012; 41:500-508.
- Bastami F, Shahab S, Parsa A, et al. Can gray values derived from CT and cone beam CT estimate new bone formation? An in vivo study. Oral Maxillofac Surg 2018; 22:13-20.
- Al-Khanati NM, Al-Moudallal Y. Effect of intrasocket application of manuka honey on postsurgical pain of impacted mandibular third molars surgery: Split-mouth randomized controlled trial. J Maxillofac Oral Surg 2019; 18:147-152.
- Hassan B, Al-Khanati NM, Bahhah H. Effect of lingual-based flap design on postoperative pain of impacted mandibular third molar surgery: Split-mouth randomized clinical trial. Med Oral Patol Oral Cir Bucal 2020; 25:e660-e667.
- Hamzeh A, Ayoub R, Issa S, et al. War-related ocular injuries in Damascus during the Syrian crisis. Injury 2021; 52:299-304.
- Wu J, Min A, Wang W, et al. Trends in the incidence, prevalence and years lived with disability of facial fracture at global, regional and national levels from 1990 to 2017. Peer J 2021; 9:e10693.
- Gupta S, Verma P, Tikku AP, et al. Effect of local application of simvastatin in bone regeneration of peri-apical defects-a clinico-radiographic study. J Oral Biol Craniofac Res 2020; 10:583-591.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Ahmad Albassal1, Nuraldeen Maher Al-Khanati1,2* and Munir Harfouch1
1Department of Oral and Maxillofacial Surgery, Faculty of Dental Medicine, Damascus University, Damascus, Syria2Department of Oral and Maxillofacial Surgery, Faculty of Dentistry, Syrian Private University, Damascus, Syria
Received: 29-Aug-2022, Manuscript No. jrmds-22-52818; , Pre QC No. jrmds-22-52818(PQ); Editor assigned: 31-Aug-2022, Pre QC No. jrmds-22-52818(PQ); Reviewed: 15-Sep-2022, QC No. jrmds-22-52818(Q); Revised: 19-Sep-2022, Manuscript No. jrmds-22-52818(R); Published: 26-Sep-2022
