Case Report - (2022) Volume 10, Issue 4
Diffuse Neurofibroma: The Pugnacious Scalp Tumor Identified by the Histopathological Exam and Role of Expander for Diseased-Free Margins: A Case Report
Muhammad Usman, Ying Cen and Ai Zhong
*Correspondence: Junjie Chen, Department of Plastic Surgery, West China School of medicine, West China Hospital, Sichuan University, China, Email:
Abstract
The diffuse neurofibroma is the inherited and rarest variation of Neurofibroma. The Diffuse neurofibroma is commonly found in children and adolescents. The tumor can develop anywhere in the peripheral nervous system and cranial nerves. Diffuse neurofibroma is highly infiltrative with inadequate borders; tumor most likely affects body part such as the head and neck. We have presented the case of a nine-year-old boy who suffered head pain and discomfort for years. He appeared to our plastic surgery department and is accompanied by an obvious tumor on the back of his scalp. MRI revealed a large mass on the scalp. An incisional biopsy was performed and based on histopathological findings; diffuse neurofibroma was diagnosed after clinical and laboratory observation in brief. The treatment included a two-step step technique, and in the first step the tissue expander implantation was done, and in the second step the surgical excision of the tumor. The patient is asymptomatic after 3 years. This is a rare variant that must be distinguished from other types of neurofibroma to prompt treatment and management. Furthermore, our case report the deep understanding of the guideline and management by providing clinical evidence of the utility of histopathological analysis and which give plastic surgeons in smaller settings a serious warning to follow the proper guideline.Keywords
Diagnosis of diffuse neurofibromas, Histopathology, Tissue expander, Surgery technique
Introduction
Diffuse neurofibroma is a subtype of neurofibroma, which is characteristically separated from its other types of neurofibroma and is inherited and uncommon. Diffuse neurofibroma arises from the neural sheath and it is distinguished by Schwann cell, perineural cell, and endoneurial fibroblast proliferation. This is an autosomal dominant pattern disease with multiple penetrance’s’ that can be traced along with the peripheral nervous system and cranial nerves. In children, the tumor might be either firm or soft. Tumors severely affect the skin and underlying subcutaneous of the head. The relationship between diffuse neurofibroma and neurofibromatosis is not well established, but there is the hypothesis that patients with diffuse neurofibroma tend to develop neurofibromatosis. We present a case report of a young boy suffering from diffuse neurofibroma on his scalp and diagnosis was verified by MRI and histopathological results. This case study may have significant implications for following guidelines and clinical management, as well as the important role of diffuse neurofibroma histopathological findings in accurate diagnosis.
Case Presentation
A 9-year-old child presented at our out-patient clinic of the Plastic surgery department of West China Hospital; he was complaining of scalp swelling for two years. The patient went to the local community hospital, where the scalp protuberance was observed, and mass was 4 Χ 5 cm in size. The tumor was managed with home remedies without any medical therapy for two years before it start to grow larger, and the patient and his family were quite concerned about the unexpected shift in its size. There was occasionally discomfort at the site of tumor, and head and neck pain. In July 2016, the family visited the Panzhihua city center hospital where the patient has been thoroughly investigated and suggested hemangioma as a first-line diagnosis without further clinical investigation, and left untreated later on was referred to our hospital. Moreover, it was an indurated, ill-defined lesion with thicker skin, and a discrete asymmetry in head circumference was noted during a physical evaluation and the primary diagnostic assumption was a diffuse hemangioma. At our hospital, MRI and CT scans revealed a lesion emanating from the soft tissue but not involving the periosteum. However, a diagnostic test was performed; a biopsy through an incision was done. The specimen showed substantial infiltration of elongated cells and nuclei, the cytoplasm was light and eosinophilic mixed with nerve fiber, and many mast cells, brief observation and these characteristics suggest that the ultimate diagnosis is diffuse neurofibroma. The psychological stability of the patient as well as the temporary aesthetic deformity caused by the enlarged balloon was discussed with the parents. They were clear about this issue and were willing to go through the complete procedure. After considering the measurements of the lesion and expander's size, shape, and volume, and donor site, two 18 x 12 x 2cm long rectangular tissue expanders were selected. The incision for inserting the expander had been planned. Hence, the incision was approximate to the lesion where it was the cutting edge of the advanced flap. Surgery was completed in a two-step technique, and it was safe and secure. The tumor hasn’t grown to date (Figures 1 to Figure 3).
