Research - (2021) Volume 9, Issue 3
Dental Practice and COVID-19: A Brief Outlook
Asma Khurshid1*, Madiha Mohaimin2, Anam Bilal2, M Ammar Ahmed3, Tuba4, Fahad Kidwai5, Nighat Shafiq6 and Kulsum Iqbal7
*Correspondence: Asma Khurshid, DOW Research Institute of Biotechnology and Biomedical Sciences, DOW College of Biotechnology, DOW University of Health Sciences, Karachi,, Pakistan, Email:
Abstract
Based on transmissibility and high mortality rate of COVID-19, it has incapacitated the global health care systems and economy. The emergence of 2019 novel coronavirus (2019- nCoV) outbreak has put the global population under major life-threatening state. The global expeditious spread of COVID-19 pandemic from China is mainly based on airborne transmission of aerosols and possibly through viral droplets due to close contact with infected individuals especially during speaking, sneezing and breathing. Based on clinical requirements dental practitioners and patients are under considerable huge risk of exposure to SARS-CoV-2 infection. Compared to other healthcare professions, the epidemic period of COVID-19 has posed severe limitations in terms of diagnosis and treatment of oral health emergencies due to lack of instructional guidelines, swift and contagious spread of virus presenting devastating situation of cure and prevention. The aim of this article is to share the general perspective and associated challenges of post pandemic impact from dental practitioners, clinicians and faculty affiliated to dental education and clinical dentistry practice across the globe due to coronavirus disease (COVID-19) outbreak. In this article we will focus on our recent understanding related to the prevalence, viral biological characteristic, and mode of transmission and clinical manifestation of SARS-CoV-2. The potential risk of transmission among dental setup emphasizes the implementation of effective strategies and policies to mitigate the transmission rate and impact of SARS-CoV-2.
Keywords
Coronavirus, 2019-nCoV, COVID-19, SARS-CoV-2, Dentistry, Dental practice, Prevention, Infection, Transmission, Clinicians
Introduction
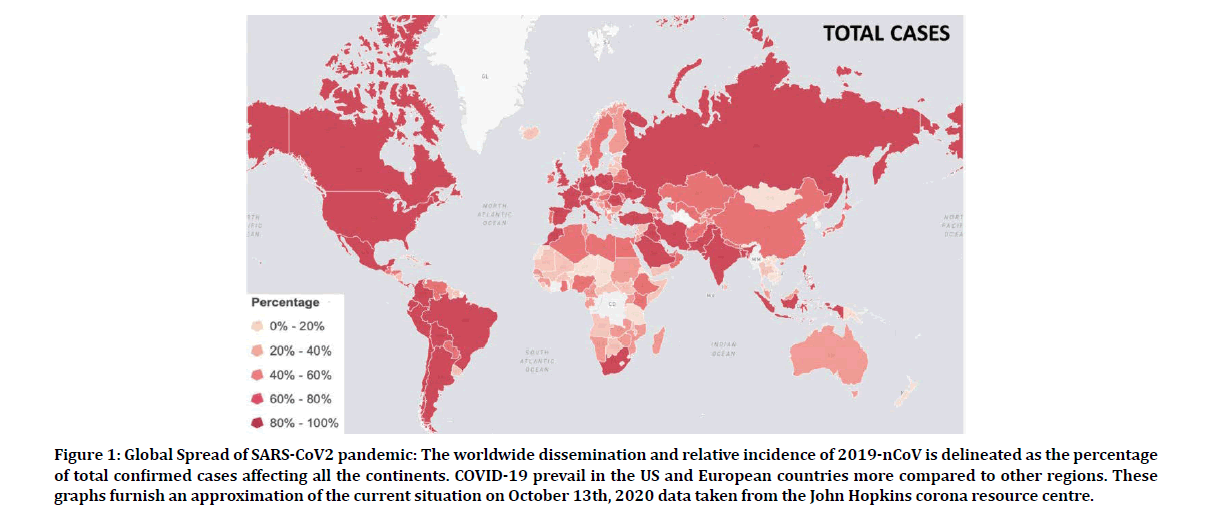
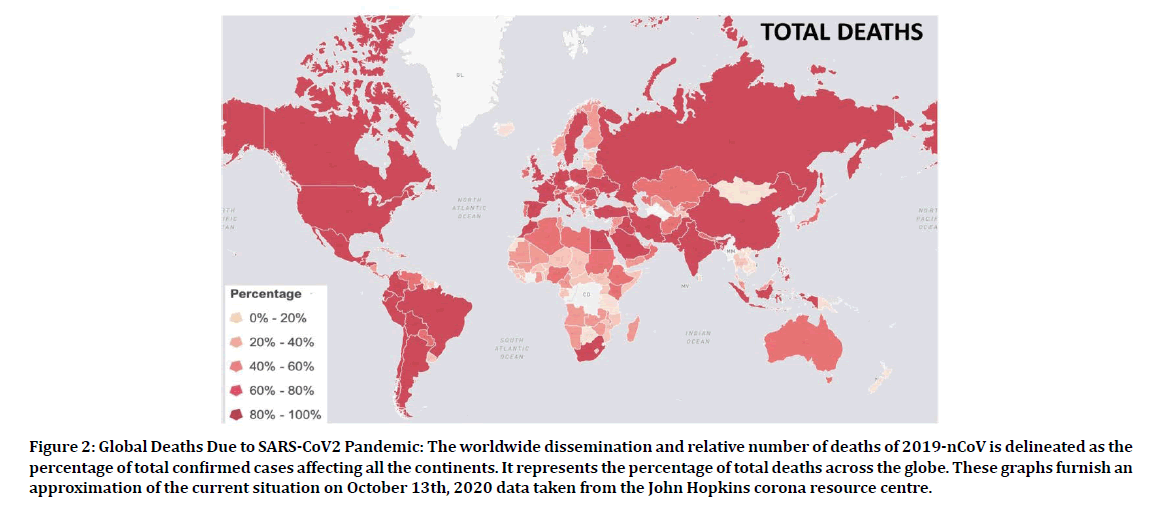
With the advancement of disease, the millions of lives are at risk. This outbreak has precede to more than 38 million proved cases and has claimed around 1,097,278 lives worldwide according to John Hopkins Coronavirus Resource center. It spread rapidly across the globe in more than 213 countries due to its contagious nature and high mortality rate. Figures 1 and 2 represents the worldwide status of the COVID-19 pandemic. The airborne transmission route of SARS-CoV-2 makes it highly infectious specifically in dental setting and become tremendous problem for patients, clinicians and professional practitioners [1]. The involvement of instruments during dental practice can cause aerosols. This manuscript will summarize and review the transmission, clinical manifestation and biological features of the virus in order to formulate the useful guideline in relation to the preventive measures for dental environment crucial for our understanding for purposeful response in controlling of SARS-CoV-2 infection among professional and patients. The perspective on post pandemic scenario from dental professionals, researchers, clinicians and academicians related to patient care, dental emergency and on routine dental health practice has been discussed with possible management strategies since the implementation of worldwide lockdown.
