Research - (2024) Volume 12, Issue 5
Malak AlOsaimi1*, Cristalle Soman1, Asma Almeslet1, Nader AlAmri2, Riyadh AlShaye2, Rawan AlHarbi3 and Tariq Wahass2
*Correspondence: Malak AlOsaimi, Maxillofacial Surgery and Diagnosis Sciences, College of Dentistry, Riyadh Elm University, Saudi Arabia, Email:
Abstract
The oral mucosa plays a crucial protective role as a natural barrier to exogenous substances and pathogens. Tobacco in any form, either smoked or smokeless, can cause a broad spectrum of oral mucosal alterations, ranging from harmless to more serious dysplastic and carcinomatous lesions. This study aimed to investigate the prevalence of Oral Mucosal Lesions (OMLs) in adult patients who do and do not use tobacco, their habits, and the relative risk of developing oral lesions associated with these habits.
Keywords
Oral mucosal lesions, Tobacco, Smoking, Precancerous lesions.
Introduction
The oral mucosa serves a vital function in providing protection by acting as a natural barrier against external chemicals and microorganisms. A wide range of lesions, varying in severity from benign to dysplastic and carcinomatous, can potentially impact these protective barriers. A consistent and methodical intraoral examination conducted by a dental professional can aid in the identification of the majority of these lesions during their early stages. It is important to intervene as early as possible, since this leads to more effective prevention against severe consequences. The excessive and frequent utilization of tobacco products is widely recognized as a significant risk factor associated with various changes in the oral cavity. These alterations encompass a broad spectrum, including heightened pigmentation and the thickening of the epithelium, which manifests as white lesions. The extent of these modifications exhibits significant variation based on the type of tobacco consumed (smoking or smokeless) as well as the frequency and length of tobacco usage. According to a survey published in 2013, the general prevalence of smoking in Saudi Arabia was documented to be 12.2% [1]. A prevalence rate of 21.4% (32.5% among males and 3.9% among females) was reported in a study conducted by the Saudi Food and Drug Authority. These findings suggest a rising trend and highlight significant public health concerns. The prevalence of smoking was found to be higher in the regions of Aljwaf, Northern Borders, Riyadh, and Eastern regions, as compared to the regions of Aseer, Jizan, and Albaha, which exhibited a lower prevalence of cigarette smokers [2]. Nevertheless, there is a dearth of epidemiological research on the prevalence and characteristics of Oral Mucosal Lesions (OMLs) and their association with tobacco product use and smoking practices in Saudi Arabia. A case-control study conducted within the Chennai population revealed that the frequency and dosage of tobacco consumption were identified as important risk factors for the development of lesions [3]. Furthermore, a high correlation was observed between smoking habits and the prevalence of oral potentially malignant disorders (OMLs) among smokers. There is a widely accepted consensus that the utilisation of tobacco, either on its own or in conjunction with alcohol consumption, is correlated with an elevated likelihood of developing oral cancer. Furthermore, this risk is shown to escalate in proportion to the frequency of exposure [4]. Furthermore, scholars have identified several oral mucosal lesions (OMLs) linked to tobacco consumption, including leukoplakia, smokeless keratosis, and oral submucosa fibrosis, some of which have the potential to develop into malignancies [5, 6]. Based on a recent survey that encompassed a representative sample of the entire nation, it was observed that the incidence of smoking in Saudi Arabia exhibited an upward trend, rising from 12.2% in 2013 to 21.4% in 2018. According to the cited source, the prevalence of smoking among males was 25.34%, while among females it was 1.91% [7]. In Saudi Arabia, cigarettes have been widely utilized as the predominant method of smoking. Consequently, there is a pressing need for clinical research to be conducted in order to establish fundamental information regarding the prevalence of oral lesions in the country [8]. Practitioners of preventive oral health care should endeavor to comprehend the incidence of these precursor lesions and intervene in their treatment prior to their progression into cancer. The purpose of this study was to examine the occurrence of Oral Mucosal Lesions (OMLs) in adult patients and its association with cigarette consumption (Table 1).