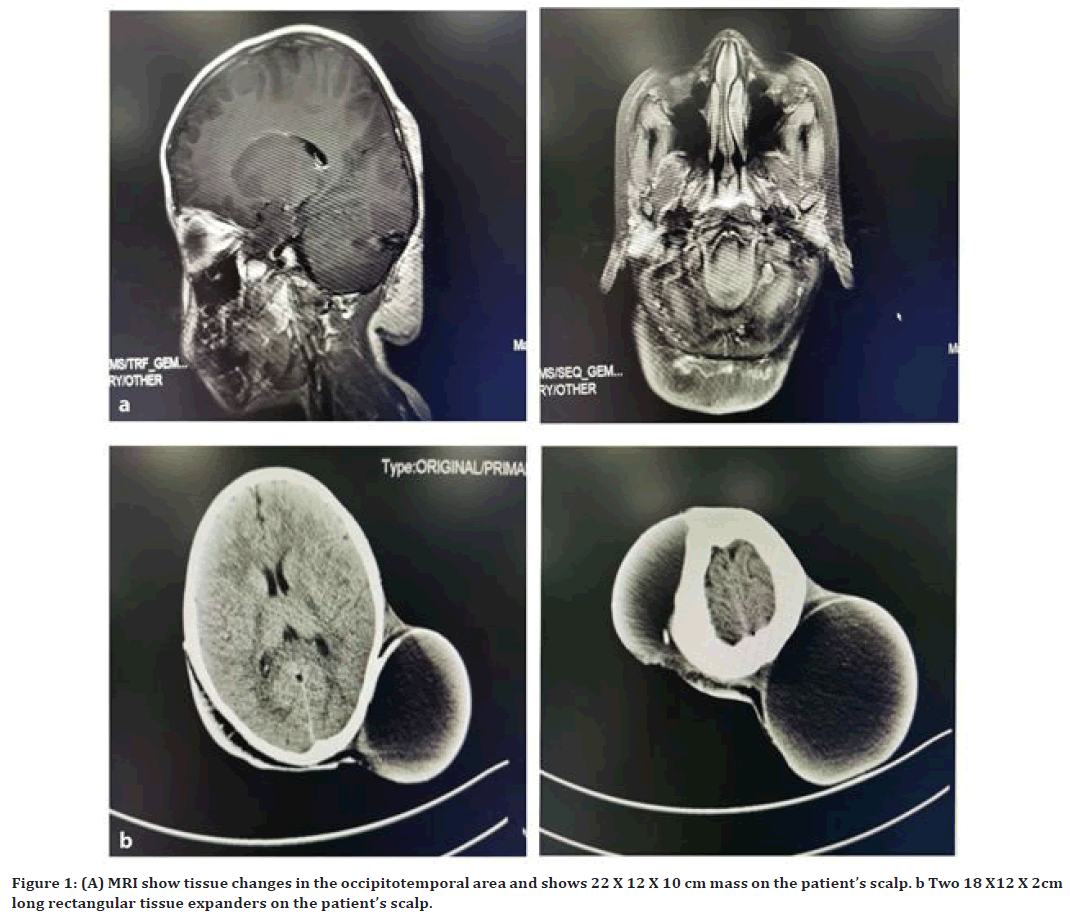
Figure 1. (A) MRI show tissue changes in the occipitotemporal area and shows 22 X 12 X 10 cm mass on the patient’s scalp. b Two 18 X12 X 2cm long rectangular tissue expanders on the patient’s scalp.