Figure 1: Global Spread of SARS-CoV2 pandemic: The worldwide dissemination and relative incidence of 2019-nCoV is delineated as the percentage of total confirmed cases affecting all the continents. COVID-19 prevail in the US and European countries more compared to other regions. These graphs furnish an approximation of the current situation on October 13th, 2020 data taken from the John Hopkins corona resource centre.
Figure 2: Global Deaths Due to SARS-CoV2 Pandemic: The worldwide dissemination and relative number of deaths of 2019-nCoV is delineated as the percentage of total confirmed cases affecting all the continents. It represents the percentage of total deaths across the globe. These graphs furnish an approximation of the current situation on October 13th, 2020 data taken from the John Hopkins corona resource centre.
Clinical manifestation
According to the latest study six different types of SARS-CoV-2 has been reported. Each type has been linked to distinct sets and variable degree of symptoms. The symptom most experienced by the patients with pneumonia due to SARS-CoV-2 is fever followed by cough. Other symptoms include shortness of breath, loss of appetite, muscle aches, loss of sense of taste (ageusia), sore throat, fatigue, diarrhea, loss of smell (anosmia) and headache [2-4]. It is reported that 20% and 60% of COVID-19 patients have experienced varying degree of loss of taste or smell [5].
What is SARS-CoV-2?
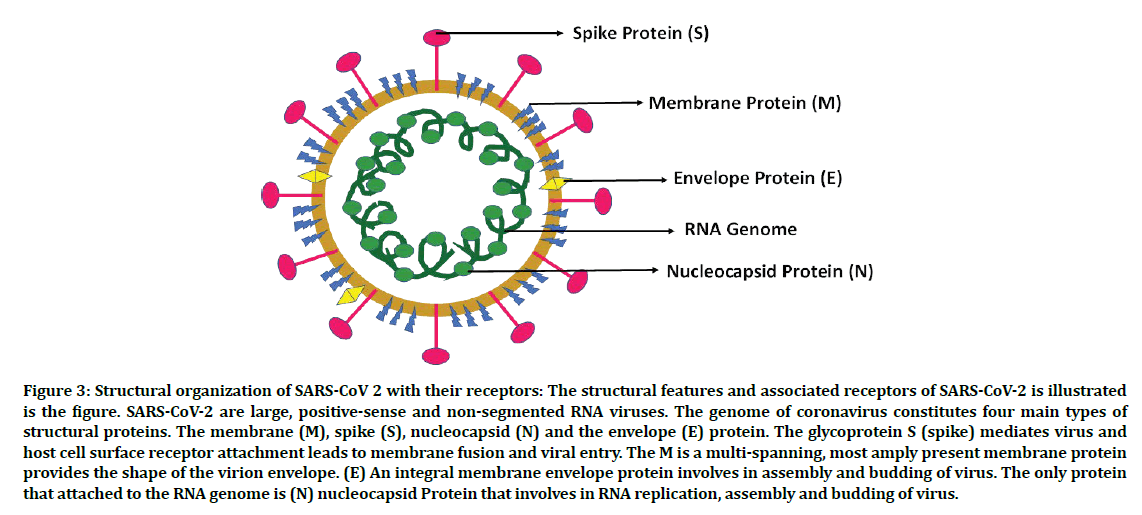
The SARS-CoV-2 a highly infectious member of its family with high mortality and morbidity rates makes it the most pernicious virus in the history of mankind. All members of CoVs possess same genome organizations with single large RNA genome that encodes 27 proteins. The ORF at the 3’ end encode 4 structural proteins named as the membrane (M), (S) spike, nucleocapsid (N) and envelope (E) proteins [6-8]. The four viral structural proteins are involved in virus structure and in replication cycle (Figure 3). Among all known structural proteins envelope spike (S) protein serves as a main determinant of host viral specificity and infectivity [9,10]. Among all structural proteins the E protein is the smallest (∼8–12 kDa) transmembrane protein with a C-terminal endodomain and N-terminal ectodomain [11]. The N protein (43 to 50 kDa) in size is an integral protein part of the helical nucleocapsid and among all structural proteins it solely interacts with the genomic RNA like a bead on a string manner [12].
Figure 3: Structural organization of SARS-CoV 2 with their receptors: The structural features and associated receptors of SARS-CoV-2 is illustrated is the figure. SARS-CoV-2 are large, positive-sense and non-segmented RNA viruses. The genome of coronavirus constitutes four main types of structural proteins. The membrane (M), spike (S), nucleocapsid (N) and the envelope (E) protein. The glycoprotein S (spike) mediates virus and host cell surface receptor attachment leads to membrane fusion and viral entry. The M is a multi-spanning, most amply present membrane protein provides the shape of the virion envelope. (E) An integral membrane envelope protein involves in assembly and budding of virus. The only protein that attached to the RNA genome is (N) nucleocapsid Protein that involves in RNA replication, assembly and budding of virus.