| TOBACCO | PRESENCE OF LESION | ||
|---|---|---|---|
| Tobacco | Pearson Correlation | I | |
| Sig. (2-tailed) | 0.397 | ||
| N | 136 | 0 | |
| Presence of Lesion | Pearson Correlation | .397" | 136 |
| Sig. (2-tailed) | 0 | I | |
| N | 136 | 136 | |
| ** Correlation is significant when P<0.01 (2-tailed). | |||
Table1: Comparison between the two included groups
Materials and Methods
The present study is a case-control descriptive clinical-pathological investigation conducted at three campuses of a private dental university in Riyadh, Kingdom of Saudi Arabia, over the period of June to August 2019. Prior to data collection, ethical approval was acquired from the Institutional Review Board of Riyadh Elm University (RC/IRB/2019/154). All participants provided written informed consent after being informed about the study, its objectives, and the potential benefits associated with their participation. The research activities described in this study were carried out in accordance with the ethical guidelines outlined in The Code of Ethics of the World Medical Association, specifically the principles outlined in the Helsinki Declaration (Table 2).
| TYPE OF EXPOSURE | TOBACCO EXPOSURE/DAY | DURATION IN YEARS | ||
|---|---|---|---|---|
| Type of exposure | Pearson | I | 350" | 654° |
| Correlation | ||||
| Sig. (2-tailed) | 000 | 000 | ||
| N | 136 | 136 | 136 | |
| Tobacco | Pearson | 350" | I | 548" |
| Exposure/day | Correlation | |||
| Sig. (2-tailed) | 0 | 0 | ||
| N | 136 | 136 | 136 | |
| Duration in years | Pearson | 654° | 548" | 1 |
| Correlation | ||||
| Sig. (2-tailed) | 0 | 000 | ||
| N | 136 | 136 | 136 |
Table2: The correlations between the type of tobacco exposure, daily exposure, and presence of lesions
Participants in this study ranged in age from 16 to 65 years old and had no prior medical conditions such as cardiovascular, endocrine, gastrointestinal, or respiratory diseases. They also had no history of alcohol consumption, no medications or drugs, and no previous oral lesions or tumors. Individuals who used tobacco were designated as the case group, which was further subdivided into two subgroups: smokers and those who smoked while being exposed to other forms of tobacco. The smoking group consisted of patients who engaged in cigarette use, while the second subgroup of individuals who utilized electronic cigarettes, hookah (also referred to as "Shishah" in Saudi Arabia), chewed tobacco, or consumed "Qat" (a local plant with a high nicotine content). The study examined the frequency, duration, and timing of cigarette consumption patterns. Frequency was operationally defined as the quantity of tobacco consumed by the patient on a daily basis, whereas length referred to the estimated period of time spanning from the initiation of tobacco use by the patient to the date of examination. Ultimately, the concept of time was operationalized as the duration, measured in minutes that the individual typically expended in consuming their allotted quantity of tobacco. The second primary cohort consisted of individuals in the control group who were healthy and did not use tobacco (Figure 1).
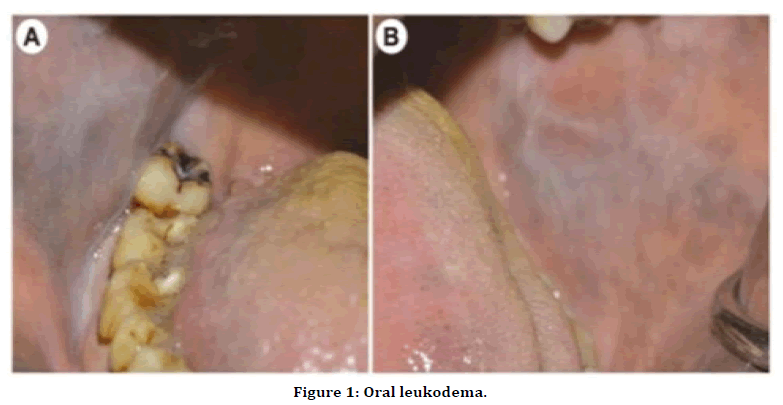
Figure 1. Oral leukodema.