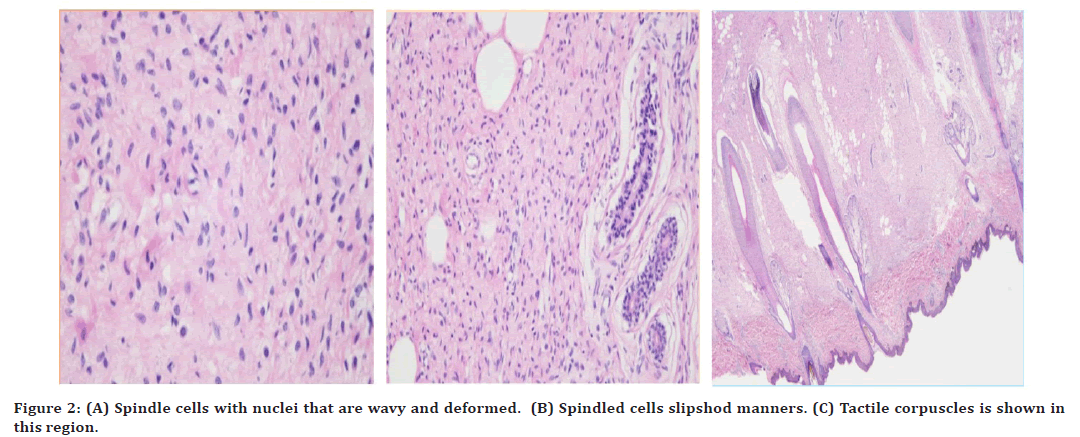
Figure 2. (A) Spindle cells with nuclei that are wavy and deformed. (B) Spindled cells slipshod manners. (C) Tactile corpuscles is shown in this region.
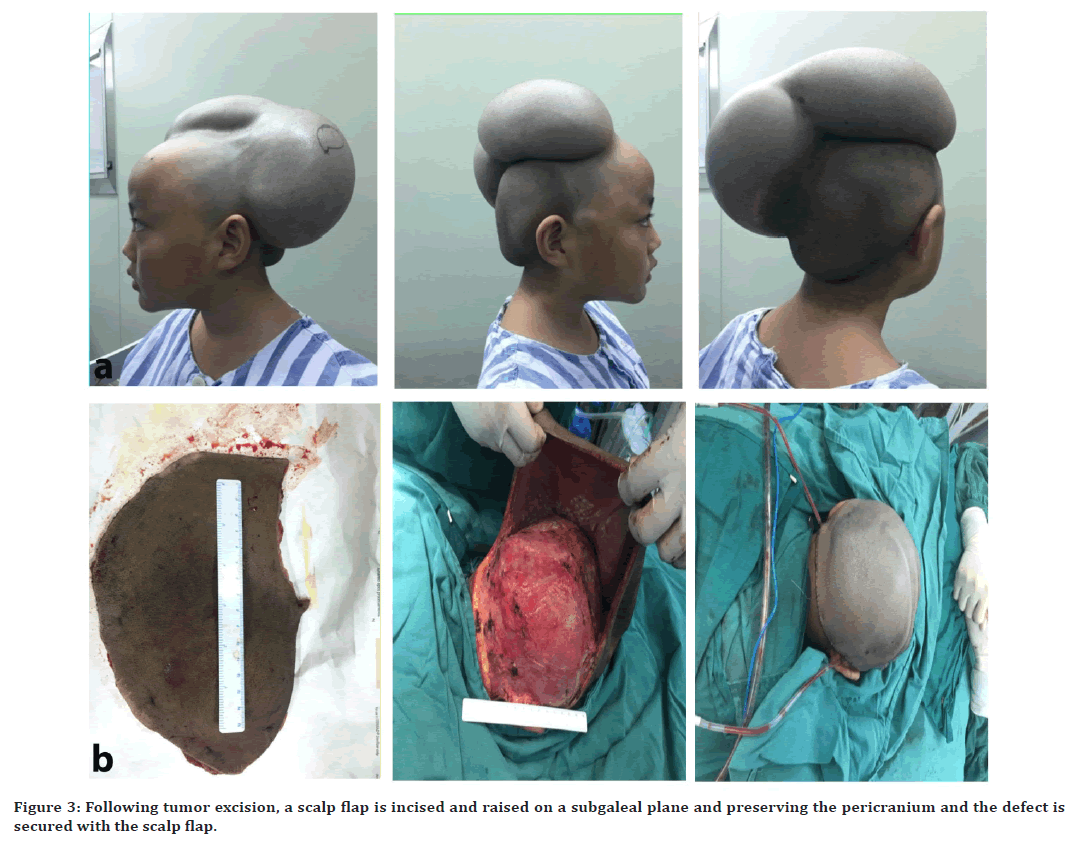
Figure 3. Following tumor excision, a scalp flap is incised and raised on a subgaleal plane and preserving the pericranium and the defect is secured with the scalp flap.