Transmission of SARS-CoV-2
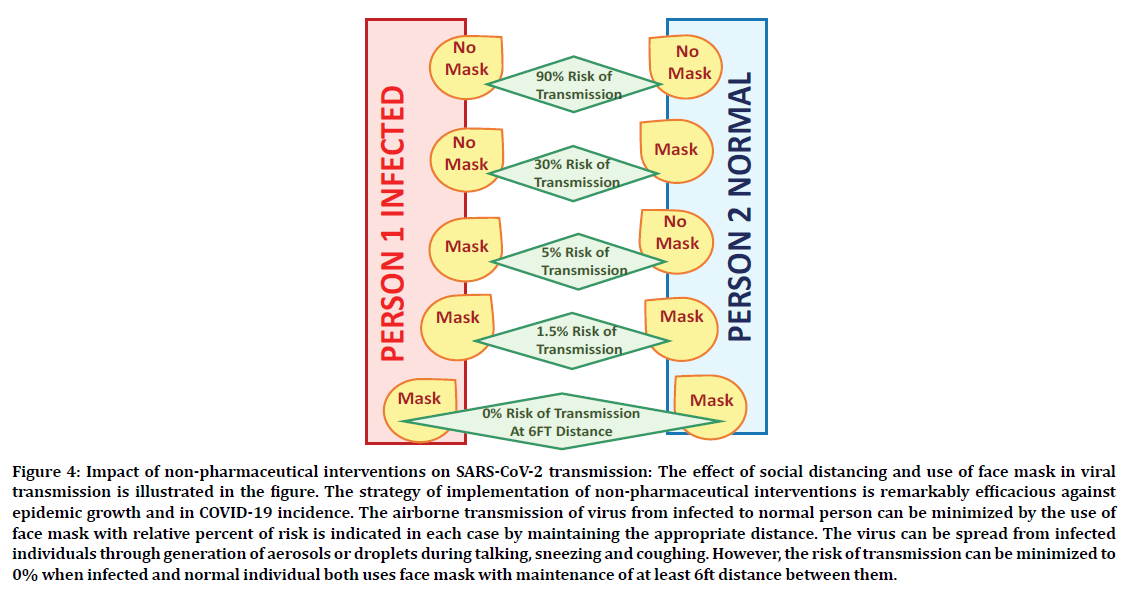
Human to human dissemination is among the major factor behind the rapid spread of infection from symptomatic or asymptomatic infected individuals. The primary transmission mode is symptomatic transmission that refers to the viral spread from an individual carrying symptom. It is reported that level of viral shedding is high in first 3 days of symptoms onset. The unrivaled challenge in regulating the swift promulgation of SARS-CoV-2 is presymptomatic patients that might be infectious, they can transmit disease before they become symptomatic [13-15]. The main route of transmission is through respiratory droplets or aerosol when infected individuals talk, cough, sneeze or possible contact routes due to close proximity, therefore use of face mask and maintaining minimal distance of 6ft is highly recommended also represented in Figure 4 [16,17]. The distance of less than 1 m should be avoided especially when one comes in contact with individuals with respiratory symptoms for infection control. The initial spread of human infection was first identified from Huanan Seafood Market in Wuhan city, China [4]. SARSCoV- 2 has been detected viable in aerosols for up to 3 hours followed by aerosolization, on copper for 4 hours, on plastic and steel till 2-3 days, and on cardboard till 24 hours thus becoming a main source of infection once an individual comes in contact with the contaminated objects followed by the direct contact through nasal or oral cavity [18,19]. The average incubation range of the infection is around 4 to 5 days that could last up to 14 days. The only cure to stop person to person transmission of COVID-19 infection is isolation of infected patients followed by several treatments. The possible intermediate hosts that promote the viral emergence among humans are civet cats for SARS-CoVs and for MERS-CoV are dromedary camels [20,21]. Transmission of virus through animals in humans is still not clear however it might be possible through taking raw meat or milk of infected animals or when one comes in direct contact with intermediated host animals [22].
Figure 4: Impact of non-pharmaceutical interventions on SARS-CoV-2 transmission: The effect of social distancing and use of face mask in viral transmission is illustrated in the figure. The strategy of implementation of non-pharmaceutical interventions is remarkably efficacious against epidemic growth and in COVID-19 incidence. The airborne transmission of virus from infected to normal person can be minimized by the use of face mask with relative percent of risk is indicated in each case by maintaining the appropriate distance. The virus can be spread from infected individuals through generation of aerosols or droplets during talking, sneezing and coughing. However, the risk of transmission can be minimized to 0% when infected and normal individual both uses face mask with maintenance of at least 6ft distance between them.
COVID-19 and Healthcare workers
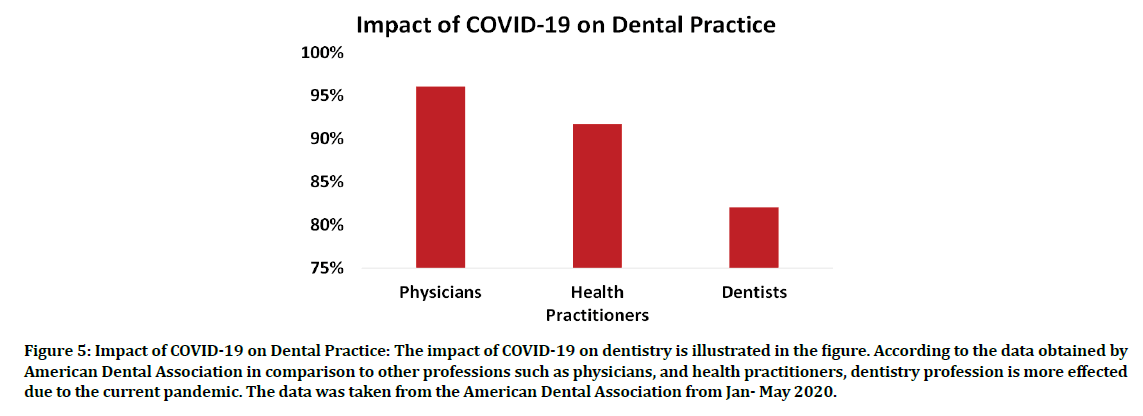
Healthcare workers are potentially at high risk of nosocomial incidents however with proper infection control strategies and use of personal protective equipment (shoe cover, N95 mask, surgical gown, coverall, head cover, double gloves, face shield) appropriate according to the pathogen infection route this could be minimized [4,23-25]. Health professionals and workers who have been involved in national crises management are working at forefront against COVID-19 battle and potential risk posed by SARS-CoV-2 for doctors and patients are same [25]. However, compared to other health professionals such as physicians and nurses, dentists are more susceptible to infection as shown in Figure 5 due to cross -infection as working closely with patients according to the published article on 15 March 2020 [26].
Figure 5: Impact of COVID-19 on Dental Practice: The impact of COVID-19 on dentistry is illustrated in the figure. According to the data obtained by American Dental Association in comparison to other professions such as physicians, and health practitioners, dentistry profession is more effected due to the current pandemic. The data was taken from the American Dental Association from Jan- May 2020.
Post-Pandemic COVID-19 scenario on dentistry
Dental profession has been facing multitudinous and unprecedented challenges during SARSCoV- 2 outbreak. The pandemic has affected the academics, research, clinical practice, patient management, safety procedures as well as the wellbeing of the dental staff [27,28]. The dental practitioners are at a high risk of COVID-19 infection because of being in close proximity to their patients [29]. The cogent restriction of clinical and surgical activities in the dental practice has resulted in a precise drastic impact on the economy of this profession [27]. Intervention by the government with respect to setting up of informed policies to aligned public and private sectors, educational institutes and social policy makers towards implementation of effective strategies for dental health crises is the need of the hour [29]. The pandemic has caused an immediate effect on the lives of professional practitioners and students associated with dental education. It has had a tremendous effect on the personal and professional life of the members of the dental fraternity and has led to having a negative impact on their psychological health as well [30]. In order to continue providing dental care to the population, associated challenges offered by the advancement and lengthening of the pandemic to the dental professionals is also enhancing tremendously [31,32].