Study tools
The case and control groups were examined by an oral diagnostic specialist. The patients were assessed using a screening examination, commencing with a standardized interview. Following this, the patients were visually assessed utilizing an artificial light source, mouth mirror, gauze, and WHO probe. The researchers methodically adhered to a structured sequence of examination for oral mucosal tissues, commencing with the examination of the lips, afterwards proceeding to the buccal mucosa and vestibules. The researchers then examined the four distinct regions of the tongue, namely the dorsal, ventral, left lateral and right lateral sides. They also investigated the floor of the mouth, the hard and soft palates, and the oropharynx. Lesions and conditions were documented during the examination. Furthermore, instances necessitating the use of scalpel biopsies were evaluated by a specialist in order to establish a conclusive histological diagnosis. The clinical diagnosis was determined using the criteria outlined [9].
Statistical analysis
All data were collected in paper form and transferred into a Microsoft Excel sheet (Microsoft, Inc. Redmond, WA). Statistical analyses were performed using the Statistical Package for the Social Sciences SPSS for Windows version 21 (SPSS, Inc. Chicago, IL). The threshold for statistical significance was set at < 0.05.
Results
A total of 136 people were enrolled in the study, with 68 in the case group and 68 in the control group. In terms of age, 49 percent of participants were between the ages of 16 and 25, 39 percent were between the ages of 25 and 40, and the remaining 20.5 percent were over 40. There was no significant age difference between tobacco users and non-users. 47 participants in the case group smoked only cigarettes, while 21 smoked cigarettes and had additional tobacco exposure (including cigarettes, shisha, tombak, shammah, gutkha, gat, and e-cigarettes). The most commonly detected OMLs were coated tongue (26.4%), followed by smoker’s melanosis (23.5%), fissured tongue (13.2%), Fordyce’s granules (13.2%), and linea alba (8.8%); other less detected OMLs accounted for 14.9%. Tobacco pouch keratosis observed (Figure 2). Only one case with a precancerous lesion was observed. Malignant lesions were not observed. The prevalence of OMLs was significantly higher among tobacco users than among non-users of tobacco. In the case group, the relationship between tobacco use and the presence of lesions was found to be statistically significant (p 0.00) The relationship between the type of tobacco used and the frequency of daily tobacco consumption was significant (p 0.00). Furthermore, the correlation between the type of exposure and tobacco exposure in years was highly significant (p 0.01). In the case group, the relationship between type of exposure and frequency was significant (p=0.02). There was no significant relationship between exposure type and exposure duration in years (p=0.063). A binomial logistic regression model with the presence or absence of oral lesions as the dependent variable and age, number of tobacco exposures, type of tobacco exposure, and duration as cofactors was developed. Individuals who had multiple types of tobacco exposure were significantly more likely to have an oral lesion than those who smoked cigarettes or did not smoke, according to the model. The number of tobacco exposures per day, years since the start of the habit, and age of the individual, on the other hand, were not associated with the presence of OMLs (Table 3).
| VARIABLES IN THE EQUATION | |||||||
|---|---|---|---|---|---|---|---|
| B | SE. | Wald | df | Sig. | Exp(B) | ||
| Step | Age | -.017 | .020 | .677 | 1 | .411 | .984 |
| I! | “TypeofTobacco exposure | 1.117 | .362 | 9.526 | 1 | .002* | 3.056 |
| Number of Exposures | .019 | .023 | .682 | 1 | .409 | 1.019 | |
| Years since commencement of habit | 0.024 | .042 | .333 | 1 | .564 | .976 | |
| Constant | 0.166 | .633 | .069 | 1 | .793 | .847 | |
Table 3: Factors affecting the presence or absence of mucosal lesions
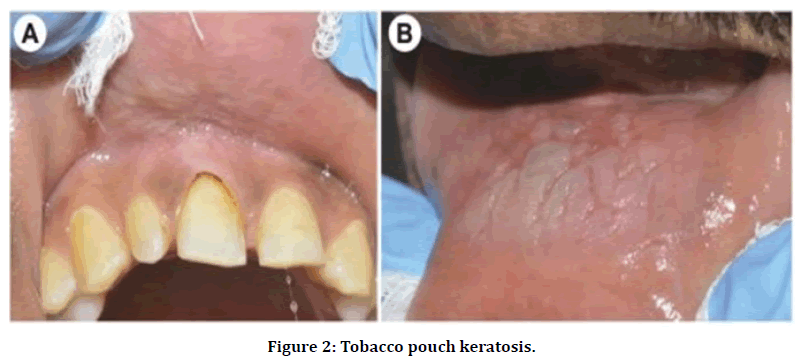
Figure 2. Tobacco pouch keratosis.
