Research - (2021) Volume 9, Issue 4
CT Evaluation of Infective Renal Pathologies
Sanjivanee Ingole and Prabakaran M*
*Correspondence: Prabakaran M, Department of Radio Diagnosis, Sree Balaji Medical College & Hospital, Bharath Institute of Higher Education and Research, India, Email:
Abstract
The present study aims to evaluate role of Computed Tomography in Diagnosis and Characterization of Renal Infectious Diseases, delineating the extent of pathology and identifying associated complications. Patients with uncontrolled diabetes mellitus with history of recurrent urinary tract infections or renal calculi, symptoms of flank pain, dysuria and fever, should be considered as high risk. These patients should be closely followed up with contrast enhanced or non-contrast CT scan, depending on their renal function.
Keywords
Chronic pyelonephritis, Xanthogranulomatous pyelonephritis, Emphysematous pyelonephritis, Renal tuberculosis
Introduction
Renal infections encompass a spectrum of infections which are treatable with timely diagnosis and proven life threatening complications. Renal infections are a result of either hematogenous or retrograde spread to kidneys with female preponderance. Inspite of the usual protocol of uncomplicated cases being treated medically, CT has been increasingly requested especially in high risk patients. Computed tomography is of great value in high risk patients evaluation, equivocal cases and determining the disease extent. CT scan is the gold standard in diagnosis of renal infections [1,2].
Renal tuberculosis, acute pyelonephritis, perinephric abscess, renal abscess xanthogranulomatous pyelonephritis and emphysematous pyelonephritis are various types of renal infections. Uncomplicated renal infections usually do not require computed tomography imaging, but it aids in the diagnosis, establishes the disease extent and helps in evaluating patients with high risk.
Non-contrast CT provides valuable information in diagnosis of calculi. Calcification in parenchyma, hemorrhage and inflammatory masses while contrast enhanced CT is valuable in demonstrating renal excretory abnormalities and other features of renal inflammation. In renal infectious diseases, its function is usually affected and hence contrast studies are essential to demonstrate alterations occurring in excretion of contrast.
To identify complications like abscess formation and the extent of disease, CT scans obtained in excretory phase are more helpful. Therefore delayed CT scans are more frequently used than early CT scans. Complications of renal infections include renal facial thickening, abscess formation, renal failure and renal scarring. Presence of these complications indicates urinary obstruction.
Renal perfusion abnormalities in acute pyelonephritis are demonstrated in nephrogenic phase, where homogenous enhancement of renal parenchyma is seen. To detect subtle lesions nephrogenic phase is more sensitive than corticomedullary phase. For extra renal extent of xanthogranulomatous pyelonephritis, mainstay of imaging is CT [3].
In cases of renal tuberculosis, CT plays a major role in evaluation of residual renal parenchyma function, papillary necrosis, calyceal erosion and extra renal spread [4].For perinephric abscess CT scan is the investigation of choice, since it is more sensitive. CT helps in defining the size, precise location, extent and degree of the loculation with respect to other retroperitoneal structures [5].
CT scan is useful in both diagnosing and planning operative procedures in cases of intra-renal abscess [6]. On CT it appears as hypodense, wedge shaped, poorly defined area that may have focal renal involvement and liquefaction. This lesion does not enhance on administration of contrast, is distinctly marginated and has low attenuation of 0 to 20 Hounsfield units. Perirenal fluid collection and inflammatory stranding with thickened Gerota’s fascia are some of the other features [7].
Materials and Methods
Source of data
A descriptive study was performed with 50 patients between November 2017 and September 2019, who were referred to the department of Radiology at Sree Balaji Medical College and Hospital, Chennai with symptoms suggestive of renal infective pathologies were reviewed (flank pain, fever, chills, dysuria, trauma).
Inclusion criteria
• All patients clinically suspected to have renal infective pathology.
• All patients diagnosed incidentally on ultrasound of renal infections.
• Patients above 16 years of age irrespective of sex.
• Paediatric population (age <16 years)
• Pregnant patients.
Method of collection of data
Patients referred to the department of Radiology with symptoms suggestive of renal infective pathologies were reviewed (flank pain, fever, chills, dysuria, trauma).