COVID-19 Pandemic: A possible intimidation in the world of dentistry
COVID-19 has affected the dental professionals just like any other health care sector [33]. The New York Times has mentioned dentistry as one of the highest professions at risk of COVID-19 [34]. Since the spread of the disease is through human-to-human transmission, chances of infection spread in a dental set up are high. Since the virus is still novel and not much is known about the natural history of the disease, there has been tremendous amount of apprehension and uncertainty amongst the dental fraternity all over the world as to how to go about their dental practices safely [33].
The standard dental setup anywhere around the globe is such that there is every possible chance of spread of the infection through aerosols produced during routine dental procedures, between the dental practitioner and the patient as there is direct face-to-face contact between the two. Also, there are high chances of contamination through aerosol emission during dental treatment and the risk is further increased due to the use of high-speed rotary instruments [33-35]. The aerosols can settle on inanimate objects and remain suspended in air long after the completion of the dental procedure that poses a serious concern regarding COVID-19 transmission. The dental practitioner, on exposure may remain asymptomatic during the incubation period of 7 to 24 days, and during this time, there are high chances of infection to patients as well as those professionals who are working in close proximity to the exposed person [35]. All this has led to a substantial amount of intimidation among the members of the dental fraternity and thereby tremendous decrease in the number of patients that are being treated at the dental clinics as the dentists try and tend to only those cases that require immediate attention and postpone all the elective procedures that can wait for treatment and can be managed without actual contact between the dental health professional and the patient through telephonic or live online consultation [33,35].
Impact on Dental clinical Setup: Post-treatment and Pre-treatment
As evidence suggests, COVID-19 infection spreads via droplet inhalation, with asymptomatic carriers pose a greater threat of silent transmission of the virus. It can spread either through micro droplets that are inhaled by a person due to being in direct proximity of an infected person (a distance of less than two meters and an exposure time duration of greater than fifteen minutes), or it can also be transmitted as a result of inhalation of core droplets that remain suspended in air after being released by coughing or sneezing by an infected person [36]. In terms of dental practice, the risk of acquiring COVID-19 virus is equal for both the dentist and the patient due to their proximity during various dental procedures [35]. In view of this situation, all possible measures must be taken to modify the dental clinical setup in such a way that the chances of spread of COVID-19 are minimized.
Safety precautions
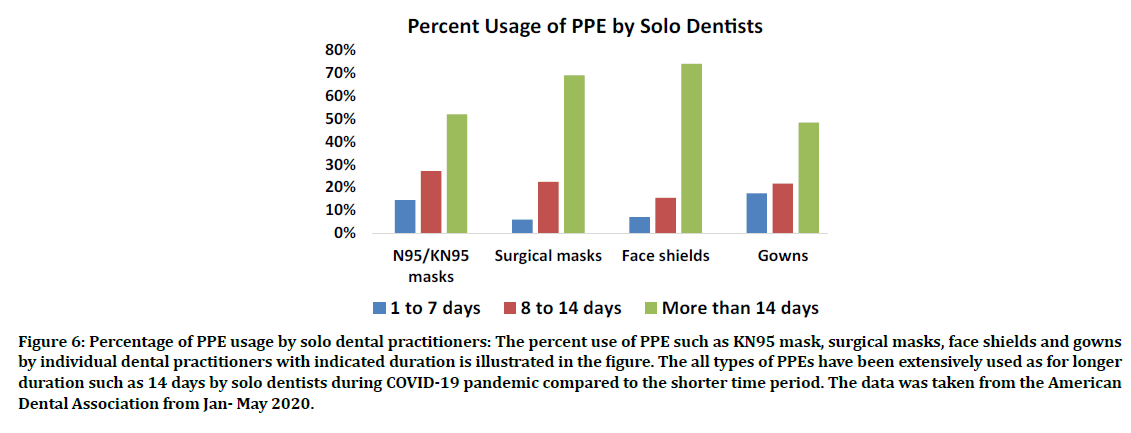
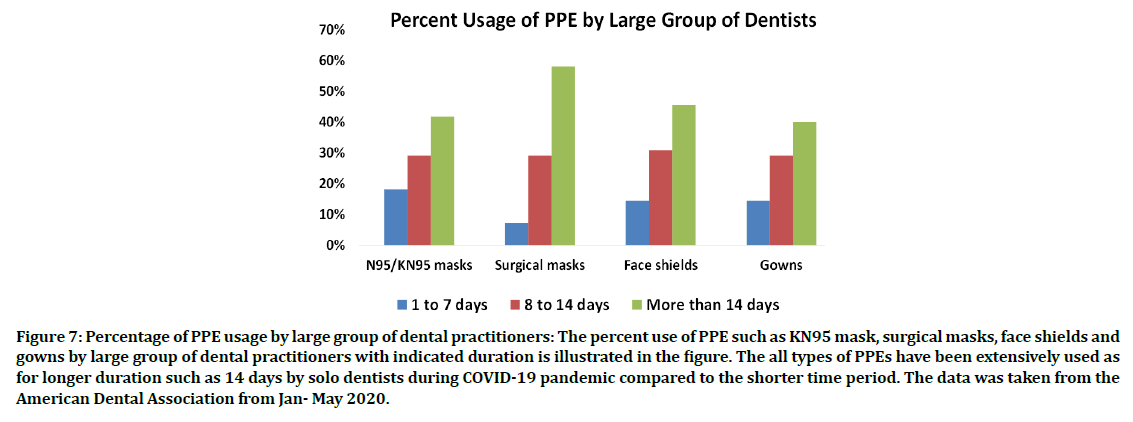
The American Dental Association (ADA) and the Centers for Disease Prevention and Control (CDC) have suggested to keep the waiting rooms empty without any overlap of appointments and if that is not possible, maintenance of social distance between two patients in the waiting area. All the unnecessary items like brochures, magazines etc. must be removed from the waiting area [35,36]. All patients must be informed beforehand regarding their appointment schedules [36]. Furthermore, the patients can be asked to wait in their automobiles, till they can safely be seen by the dentist [37]. The dentists should follow the protocol for personal protection at all times which includes the use of personal protective equipment (PPE) and these should be properly disposed of according to the given instructions. The percent use of PPE such as KN95 mask, surgical masks, face shields and gowns by solo and large group of dentists during span of 1 to 14 days has been shown in the Figure 6 and 7. The highest percent use of all PPEs has been observed till maximum observed period of 14 days as compared to shorter durations [38]. Hands should be washed properly before and after examining or treating a patient. Care should be taken to avoid touching the face, eyes and nose until it safe to do so [35]. Use of rubber dams reduces the aerosol production significantly [34,35]. It is highly recommended to use anti-retraction handpieces instead of the usual high speed rotary instruments as the reduce the backflow of pathogens from the oral cavity into the handpiece tubes [34,35]. The treatment of patients who require aerosol producing treatment should be done towards the end of the day [37]. The use of extraoral radiographic techniques is preferred in over intraoral ones [36]. Use of intraoral radiography should be avoided as it stimulates salivation and coughing that can lead to the spread of infection. Orthopantomography or CT (Computed Tomography) scan can be used when absolutely necessary. Use of four-handed dentistry also helps reduce cross contamination [34]. Follow up of all the patients must be done for any symptoms of COVID-19 [36]. Clinical waste should be properly disposed of in bags and marked in order to facilitate their proper elimination of medical waste [34,35]. The use of sodium hypochlorite as a surface disinfectant surfaces for about 10 minutes along with steady ventilation of the dental surgery room is suggested [34]. A proper record of the body temperature and symptoms, if any, of all the people working in the dental clinical setup must be strictly maintained. This record should be reviewed from time to time in order to spot any suspected cases, and in case any dental healthcare provider is a suspected case of COVID-19, he or she should be asked not to come to work and their primary healthcare providers should be informed in order to decide whether medical evaluation is necessary [36].