Discussion
Oral Mucosal Lesions (OMLs) have been linked to mortality; however, there is little information available about their prevalence in the Saudi population and their relationship with oral behaviours such as smoking. Oral mucosal lesions (OMLs) and oral mucosal illnesses are caused by a variety of etiological factors, including infections, systemic disorders, drugs, and risk factors such as cigarette, betel nut, and alcohol use. The utilization of tobacco has been found to have a positive correlation with the malignant alteration of tissues. The World Health Organization employs the phrase "potentially malignant lesions" to denote diseases that have the potential to develop into malignancies or precancerous states. These encompass OMLs that exhibit a higher propensity for undergoing malignant transformation. The occurrence of these lesions is prevalent among individuals who engage in cigarette consumption, and their potential transformation into malignant tumors can be mitigated through the implementation of thorough screening protocols, timely diagnosis, and suitable therapeutic interventions [10, 11]. The current case-control study was conducted at a privately owned dentistry university in Saudi Arabia with the goal of evaluating patients' Oral Potentially Malignant Lesions (OMLs) and malignant lesions that may be linked to tobacco consumption. The Saudi Ministry of Health launched the national tobacco control programme in 2002, in response to the Kingdom's 2005 membership in the World Health Organization's Framework Convention on Tobacco Control. OMLs were found in 70.5 percent of the cases and 30.8 percent of the controls, indicating a statistically significant difference. The prevalence of Oral Mucosal Lesions (OMLs) was found to be 50.6 percent on average in both groups, which is consistent with previous research findings (ranging from 58.8 percent to 61.6 percent). According to Martnez and Garca's 200-patient study, approximately 59 percent of patients had oral mucosal lesions. Among these lesions, melanin pigmentation was identified as the most commonly diagnosed form, followed by frictional keratosis, linea alba, cheek biting, and traumatic ulcer. The prevalence of stomatitis and hyperplasia was found to be highest among patients who utilized dentures [12]. It was found that 61% of the participants exhibited oral lesions of various types. The gender distribution of these lesions differed, with 37.8 percent of females and 62.5 percent of males affected. Betel nut chewer's mucosa (44 percent), leukoedema (6 percent), melanin pigmentation (8 percent), geographic tongue (16 percent), Fordyce's spots (8 percent), leukoplakia (6 percent), and fibroepithelial papilloma (8 percent) were the most commonly observed lesions [13]. Another study found a significant difference in the prevalence of tobacco-related lesions (namely leukoplakia and smoker's palate) between men and women, with men having a higher occurrence (p0.05). Lichen planus, denture stomatitis, and herpes labialis, on the other hand, were found to be more common in women. Furthermore, the current study found a significant link between the prevalence of oral mucosal lesions and a variety of factors, including the type and frequency of tobacco consumption, as well as the presence of lesions. Nevertheless, several research [14] have shown variations in the claimed prevalence. The prevalent oral mucosal lesions (OMLs) are coated tongue (26.4%), smoker's melanosis (23.5%), fissured tongue (13.2%), Fordyce's granules (13.2%), and linea alba (8.8%). Other OMLs with lower detection rates, accounting for 14.9% of cases, including nicotine stomatitis. There was one case of a precancerous lesion, specifically oral sub mucous fibrosis, but no malignant lesions were found. The occurrence of oral potentially malignant lesions (OMLs) was associated with both the type of tobacco used and the level of exposure [15]. The control group, in comparison, had a lower frequency of OMLs. The prevalent oral mucosal lesions (OMLs) among individuals who use cigarettes included fissured tongue, coated tongue, aphthae, linea alba, glossitis, and leukoplakia [16]. The prevalent observations in our study encompassed several oral manifestations, including coated tongue, melanosis in individuals who smoke, linea alba, frictional keratosis, tobacco pouch keratosis, leukoedema, morsicatio buccarum, and oral submucous fibrosis. Moreover, the prevalence of melanosis in the Oral Mucosal Lesions (OML) seen in smokers in this study aligns with the results reported in other investigations [17, 18].Our research findings have revealed a significant correlation between the usage of cigarettes and Oral Mucosal Lesions (OMLs). The current study examined the length, frequency, timing, and various forms of cigarette consumption, following the methodology used in previous research studies [19, 20]. In the case group, there was a positive correlation between habit duration and frequency and the occurrence of OMLs, but no such correlation was found in the control group. The control group had a lower incidence of OMLs; yet, the specific type of tobacco employed shown a correlation with the characteristics and site of OMLs. The characteristics and distribution of Oral Mucosal Lesions (OMLs) are dependent on the type of tobacco used, the manner in which it is used, as well as the frequency and length of use [21]. Nonetheless, our research discovered that the patient's duration of tobacco product consumption was not a statistically significant predictor of Oral Mucosal Lesions (OMLs). Individuals who use tobacco have a significantly higher risk of developing oral potentially malignant lesions (OMLs) than those who do not. As a result, more research at various dental facilities and hospitals is recommended in order to obtain a more accurate assessment of the prevalence of Oral Mucosal Lesions (OML) in Riyadh City [22].
