Research - (2022) Volume 10, Issue 2
Direct Trocar Insertion without Previous Pneumoperitoneum in Laparoscopic Surgery
BushraTasneem1*, Aisha Tasneem1, Rahila Imtiaz2, Aqsa Ismail1, Nida Ahmed3, Iqra Mustaqeem1, Ahsan Ali Siddiqui4 and Sana Bilar5
*Correspondence: BushraTasneem, Department of Surgery, Abbasi Shaheed Hospital Karachi, Pakistan, Email:
Abstract
Objectives: The purpose of this study was to assess the safety, feasibility, benefits and risks of direct trocar insertion (DTI) in various laparoscopic procedures without previous Pneumoperitoneum Methodology: This prospective observational study was conducted at the department of surgery Abbasi Shaheed Hospital Karachi June 2015 to June 2021. Patients that underwent various laparoscopic procedures and admitted through OPD and emergency were included. All patients of either gender in-between 15 to 70 years, undergoing any laparoscopic surgery were included having direct trocar insertion (DTI) without any previous pneumoperitoneum. Patients with history of surgeries or current abdominal tuberculosis, appendicular lump, peritonitis, unfit for anesthesia (ASA III or above) or any systemic disease were excluded. SPSS version 23.0 was used for data analysis. For qualitative data, frequency and percentages were reported whilst for quantitative data, mean and standard deviation was recorded Results: From total of 1913 patients, 1900 underwent laparoscopic cholecystectomy, 08 laparoscopic appendectomies while 05 patients had undergone laparoscopic ovarian cystectomy. 1668 (87.2%) patients were females while 245 (12.8%) were males.DTI was found to be successful in all 100% of patients without any intra-abdominal or visceral injuries either major or minor. No leakage of gas was reported in any patient. 27 (1.4%) patients were reported to develop abdominal wall haemorrhage while 36 (1.9%) patients developed wound infection. Conclusion: This study suggests that DTI is a faster, safer and more reliable alternative to the traditional technique for establishment of pneumoperitoneum and should be used routinely.
Keywords
Direct Trocar Insertion, Laparoscopic entry, Pneumoperitoneum, Laparoscopy
Introduction
Prior to entry of trocar, a successfully established pneumoperitoneum is usually termed as the initial step in laparoscopy. Rationale for pneumoperitoneum to be adequate is the provision of buffer space in-between site of insertion and abdominal or pelvic viscera [1]. Nonetheless, current data suggests that a substantial number of complications are associated with laparoscopy assisted Veress needle insufflation, for instance subcutaneous or sub-fascial insufflation, gas embolism, bowel or visceral insufflation and failure of pneumoperitoneum resulting in failure of laparoscopy [2].
Initially, Dingfelder demonstrated the technique for direct trocar insertion and termed it as both safe and effective laparoscopic technique. It was thought that elevation of abdominal wall was the most important factor in attaining safety regardless of the technique used, which was ideally accomplished without establishment of pneumoperitoneum [3]. Studies have described the use of this technique successfully with only mild/easily manageable complications. A research even preferred direction trocar insertion/placement since it reported minimal and minor complications only with lesser time for operating. This modality has now become an increasingly popular technique in many of the health care institutions all over the globe [4].
Even then at present, many hospitals use the conventional methods for majority of laparoscopic surgeries with the establishing of pneumoperitoneum prior to the entry of trocar. However, many surgeons recommend switching from conventional techniques towards insertion of trocar directly without establishing pneumoperitoneum [5].
Since the use of laparoscopic surgery have been the preferred mode of abdominal surgeries as they are associated to improved cosmetic results and fewer complications in relation to patient’s sufferings and morbidity. The use of DTI as opposed to other methods for establishing pneumoperitoneum was initially reported by Dingfelder [6]. Even though DTI is a blind technique but it has decreased number of blind steps. Although complications following laparoscopic surgeries are uncommon, yet majority (almost half) of the observed complications occur during pneumoperitoneum creation, i.e. in gaining access into the abdominal cavity [7].
Entry-related injuries/complications to the abdomen include gastrointestinal tract perforation, sub-cutaneous emphysema, major or minor vessel injury, all of which occur amid creation of pneumoperitoneum [8]. For this reason, DTI as opposed to conventional or traditional methods have been increasingly being used for minimizing such entry-related injuries [9]. The rationale behind use of DTI without previous pneumoperitoneum over other techniques is on the basis of difficulty to grasp and lift abdomen after distention with gas and it accounts for various complications. Multiple researchers have recommended the use of initial trocar insertion to be the most important and dangerous aspect in the use of trocars and probably the most difficult step throughout minimally invasive surgeries [10].