Figure 6: Percentage of PPE usage by solo dental practitioners: The percent use of PPE such as KN95 mask, surgical masks, face shields and gowns by individual dental practitioners with indicated duration is illustrated in the figure. The all types of PPEs have been extensively used as for longer duration such as 14 days by solo dentists during COVID-19 pandemic compared to the shorter time period. The data was taken from the American Dental Association from Jan- May 2020.
Figure 7: Percentage of PPE usage by large group of dental practitioners: The percent use of PPE such as KN95 mask, surgical masks, face shields and gowns by large group of dental practitioners with indicated duration is illustrated in the figure. The all types of PPEs have been extensively used as for longer duration such as 14 days by solo dentists during COVID-19 pandemic compared to the shorter time period. The data was taken from the American Dental Association from Jan- May 2020.
Patient care and management
Sound knowledge of COVID-19 is mandatory for prevention of spread of the infection in a dental clinic. Because of the novelty of the virus, much is still unknown about the natural history of the disease and hence proper patient screening is an absolute necessity in order to minimize the spread of the pathogen in a dental setup.
Use of telephone triage and questionnaire-based information collection from the patients prior to their visit to the dentist regarding symptoms, if any, and movements during the past two weeks along with social history should be made an essential norm in order to avoid unnecessary contact with suspected cases of COVID-19 [34,35]. Use of tele-dentistry includes telescreening, tele-triage, and teleconsulting. Telescreening involves acquiring patient history over telephone and teleconsulting is providing consult to the patient via a live video [36]. This remote service helps provide the required advice and prescribe medication without actual contact with the patient [35,36].
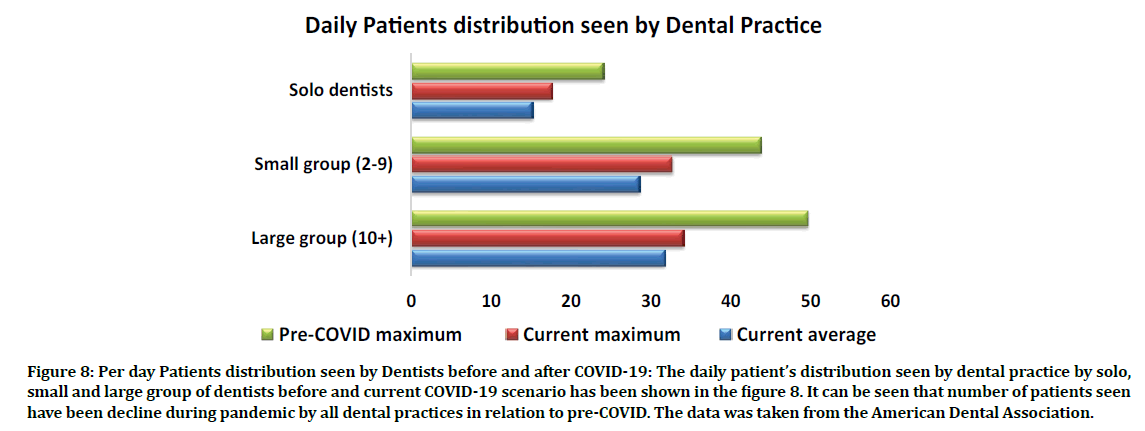
During COVID-19 the daily number of patients seen by solo, small and large group of dentists has been decline compared to pre- COVID as shown in the Figure 8 [38]. The daily patient’s distribution seen by dental practice by solo, small and large group of dentists before and current COVID-19 scenario has been shown in the Figure 8. It can be seen that number of patients seen have been decline during pandemic by all dental practices in relation to pre-COVID. The data was taken from the American Dental Association. Proper patient screening should be done of the patients entering the dental clinic. Obtaining sound history from the patients for possible signs and symptoms of coronavirus, such as cough, fever and shortness of breath is an extremely essential part of the patient screening process [37]. The use of oral rinses like chlorhexidine or hydrogen peroxide prior to the commencement of dental treatment may help reduce the chances of cross contamination through aerosols [34,35]. Persons accompanying pediatric patients must not attend the treatment in order to avoid aerosol inhalation [34]. Disposable should be used during dental treatment as much as possible in order to avoid cross contamination [39].
Figure 8: Per day Patients distribution seen by Dentists before and after COVID-19: The daily patient’s distribution seen by dental practice by solo, small and large group of dentists before and current COVID-19 scenario has been shown in the figure 8. It can be seen that number of patients seen have been decline during pandemic by all dental practices in relation to pre-COVID. The data was taken from the American Dental Association.