A potential constraint of the research lies in its exclusive focus on a privately-owned dental hospital [23]. This setting may have attracted individuals primarily seeking cosmetic dental procedures, rather than those seeking treatment for oral lesions. This limitation arises from a lack of public awareness regarding the availability of oral medicine treatments at such facilities [24] (Figure 3).
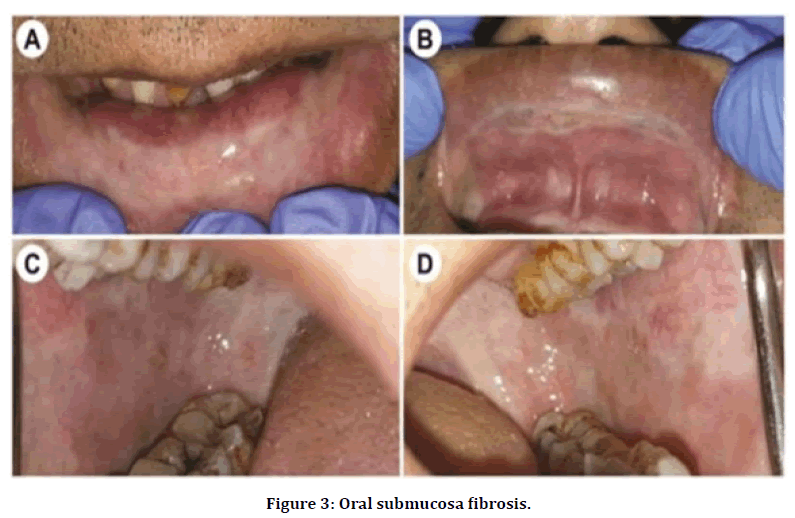
Figure 3. Oral submucosa fibrosis.
Conclusion
A recent study has demonstrated a significant association between the presence of oral mucosal ulcers and cigarette consumption. The occurrence and distribution of oral mucosal lesions are contingent upon the specific type of tobacco used, as well as the frequency and length of tobacco usage. Hence, it is advisable to refrain from cigarette usage in order to maintain the overall health of the oral mucosa. In order to effectively address the issue of tobacco use, it is imperative to implement awareness programmes throughout the community. These campaigns should aim to educate individuals about the risk factors associated with tobacco consumption and provide guidance on strategies to eradicate its use. It is recommended that these efforts be carried out in partnership with the National Committee for Tobacco Control in the Kingdom of Saudi Arabia, with the shared objective of eradicating tobacco use.
Acknowledgement
The authors would like to thank Dr. Renad Allahim for participating in the data collection.
References
- Moradi-Lakeh M, El Bcheraoui C, Tuffaha M, et al. Tobacco consumption in the Kingdom of Saudi Arabia, 2013: findings from a national survey. BMC Public Health. 2015;15.
- Algabbani AM, Almubark R, Althumiri N, et al. The prevalence of cigarette smoking in Saudi Arabia in 2018. FDRSJ. 2018;1.
- Behura SS, Masthan MK, Narayanasamy AB. Oral mucosal lesions associated with smokers and chewers–A case-control study in Chennai population. J Clin Diagn Res. 2015;9.