The purpose of this study was to assess the safety, feasibility, benefits and risks of direct trocar insertion (DTI) in various laparoscopic procedures without previous Pneumoperitoneum.
Material and Methods
This prospective observational study was conducted at the department of surgery at Abbasi Shaheed Hospital Karachi for a period of 6 years from June 2015 to June 2021. A total of 1913 patients were included in the study that underwent various laparoscopic procedures and were admitted through the Out-Patient Department (OPD) and emergency while ovarian cyst patients were taken from the Gyne Ward. In all of the patients, a direct trocar insertion (DTI) was carried out at the level of umbilicus, without any previous pneumoperitoneum.
All patients of either gender in-between 15 to 70 years of age, of any body mass index (BMI obese or thin, undergoing any laparoscopic surgery such as laparoscopic cholecystectomy, laparoscopic appendectomy, laparoscopic ovarian cystectomy etc. were included in the study having direct trocar insertion (DTI) without any previous pneumoperitoneum.
Patients with a history of previous surgeries or having surgery above the level of umbilicus, history or current abdominal tuberculosis, appendicular lump, peritonitis were excluded from the study. In addition patients unfit for anesthesia (ASA III or above) or any systemic disease such as chronic obstructive pulmonary disease (COPD), ischemic heart disease (IHD) and coagulation problems were also excluded from the study.
Data analysis
For data analysis, SPSS version 23.0 was used. For qualitative data, frequency and percentages were reported whilst for quantitative data, mean and standard deviation was recorded.
Results
From the total of 1913 patients included in the study, 1900 patients underwent laparoscopic cholecystectomy, 08 patients underwent laparoscopic appendectomy while 05 patients had undergone laparoscopic ovarian cystectomy (Table 1).
| Type of laparoscopy | Frequency (%) |
|---|---|
| Laparoscopic cholecystectomy | 1900 (99.3) |
| Laparoscopic appendectomy | 08 (0.42) |
| Laparoscopic ovarian cystectomy | 05 (0.26) |
Table 1: Type of laparoscopy patients included in the study (n=1913).
The age range of patients was in-between 15 to 70 years of age with 49 (2.6%) patients between 15-20 years of age, 241 (12.6%) patients between 21-29 years of age, 515 (27%) patients were between 31-39 years of age, 470 (24.6%) of patients were between 41-49 years of age, 402 (21%) patients were between 51-59 years of age while 229 (12%) patients were in-between 61-70 years of age (Figure 1).
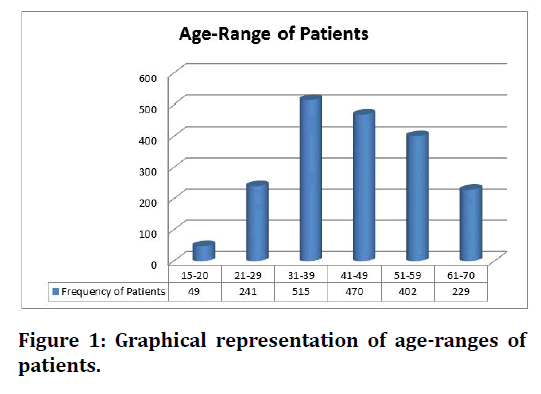
Figure 1. Graphical representation of age-ranges of patients.
From the total patients, 1668 (87.2%) patients were females while 245 (12.8%) patients were males (Figure 2).
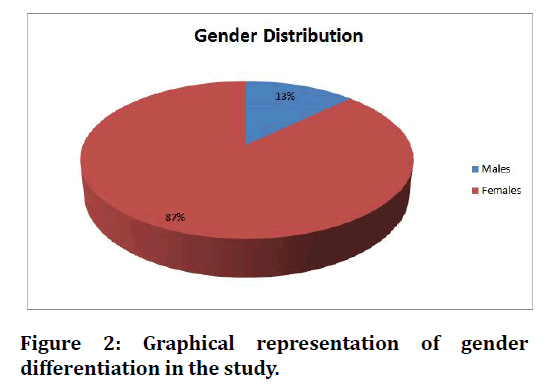
Figure 2. Graphical representation of gender differentiation in the study.