Use of antiviral mouthwashes
The use of antiviral mouthwashes could help in reducing the viral load in throat and in the oral cavity. It is assumed that the use of mouthwashes through gargling can be effective in decreasing the load of viruses and possibly the transmission of disease for a short-term period. The transmission of SARS-CoV-2 through saliva, aerosol and droplet in the dental practice could also be minimized by the use of antiviral mouthwashes before dental procedures and also among suspected COVID-19 individuals to overcome the essential problems linked with oral microbial flora [40].
Dental emergencies and COVID-19
Dental emergencies arise and escalate in a short span of time and hence require immediate attention [41]. Furthermore, it is extremely important for the dental practitioners to follow proper protocol for treatment of the patients as well as assess the level of exposure risk associated with the task involved. According to Occupational Safety and Health Administration (OSHA), there are various levels of exposure, ranging from low to very high, associated with the tasks to be performed by the dentists. Examination and treatment of suspected or confirmed COVID-19 patients falls under the high caution category [42].
Various kind of dental emergencies include uncontrolled bleeding or compromised airway of the patient due to trauma, cellulites etc. [43]. Such cases should be treated only after proper assessment of the patients as well as the risk to the patient and the dental healthcare providers [44]. Adequate supplies of all the necessary items required for treatment procedures to be conducted must be ensured. If in case the supplies are limited, it is advisable to prioritize the treatment of those patients who are at a higher risk if treatment is further delayed, over those cases that can be deferred [44]. Apart from dental emergencies, some patients may require urgent dental care, like those suffering from dry socket or acute pulpitis. Such patients must be handled with utmost caution and care and only when the treatment cannot be deferred any further [43].
COVID-19 Pandemic Impact on Dental Education
With the outbreak of COVID-19 came the imposition of lockdowns and rules for social distancing. This included shutdown of preclinics, clinics and educational institutes as well with access provided only for emergency use and vulnerable population. This hindered learning opportunities for students thereby increasing the difficulties of academicians in adapting to the new guidelines. Therefore, it necessitated alternative modes of imparting education via webinars, online mode of presentations, exams and assessments to avoid the spread of COVID-19 [45]. With the advancement in technology, students can attend lectures from their homes using various software available online without having to attend the lectures in person which could risk spreading COVID-19 virus. This form of E-learning has increased selfpaced independent learning amongst students. Dentistry being a skill-based profession requires hands on training for better skill development. To tackle this way to provide Undergraduate training has been improved via virtual reality (VR) simulation technology. The haptic technology in VR simulators have been effective and safe in helping the students to feel and touch the tooth tissue virtually and helps improve the hand-eye coordination and motor skills via distance learning during this pandemic [35]. Apart from this changes that have been incorporated are reduction in clinical hours, extension of various program dates, changes in exam and assessment patterns. However, all the virtual modalities cannot match up to the realtime patient experience required for learning dentistry and has resulted in a deficit in clinical exposure for undergraduates and trainees [46]. Looking at the current situation it is imperative to say that COVID-19 will have a huge impact on dental education which may bring about a change in the overall oral healthcare system in the future [47].
COVID-19 pandemic Impact on Research
Research has been badly affected due to COVID-19 with various institutes scaling back research activities and stopping or slowing down laboratory experiments which have resulted in time and financial loss. There has been a delay in research process, grant applications, result publications and postponing of academic conferences. Various academic institutes have announced a hiring freeze leading to unemployment in post-doctoral fellows affecting them financially and mentally [28]. However, this has opened an opportunity amongst researchers with funding agencies prioritizing COVID-19 related research. Future researches in relation to dentistry and COVID-19 can include: Issues related to COVID-19 and Dental Public Health, Effect of the pandemic on dentistry as a profession, Role of PPE in dentistry, Screening, diagnosing, and managing COVID-19 patients in a dental setup, Use of teledentistry in clinical and educational setup, effect of COVID-19 on oral tissues [48,49].
Psychological impact of pandemic on dental professionals
Due to the spread of COVID-19 virus via airborne droplets, dental professionals have been considered to be at a greater risk of acquiring infection, as they work in close proximity with their patients. The pandemic has led to limited physical contact with family members and friends as anxiousness has been on the rise amongst medical and dental healthcare workers about catching the virus and infecting their loved ones [50,51]. As the incubation period before symptoms of COVID-19 is long, fear developed by working dentists is the risk of carrying the virus home and infecting their families. This along with the apprehensions of precautionary quarantine in case of suspected disease or mandatory quarantine in case of actual infection has caused psychological distress amongst dentists and other healthcare workers [52]. Dental academic staff who teach and train dental students face stress due to overload of work in proving e-learning in this current situation and fear of not meeting the expectations [53]. Mild anxiety has led to increased implementation of precautionary measures against COVID-19 but prolonged severe anxiety affects mental and physical health [54].
In order to counter these effects inspiration has to be sought for joy and mental well-being. Social media has an important role in keeping everyone in touch with their family and friends who are away. Counseling and psychological support groups have to play a very crucial role in motivating the students and the trainees both during and post pandemic [35,55]. Several surveys should be conducted in hospitals and dental clinics, to evaluate the amount of physical and mental exhaustion of the healthcare workers and accordingly counseling should be provided [55]. By following the recommended protocol, dentists and dental healthcare workers can curtail their fears and anxiety regarding catching the COVID-19 virus [52].
Role of tele-dentistry in the pandemic
Tele-dentistry means the use of technology to deliver educational, medical and healthcare services in a virtual manner [56]. An alternative method to provide healthcare facilities to patients during lockdown keeping in mind social distancing led to an increased use of teledentistry. This helped practitioners to provide consultation, clinical care to patients and conduct triage and categorize patients as acute or chronic and decide who require face to face consultation [57]. Tele-dentistry is carried out by means of telephones, secure video conferencing networks like Skype, Zoom, Face time, WhatsApp etc., based on patients’ convenience and availability of facilities. Before beginning with the consultation, patient should be made aware about the limitations of tele-dentistry and that best possible diagnosis in the absence of actual face to face consultation is being provided. This should be documented [56]. Following this patient should provide informed consent verbally before the start of consultation. After this complete history has to be obtained followed by hand sanitization by the patient for retraction of their lips or cheeks using their hands or a tongue depressor, handle of spoon etc under adequate light source for better visualization by the dentist. Patients may be asked for photographs of the lesion post video or tele-conference for better judgment and record keeping purpose [57]. Advantages of tele-dentistry include: Reduction in social contact, travel cost and risk of exposure to vulnerable patients. It has led to tele-triage of acute patients who need immediate face to face consultation or treatment and has improved access of care to rural community who are unable to travel to larger cities. Limitations of tele-dentistry include: Lack or inadequate internet facilities for every patient and dentist, Ill equipped communication facilities at healthcare institutes, Technologically unsound patients and practitioners, Two-dimensional representation of lesions, Confidentiality issues in sharing information online, lack of acceptance by patients and high -cost factor [58]. With the outbreak of COVID-19, we have adjusted to various new norms and protocols for personal protection against the virus, tele-dentistry still being a new way of diagnosis and treatment needs focus, funding and dedicated training of dental professionals for it to be accepted and used successfully both by patients and dentists in the future [59].