Discussion
This case study is significant for following the guidelines and clinical management, as well as here we can see the important role of diffuse neurofibroma histopathological results to make the accurate diagnosis. Findings from our study suggest that diagnosis of diffuse neurofibroma, like other tumors and/or other neurofibroma subtypes may be difficult to make on the basis of x-ray or just clinical manifestation and without histopathological examination. Neurofibromas are neuroectodermal tumors, arising from the peripheral nerve sheath and cranial nerves. The Schwann cells are a remarkable source of neurofibromas [1]. Diffuse neurofibroma is the most segregate and rare type of neurofibroma which makes diffuse neurofibroma fundamentally unpredictable for its progression, and we support the common belief that tumor involve the skin which facilitate its growth and in short time tumor gets huge mass as it is mentioned in previous literature findings. Lesions are distinguished with prominent skin enlargement, which commonly occurs on the head of children and young adults [1,2]. With its intrusion character, the lesion envelops instead of destroying the normal structure and functions. It is made up of longitudinal and spindly cells with the embezzled nucleus and cytoplasm containing abounding eosinophil’s that are surrounded by a network of collagen fiber. Structures such as Meissner are distinctive, but often not evident. The S-100 is not very significant apart from this slight discordance; the result is confirmation of S-100 protein marker expression in neurofibromatosis tissues, which is reliable for nerve sheath tumors [3]. It was found that diffuse neurofibroma rarely extends intracranial [1,4]. Delay in diagnosis may increase the risk of intracranial tumor. Even though 10% diffuse neurofibroma correlates NF-1, although malignant transformation is rare. Noteworthy, it was found in megahed’s results that show clear NF-1 was found in more than 61 percent of his patients [5]. Diffuse neurofibroma is considered as pathognomonic for neurofibromatosis type 1. Discomfort or uncontrolled growth of a neurofibroma should indicate malignancy mutation whereas patients suffering from diffuse neurofibroma don’t complain about pain. In contrast to his results the importance of malignant transformation cannot be stressed because a smaller number of NF-1 with diffuse neurofibromas has been found in the past literature, we believe that in younger patients, it is most unlikely to happen, and we shouldn’t ignore the possibility because the idea of diffuse neurofibromas mutation in NF-1 is uncommon [6]. Biopsy has an advantage over the additional imaging CT/MRI and this is in good agreement that MRI is the valuable tool for the diagnosis of diffuse neurofibroma because MRI results offer compelling evidence which supports to identifies the anatomical relationship between the surrounding tissues and neurofibroma. In most cases, MRI scans of a diffuse neurofibroma show a localized, distinct tumor with a dominant characteristic pattern [7]. Even though neurofibroma sometimes imitates a hemangioma, enclosed adipose tissue of diffuse neurofibroma mimicking the hemangioma [2]. This lends support to neurofibroma earlier research that found diffuse neurofibroma are mixed with fat cells as perineural fat tissue, may cause these tumors to resemble fat-containing tumors. Still we insist on the importance of histopathological examination which distinguishes types of neurofibroma and gives us solid proof to start the needed treatment. We started with MRI and carried out as biopsy, these satisfactory steps added values and correlate fairly well with our approach of treatment.