DTI was found to be successful in all 100% of patients without any intra-abdominal or visceral injuries either major or minor. No leakage of gas was reported in any patient. 27 (1.4%) patients were reported to develop abdominal wall hemorrhage while 36 (1.9%) patients developed wound infection (Table 2).
| Complications | Frequency (%) |
|---|---|
| Wound Infection | 36 (1.9) |
| Abdominal Wall Hemorrhage | 27 (1.4) |
| Visceral Injury | Nil |
| Vascular Injury | Nil |
| Gas Leak | Nil |
Table 2: Frequency of complications in patient’s undergoing laparoscopic surgery.
Discussion
The results of this study showed that DTI without previous pneumoperitoneum was highly successful in all the patients wherein from 1913 patients, only 36 (1.9%) patients developed wound infection while 27 (1.4%) developed abdominal wall hemorrhage. Majority of the patients, i.e. 87% were females. Most patients were inbetween the ages of 31-39 (515, 27%).
In accordance with our study, various researchers have reported that DTI without previous pneumoperitoneum was highly successfully in patients undergoing laparoscopic surgeries [10]. Likewise, the mean age of patients in one of the study was similar to most of patients included in our study with the same age group (32 ± 1.9 years) [11].
In one of the studies byPantoja-Garrido et al. who compared the use of direct trocar insertion (DTI) without previous pneumoperitoneum against insertion postinsufflation using Veress needle in laparoscopic abdominal surgeries, it was concluded by the results of the study that DTI was a much safer alternate against traditional technique for abdominal laparoscopic surgeries [12].
Use of DTI for direct entry technique has been employed for young, old, obese, non-obese and non-virginal or virginal abdominal surgeries. One of the study reported DTI to be safer in obese patients, being safer and quicker than classical techniques [13]. DTI has been termed as the fastest abdominal entry method. A research reported post-operative complications using DTI to range inbetween 0.2-10.3%, which is in line with our study were overall, 3.3% of patients were found to have a complication such as wound infection and abdominal wall hemorrhage [14]. Other studies have reported major complications in terms of injury to the bowel, major vessel, and urinary bladder and/ or anesthesia related complications because of raised intra-abdominal pressures, leading to aspiration and causing difficulty in patients’ ventilation. The minor complications included port site hernia and surgical wound infection [15]. In our research, one complication reported was major, i.e. abdominal wall hemorrhage while wound infection was termed as a minor complication.
In yet another research done by Choudhury et al. from the total of 175 laparoscopic surgeries undergoing DTI without any prior establishment of pneumoperitoneum observed no vascular or visceral complications in any of the patient [16]. In line with our study, a study by Ahmed et al reported no or minor complications following DTI for laparoscopic surgeries. The study also compared DTI with Veress needle entry, demonstrating three benefits of DTI over veress, i.e. less incidences of failed entry with DTI, extra peritoneal insufflation and omental injury [17].
In our study and majority of the studies as well, the main reason behind laparoscopic surgery related complications are linked to maneuvers of placement of trocars, both optical and accessory and insufflation. In a study similar to ours, DTI was regarded to be safe, efficient, rapid and easily-learned alternate method for reducing the frequency of laparoscopic procedure related complications [18].
In line with our study, another study by Ulusoy et al. done to examine the safety and efficiency of STI for creating pneumoperitoneum in laparoscopic surgery reported that in 1200 patients included in the research, only 4 patients were found to have skin hematoma and ecchymosis (bruising of the skin), while only 01 patient was observed to have abdominal wall haemorrhage. No other complications were seen in the research. The study concluded that laparoscopic surgeries that used DTI are safer and efficient in all patients, especially in those having no previous history of abdominal surgery [19].
Conclusion
This study suggests that DTI is a faster, safer and more reliable alternative to the traditional technique for establishment of pneumoperitoneum and should be used routinely.
References
- Kaistha S, Kumar A, Gangavatiker R, et al. Laparoscopic access: Direct trocar insertion versus open technique. J Laparoendosc Adv Surg Tech 2019; 29:489-94.
- Godara R, Bansal AR, Verma S, et al. Direct trocar insertion without the pneumoperitoneum in laparoscopic surgery-Is this a safe technique?. Hellenic J Surg 2015; 87:415-418.
- Kumar R, Hastir A, Bandlish MK. Pneumoperitoneum by direct trocar insertion: Safe laparoscopic access. J Evol Med Dent Sci 2015; 4:2432-8.