Conclusion
The current situation requires strong law enforcements in order to fight COVID-19. To abrogate the spread of virus international travel restrictions to suspected countries, social distancing, proper use face mask, gloves, contact tracing and sterilization are the best weapons to neutralize the corona virus infection notably in dominant viral hotspots. The existing situation of COVID-19 outbreak demands for the unprecedented global response of government, academic and policy makers to aligned together for adequate solution. Till the availability of effective cure or vaccine against SARS-CoV-2 there is an immediate need to addressed the efficient policies and guideline for optimum patient care and infection control in oral diagnosis, dental emergencies and in routine dental practice. However, like previous epidemics this time again is still very challenging to control and monitor the fast spread of virus and to develop the effective cure of COVID-19 outbreak because it evolves continuously among susceptible population. Dental practice leads to high risk of infection due to airborne transmission might occur while encountering the aerosol and droplets producing procedures necessitating the requirement of personal protective equipment and appropriate training of the healthcare professionals to ensure high level of safety and care for patients, staff, visitors and surrounding. Every one of us can make a difference as the future is our own hands now.
References
- Cagetti MG, Cairoli JL, Senna A, et al. COVID-19 outbreak in North Italy: An overview on dentistry. A questionnaire survey. Int J Environ Res Public Health 2020; 17:3835.
- Ciotti M, Angeletti S, Minieri M, et al. COVID-19 outbreak: An overview. Chemotherapy 2019; 64:215-223.
- https://www.weforum.org/agenda/2020/07/covid-19-study-6-strains-severity-kings-college-london
- Al Omari A, Ra’ed Al-Ashqar AN, Balas HA, et al. Overview of upper airway management during COVID-19 outbreak: Head and Neck Surgeon's perspective. J Craniofac Surg 2020.
- Dell’Era V, Farri F, Garzaro G, et al. Smell and taste disorders during COVIDâ?19 outbreak: Crossâ?sectional study on 355 patients. Head Neck 2020; 42:1591-1596.
- Chen B, Tian EK, He B, et al. Overview of lethal human coronaviruses. Signal Transduction Targeted Therapy 2020; 5:1-6.
- Lu R, Zhao X, Li J, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: Implications for virus origins and receptor binding. Lancet 2020; 395:565-574.
- Wu A, Peng Y, Huang B, et al. Genome composition and divergence of the novel coronavirus (2019-nCoV) originating in China. Cell Host Microbe 27:325-328.
- Andersen KG, Rambaut A, Lipkin WI, et al. The proximal origin of SARS-CoV-2. Nat Med 2020; 26:450-452.
- Pourrajab F, Zare-Khormizi MR, Sheikhha MH. Molecular basis for pathogenicity of human coronaviruses. Infect Drug Resist 2020; 13:2385-2405.
- Venkatagopalan P, Daskalova SM, Lopez LA, et al. Coronavirus envelope (E) protein remains at the site of assembly. Virology 2015; 478:75-85.
- de Haan CA, Rottier PJ. Molecular interactions in the assembly of coronaviruses. Adv Virus Res 2005; 64:165-230.
- Mahapure KS, Kulkarni NS. Asymptomatic transmission of severe acute respiratory syndrome-coronavirus 2 within a family cluster of 26 cases: Why quarantine is important? J Glob Infect Dis 2020; 12:115-116.
- Malik YA. Properties of coronavirus and SARS-CoV-2. Malays J Pathol 2020; 42:3-11.
- Wei WE, Li Z, Chiew CJ, et al. Presymptomatic transmission of SARS-CoV-2-Singapore, January 23-March 16, 2020. Morb Mortal Wkly Rep 2020; 69:411-415.
- Guo YR, Cao QD, Hong ZS, et al. The origin, transmission and clinical therapies on coronavirus disease 2019 (COVID-19) outbreak-An update on the status. Mil Med Res 2020; 7:11.
- Sakelliadis EI, Katsos KD, Zouzia EI, et al. Impact of Covid-19 lockdown on characteristics of autopsy cases in Greece. Comparison between 2019 and 2020. Forensic Sci Int 2020; 313:110365.
- Ong SW, Tan YK, Chia PY, et al. Air, surface environmental, and personal protective equipment contamination by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) from a symptomatic patient. JAMA 2020; 323:1610-1612.
- van Doremalen N, Bushmaker T, Morris DH, et al. Aerosol and surface stability of HCoV-19 (SARS-CoV-2) compared to SARS-CoV-1. medRxiv 2020.
- Chen R, Liang W, Jiang M, et al. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest 2020; 158:97-105.
- Lauer SA, Grantz KH, Bi Q, et al. The incubation period of coronavirus disease 2019 (COVID-19) from publicly reported confirmed cases: estimation and application. Annals Internal Med 2020; 172:577-582.
- Liya G, Yuguang W, Jian L, et al. Studies on viral pneumonia related to novel coronavirus SARSâ?CoVâ?2, SARSâ?CoV, and MERSâ?CoV: A literature review. Apmis 2020; 128:423-432.
- Çelebi G, PiÅ?kin N, Bekleviç AÇ, et al. Specific risk factors for SARS-CoV-2 transmission among health care workers in a university hospital. Am J Infection Control 2020; 48:1225-12230.
- Peres D, Boléo-Tomé JP, Santos G. Respiratory and facial protection: current perspectives in the context of the COVID-19 pandemic. Acta Med Portuguesa 2020; 33:583-592.
- Tian Z, Stedman M, Whyte M, et al. Personal protective equipment (PPE) and infection among healthcare workers–what is the evidence?. Int J Clin Practice 2020; 74:e13617.
- https://www.nytimes.com/interactive/2020/03/15/business/economy/coronavirus-worker-risk.html?action=click&module=Top+Stories&pgtype=Homepage
- Spagnuolo G, De Vito D, Rengo S, et al. COVID-19 outbreak: An overview on dentistry. Int J Environ Res Public Health 2020; 17:2094.
- Wu DT, Wu KY, Nguyen TT, et al. The impact of COVID-19 on dental education in North America-Where do we go next? Eur J Dent Educ 2020; 24:825-827.