A total number of 50 cases were taken up for the study. Relevant history was taken into account: diabetes mellitus, immunosuppression, renal transplant, debilitating diseases, intravenous drug abuse. All patients underwent blood analysis for renal function. CT was be done for all the patients (contrast enhanced/non-contrast).
Technique of CT study
Patients were asked to be fasting for 4 hours before the CT study. Prior to the contrast study in suitable patients who had normal renal function tests and no contraindication to contrast administration, the risks of intravenous contrast injection was explained and consent obtained. An initial antero-posterior scanogram was obtained in supine position with patient holding the breath. Axial plain sections of thickness 5mm were taken from the level of lung base to ischial tuberosity.
Plain scan was followed by contrast enhanced scan in suitable patients. For those patients in whom contrast could not be administered NCCT was performed, Careful consideration of pathological changes is necessary in selection of CT technique for detecting pathological changes. The protocol in present study included pre and post contrast CT scan.
Image analysis
After the image acquisition, they were sent for reporting by senior radiologists. Once the presence or absence of renal inflammation was confirmed, their characterization including location, laterality, distribution, perinephric spread and complications were identified and specified.
Results
Present study is a descriptive study comprising of 60 patients and was conducted within the period between November 2017 to September 2019 in the Department of Radiology, Sree Balaji Medical College and Hospital.
Demographics
As described in Table 1 and Figure 1 the minimum age was 17 years and the maximum was 88 years with mean of 50.2 years and standard deviation of 15.2 years. Renal infections were found to be more common in older age groups with maximum patients (28%) within age group of 51-60 years.
| Frequency | Percent | |
|---|---|---|
| Upto 30 yrs. | 8 | 16 |
| 31-40 yrs. | 4 | 8 |
| 41-50 yrs. | 13 | 26 |
| 51-60 yrs. | 14 | 28 |
| Above 60 yrs. | 11 | 22 |
| Total | 50 | 100 |
Table 1: Age distribution of renal infections.
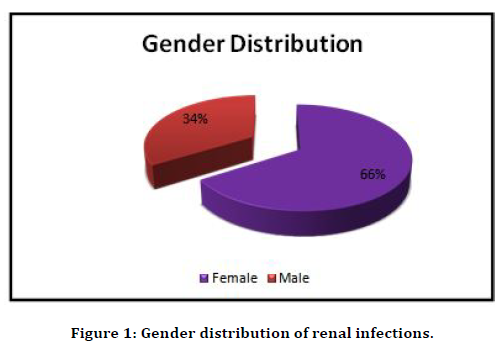
Figure 1. Gender distribution of renal infections.
NCCT shows foci of hyperdensity in the lower pole of right kidney. Perinephric fat stranding and renal facial thickening seen. CECT shows delayed excretion of contrast in right kidney (Figure 2). Figure 3 shows the distribution of immunosuppression.
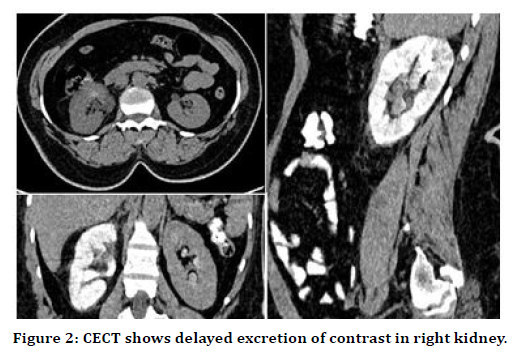
Figure 2. CECT shows delayed excretion of contrast in right kidney.
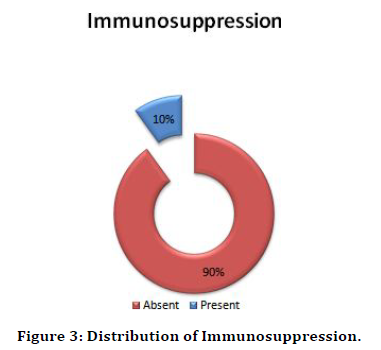
Figure 3. Distribution of Immunosuppression.