- Ahmadi-Motamayel F, Falsafi P, Hayati Z, et al. Prevalence of oral mucosal lesions in male smokers and nonsmokers. Chonnam Med J. 2013;49.
- Castellsagué X, Quintana MJ, Martínez MC, et al. The role of type of tobacco and type of alcoholic beverage in oral carcinogenesis. Int J Cancer. 2004;108.
- Sujatha D, Hebbar PB, Pai A. Prevalence and correlation of oral lesions among tobacco smokers, tobacco chewers, areca nut and alcohol users. Asian Pac J Cancer Prev. 2012;13.
- Qattan AMN, Boachie MK, Immurana M, et al. Socioeconomic determinants of smoking in the Kingdom of Saudi Arabia. Int J Environ Res Public Health. 2021;18:5665.
- Bassiony MM. Smoking in Saudi Arabia. Saudi Med J. 2009;30.
- Neville BW, Damm DD, Allen C,et al. Oral and maxillofacial pathology. Elsevier Health Sciences. 2015.
- Muthukrishnan A, Warnakulasuriya S. Oral Health consequences of smokeless tobacco use. Indian J Med Res. 2018;148.
- Verma R, Khanna P, Prinja S, et al. Prevalence of tobacco use & its correlate factors among school going adolescents in rural areas of Haryana, India. Indian J Public Health Res. 2012;2.
- AI MD, MJ GP. Epidemiological study of oral mucosa pathology in patients of the Oviedo School of Stomatology. Medicina Oral: Organo Oficial de la Sociedad Espanola de Medicina Oral y de la Academia Iberoamericana de Patologia y Medicina Bucal. 2002;7.
- Cadugo MA, Chua MG, Feliciano MA, et al. A preliminary clinical study on the oral lesions among the Dumagats. J Philipp Dent Assoc. 1998;50.
- Campisi G, Margiotta V. Oral mucosal lesions and risk habits among men in an Italian study population. J Oral Pathol Med. 2001;30..
- Mehrotra R, Thomas S, Nair P, et al. Prevalence of oral soft tissue lesions in Vidisha. BMC Res Notes. 2010;3.
- Jainkittivong A, Aneksuk V, Langlais RP. Oral mucosal conditions in elderly dental patients. Oral Dis. 2002;8.
- Pentenero M, Broccoletti R, Carbone M, et al. The prevalence of oral mucosal lesions in adults fro the Turin area. Oral Dis. 2008;14.
- Srivastava R, Sharma L, Pradhan D,et al. Prevalence of oral premalignant lesions and conditions among the population of Kanpur City, India: A cross sectional study. J Family Med Prim Care. 2020;9.
- Kiran Kumar KK, Saraswathi TR, Ranganathan K, et al. Oral submucous fibrosis: A clinico-histopathological study in Chennai. Indian J Dent Res. 2007;18..
- Morger R, Ramseier CA, Rees TD, et al. Oral mucosal findings related to tobacco use and alcohol consumption: a study on Swiss army recruits involving self-reported and clinical data. Oral Health Prev Dent. 2010;8.
- Saraswathi TR, Ranganathan K, Shanmugam S,et al. Prevalence of oral lesions in relation to habits: cross-sectional study in South India. Indian J Dent Res. 2006;17.
- Hayes RB, Bravo-Otero E, Kleinman DV, et al. Tobacco and alcohol use and oral cancer in Puerto Rico. Cancer Causes Control. 1999;10.
- Winn DM. Tobacco use and oral disease. J Dent Educ. 2001;65.
- Gupta PC, Mehta FS, Pindborg JJ, et al. Primary prevention trial of oral cancer in India: a 10-year follow-up study. J Oral Pathol Med. 1992;21.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Malak AlOsaimi1*, Cristalle Soman1, Asma Almeslet1, Nader AlAmri2, Riyadh AlShaye2, Rawan AlHarbi3 and Tariq Wahass2
1Maxillofacial Surgery and Diagnosis Sciences, College of Dentistry, Riyadh Elm University, Saudi Arabia2College of Dentistry, Riyadh Elm University, Riyadh, Saudi Arabia
3AlFarabi College, Riyadh, Saudi Arabia
Published: 27-May-2024