- Amato A, Caggiano M, Amato M, et al. Infection control in dental practice during the COVID-19 pandemic. Int J Environ Res Public Health 2020; 17:4769.
- Jevon P, Shamsi S. COVID-19 and medical emergencies in the dental practice. Br Dent J 2020; 229:19-24.
- Checchi V, Bellini P, Bencivenni D, et al. COVID-19 dentistry-related aspects: A literature overview. Int Dent J 2021.
- Qian LI, Zhong-ren LI, Jiang TA, et al. Management and prevention of dental emergency during corona virus disease 2019 (COVID-19) epidemic. Shanghai J Stomatol 2020; 29:123.
- Balaji SM. COVID-19-Future of dentistry. Indian J Dent Res 2020; 31:167-168.
- Villani FA, Aiuto R, Paglia L, et al. COVID-19 and dentistry: Prevention in dental practice, a literature review. Int J Environ Res Public Health 2020; 17:4609.
- Barabari P, Moharamzadeh K. Novel coronavirus (COVID-19) and dentistry–A comprehensive review of literature. Dent J 2020; 8:53.
- Kochhar AS, Bhasin R, Kochhar GK, et al. COVID-19 pandemic and dental practice. Int J Dent 2020; 2020:8894794.
- Mostoufi B, Ashkenazie Z, Abdi J, et al. COVID-19 and the dental profession: Establishing a safe dental practice for the coronavirus era. J Global Oral Health 2020; 3:41.
- https://surveys.ada.org/reports/RC/public/YWRhc3VydmV5cy01ZWY5ZWE5MzIyMDBiMzAwMGZmNGM2NGUtVVJfNWlJWDFFU01IdmNDUlVO
- Ather A, Patel B, Ruparel NB, et al. Coronavirus disease 19 (COVID-19): Implications for clinical dental care. J Endodont 2020; 46:584-595.
- Moosavi MS, Aminishakib P, Ansari M. Antiviral mouthwashes: possible benefit for COVID-19 with evidence-based approach. J Oral Microbiol 2020; 12:1794363.
- Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J Dent Res 2020; 99:481-487.
- https://www.osha.gov/coronavirus/control-prevention/dentistry
- Mihailovic B, Miladinovic M, Vujicic B. Telemedicine in dentistry (Teledentistry). Advances in telemedicine: Applications in various medical disciplines and geographical areas. 2011; 22:215-30.
- https://www.cdc.gov/coronavirus/2019-ncov/hcp/dental-settings.html
- Alzahrani SB, Alrusayes AA, Aldossary MS. Impact of COVID-19 pandemic on dental education, research, and students. Int J Health Sci Res 2020; 10:207-212.
- Doughty F, Moshkun C. The impact of COVID-19 on dental education and training. Dent Update 2020; 47:527-528.
- Quinn B, Field J, Gorter R, et al. COVIDâ?19: The immediate response of european academic dental institutions and future implications for dental education. Eur J Dent Educ 2020; 24:811-814.
- Monteil V, Kwon H, Prado P, et al. Inhibition of SARS-CoV-2 infections in engineered human tissues using clinical-grade soluble human ACE2. Cell. 2020; 181:905-913.
- Moharamzadeh K, Brook IM, Van Noort R, et al. Tissue-engineered oral mucosa: A review of the scientific literature. J Dent Res 2007; 86:115-124.
- Ammar N, Aly NM, Folayan MO, et al. Behavior change due to COVID-19 among dental academics—The theory of planned behavior: Stresses, worries, training, and pandemic severity. PloS One 2020; 15:e0239961.
- Coulthard P. Dentistry and coronavirus (COVID-19)-moral decision-making. Br Dent J 2020; 228:503-505.
- Ahmed MA, Jouhar R, Ahmed N, et al. Fear and practice modifications among dentists to combat novel coronavirus disease (COVID-19) outbreak. Int J Environ Res Public Health 2020; 17:2821.
- Rutter H, Herzberg J, Paice E. Stress in doctors and dentists who teach. Med Educ 2002; 36:543-549.
- Vinkers CH, van Amelsvoort T, Bisson JI, et al. Stress resilience during the coronavirus pandemic. Eur Neuropsychopharmacol 2020; 35:12-16.
- Vergara-Buenaventura A, Chavez-Tuñon M, Castro-Ruiz C. The mental health consequences of coronavirus disease 2019 pandemic in dentistry. Disaster Med Public Health Preparedness 2020; 1-4.
- Niazi MIK GS. Teledentistry and COVID-19; Today and tomorrow. Biomedica 2020; 36:74-76.
- Villa A, Sankar V, Shiboski C. Tele (oral) medicine: A new approach during the COVIDâ?19 crisis. Oral Diseases 2020.
- Murillo-Escobar MA, Cardoza-Avendaño L, López-Gutiérrez RM, et al. A double chaotic layer encryption algorithm for clinical signals in telemedicine. J Med Systems 2017; 41:59.
- Ghai S. Are dental schools adequately preparing dental students to face outbreaks of infectious diseases such as COVID-19? J Dent Educ 2020; 84:631-633.
Author Info
Asma Khurshid1*, Madiha Mohaimin2, Anam Bilal2, M Ammar Ahmed3, Tuba4, Fahad Kidwai5, Nighat Shafiq6 and Kulsum Iqbal7
1DOW Research Institute of Biotechnology and Biomedical Sciences, DOW College of Biotechnology, DOW University of Health Sciences, Karachi, Pakistan2Institute of Dental Sciences, Sehora, Jammu University, Jammu & Kashmir, India
3Faculty of Mathematics, Informatics and Statistics, Ludwig Maximilian University of Munich, Geschwister-Scholl-Platz 1,München,, Germany
4DOW College of Biotechnology, DOW University of Health Sciences, Karachi, Pakistan
5Department of Health and Human Services, Craniofacial and Skeletal Diseases Branch, National Institute of Dental and Craniofacial Research, National Institutes of Health, Bethesda, MD, USA
6Oral Biology department, Khyber College of Dentistry, Peshawar University, Pakistan
7School of Dental Medicine, Tufts University, Boston, MA, USA
Citation: Asma Khurshid, Madiha Mohaimin, Anam Bilal, M Ammar Ahmed, Tuba, Fahad Kidwai, Nighat Shafiq, Kulsum Iqbal, Dental Practice and COVID-19: A Brief Outlook, J Res Med Dent Sci, 2021, 9 (3):154-164.
Received: 27-Feb-2021 Accepted: 18-Mar-2021 Published: 25-Mar-2021