- Tariq M, Ahmed R, Rehman S, et al. Comparison of direct trocar insertion with other techniques for laparoscopy. J Coll Physicians Surg Pak 2016; 26:917-919.
- Hameed F, Iqbal MS, Iqbal Z, et al. Safety of direct trocar insertion for laparoscopic procedures. Ann Punjab Med Col 2018; 12:211-214.
- Abdullah Shoeb Mansuri D, Talreja M, Anis M, et al. A prospective study of direct trocar entry versus veress needle entry for laparoscopic surgery. Int J Surg 2021; 5:293-296.
- Abdullah AA, Abdulmageed MU, Katoof FM. The efficacy of direct trocar versus veress needle method as a primary access technique in laparoscopic cholecystectomy. Mustansiriya Med J 2019; 18:47-50.
- Mushtaq U, Naikoo GM, Gilkar IA, et al. Classical closed technique by veress needle insertion versus direct trocar insertion in the creation of pneumoperitoneum in various laparoscopic surgeries. J Contemporary Med Res 2019; 6:9-13.
- Choudhry ZA, Iqbal MS, Latif M, et al. Comparison of direct trocar versus veress needle insertion in creation of pneumoperitoneum in patients undergoing laparoscopic cholecystectomy. Ann Punjab Med Coll 2019; 13:126-129.
- Vilos GA, Ternamian A, Vilos AG, et al. Direct laparoscopic trocar insertion: Lessons learned from nine litigated cases. J Minim Invasive Gynecol 2017; 24:960-70.
- Dwedar AE, Taher Ismail M, et al. Direct trocar insertion in gynecological laparoscopy: A case series of 300 cases. Al-Azhar Med J 2021; 50:1921-32.
- Pantoja-Garrido M, Frías Sánchez Z, Zapardiel Gutiérrez I, et al. Direct trocar insertion without previous pneumoperitoneum versus insertion after insufflation with Veress needle in laparoscopic gynecological surgery: A prospective cohort study. J Obstetr Gynaecol 2019; 39:1000-1005.
- Ertugrul I, Kayaalp C, Yagci MA, et al. Comparison of direct trocar entry and Veress needle entry in laparoscopic bariatric surgery: Randomized controlled trial. J Laparoendosc Adv Surg Tech 2015; 25:875-879.
- Abass MO, Elssayed EO, Mhammed AB. Laparoscopic access techniques: Experience in a developing country, Sudan. J Surg 2020; 8:109-113.
- Cornette B, Berrevoet F. Trocar injuries in laparoscopy: Techniques, tools, and means for prevention. A systematic review of the literature. World J Surg 2016; 40:2331-2341.
- Choudhury DK, Kaman A. Direct trocar entry technique: A safe method of primary trocar entry in laparoscopic surgery. J Dent Med Sci 2017; 16:38-40.
- Ahmad G, Baker J, Finnerty J, et al. Laparoscopic entry techniques. Cochrane Database Sys Rev 2019; 146.
- Nouri B, Amini FG, Arab M, et al. Comparison of the outcomes of direct trocar insertion with modified open entry in laparoscopic surgery. Indian J Gynecol Oncol 2021; 19:1-5.
- Ulusoy S, Özer M, Kilinç İ, et al. Direct trocar entry for laparoscopy safety and efficiency. Laparosc Endosc Surg Sci 2018; 25:64-66.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
BushraTasneem1*, Aisha Tasneem1, Rahila Imtiaz2, Aqsa Ismail1, Nida Ahmed3, Iqra Mustaqeem1, Ahsan Ali Siddiqui4 and Sana Bilar5
1Department of Surgery, Abbasi Shaheed Hospital Karachi, Pakistan2Department of Gynaecology, Abbasi Shaheed Hospital, Karachi, Pakistan
3Senior Registrar Surgery, Karachi Institute of Medical Sciences, Pakistan
4Specialist Family Medicine, Ministry of Health, Riyadh, Saudi Arabia
5Specialist Family Medicine, Sulaiman Alhabib Hospital, Pakistan
Received: 01-Feb-2022, Manuscript No. JRMDS-22-53016; , Pre QC No. JRMDS-22-53016 (PQ); Editor assigned: 03-Feb-2022, Pre QC No. JRMDS-22-53016 (PQ); Reviewed: 17-Feb-2022, QC No. JRMDS-22-53016; Revised: 21-Feb-2022, Manuscript No. JRMDS-22-53016 (R); Published: 28-Feb-2022