As expected, the tumor is adequately defined on histopathological analysis, substantial irregularities of border and infiltration into the subcutaneous layer of the scalp anticipated inaccurate diagnosis. Giant neurofibromas are treated surgically, either partially or completely. Clinically recurrence might develop though after full resection due to the infiltrative nature of the tumor, therefore a yearly check-up is advised due to the possibility of recurrence and the growth of neurofibromatosis [1,3]. Initially at the Panzhihua city center hospital doctors make the diagnosis on the basis of tumors appearance, why did they ignore the histopathological test and left the patient without a specific treatment is a question, maybe they misunderstood the nature of tumor or neglected the importance of histopathological test or they thought that clinical findings are enough to make the diagnosis, the reason whatever could be we must follow the guideline and protocols when we treat tumors. However, to classify diffuse neurofibroma as a primary disease any additional indications of hemangioma and neurofibromatosis type 1 must be ruled out. The biopsy is the best option for it. Careful analysis and closer inspection revealed that biopsy has far behind the impact on the diagnosis of the disease. In the current case, the findings show the deep infiltration which reach’s the pericranium. As proposed in literature the full excision of the diffuse neurofibroma was rarely successful without performing multiple debulking surgeries. In conclusion, the use of expanders allows us to repair the defect with well-vascularized tissue and remove potential pathogenic tissue as much as possible to avoid the recurrence and root out the disease once and for all. Most notably, the remarkable result that emerged from our study is that diffuse neurofibroma on a young boy's scalp can be removed in two-step surgeries, in the first step we inserted the tissue expanders, and in the second step, the total excision of the tumor is done and the defect is covered with the flap, without performing multiple surgeries and facing the insufficient normal skin tissue to cover the defect and with this technique disease-free margins are possible which are difficult to get without using a tissue expander. The clinical appearance leads to misdiagnosis of diffuse neurofibroma with hemangioma seems to be true in this case. However, considerable vigilance is required to achieve high results and solve the challenging shortage of required tissue to cover the defect and our experience is worth mentioning, in particular, diagnosis and increase the effectiveness of the treatment of the diffuse neurofibroma. We believe that our findings are appreciable and will help in clinical studies and further clinical investigation is needed for the effectiveness of tissue expanders, histopathological analysis and MRI of the diffuse neurofibroma. We completely agree to intend to increase diagnostic skills, tumor-free survival rates and solve the shortage and tumor free margins of tissue with expanders in patients, but also we believe in the first stage the primary focus should be on histopathological analysis and MRI for diagnosis and in the second stage on the issue of tissue shortage for the defect, if these steps are not accomplished, tumor recurrence and unacceptable surgery results are suspected. If these two key stages are developed in the treatment of diffuse neurofibroma will improve the clinical effectiveness and prevention of the tumor.
Funding
The Sichuan Science and Technology Program 2020YFS0267 provided funding for this research.
Reporting Checklist
The authors have completed the CARE reporting checklist.
Conflicts of Interest
The authors stated no conflicts of interest.
Ethical Statement
The authors accept full responsibility for the work, including ensuring that any concerns about the correctness and/or moral fiber of any of our work are thoroughly investigated and resolved.
References
- Daoud MS, Pittelkow MR. Lichen planus. In: Freedberg IM, Eisen AZ, Wolff K, et al. Fitzpatrick's dermatology in general medicine. 6th Edn. New York: McGraw-Hill, 2003; 463-477.
- Ito H, Akagi O, Nomura N, et al. Giant pigmented tumor of the scalp--a diffuse neurofibroma or a congenital naevus showing neurofibromatous changes? Immunohistochemical and electron microscopic studies. Histopathology 1988; 13:181-189.
- van Zuuren EJ, Posma AN. Diffuse neurofibroma on the lower back. J Am Acad Dermatol 2003; 48:938-940.
- Ergun SS, Emel E, Karabekir S, et al. Extracranial diffuse neurofibroma with intracranial extension. Plast Reconstr Surg 2000; 105:801-803.
- Beggs I, Gilmour HM, Davie RM. Diffuse neurofibroma of the ankle. Clin Radiol 1998; 53:755-759.
- Megahed M. Histopathological variants of neurofibroma. A study of 114 lesions. Am J Dermatopathol 1994; 16:486-495.
- Peh WC, Shek TW, Yip DK. Magnetic resonance imaging of subcutaneous diffuse neurofibroma. Br J Radiol 1997; 70:1180-1183.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Muhammad Usman, Ying Cen and Ai Zhong
1Department of Plastic Surgery, West China School of medicine, West China Hospital, Sichuan University, Chengdu, Sichuan Province, ChinaCitation: Muhammad Usman, Junjie Chen, Ying Cen, Ai Zhong, Diffuse Neurofibroma: The Pugnacious Scalp Tumor Identified by the Histopathological Exam and Role of Expander for Diseased-Free Margins: A Case Report, J Res Med Dent Sci, 2022, 10 (4):108-111.
Received: 01-Apr-2022, Manuscript No. JRMDS-22-60234; , Pre QC No. JRMDS-22-60234 (PQ); Editor assigned: 04-Apr-2022, Pre QC No. JRMDS-22-60234 (PQ); Reviewed: 18-Apr-2022, QC No. JRMDS-22-60234; Revised: 22-Apr-2022, Manuscript No. JRMDS-22-60234 (R);; Published: 29-Apr-2022