The study included two patients with congenital renal anomalies namely autosomal dominant polycystic kidney disease and horseshoe kidney which accounted for 4% of study population adding to the risks factors. This is depicted in Table 2 and Figure 4. Least common complaint was found to be hematuria seen in 17 patients (34%) as seen in Table 3 and Figure 5. Intravenous pyelography shows nonfunctioning calcified left, right kidney (Figure 6). As evident in Table 4 and Figure 7, perinephric fat stranding was closely followed by renal facial thickening seen in 43 patients (86%). CECT shows heterogenous enhancing lesion in antero-medial aspect of posterior cortex of right kidney in mid/ lower pole. It is seen abutting the abscess in the proximal right psoas muscle (Table 5 and Figure 8).
| Congenital renal anomalies | Frequency | Percent |
|---|---|---|
| Absent | 48 | 96 |
| Present | 2 | 4 |
| Total | 50 | 100 |
Table 2: Distribution of congenital anomalies.
| Hematuria | Frequency | Percent |
|---|---|---|
| Absent | 33 | 66 |
| Present | 17 | 34 |
| Total | 50 | 100 |
Table 3: Distribution of symptom of hematuria.
| Frequency | Percent | |
|---|---|---|
| Absent | 7 | 14 |
| Present | 43 | 86 |
| Total | 50 | 100 |
Table 4: Distribution of renal fascia thickening.
| CT | Frequency | Percent |
|---|---|---|
| Positive | 47 | 94 |
| Negative | 3 | 6 |
| Total | 50 | 100 |
Table 5: Distribution of positive CT diagnosis.
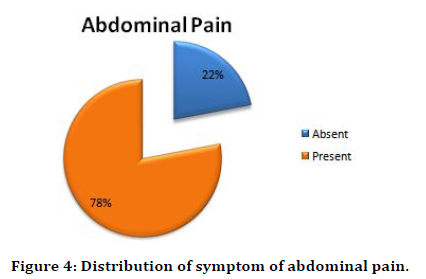
Figure 4. Distribution of symptom of abdominal pain.
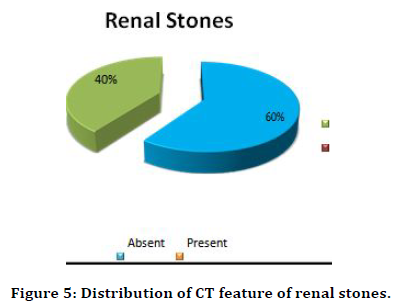
Figure 5. Distribution of CT feature of renal stones.
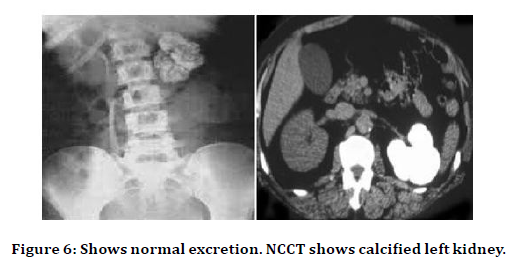
Figure 6. Shows normal excretion. NCCT shows calcified left kidney.
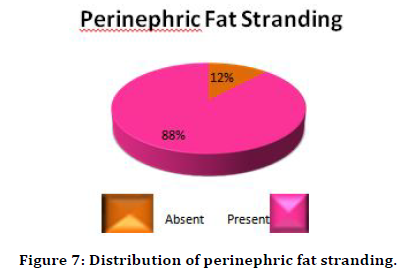
Figure 7. Distribution of perinephric fat stranding.
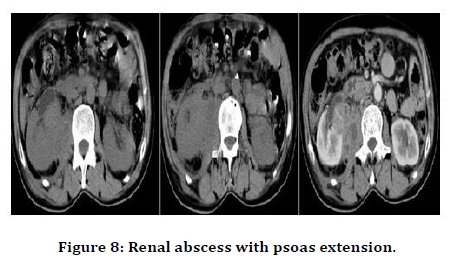
Figure 8. Renal abscess with psoas extension.
Discussion
The present study is a descriptive study of 50 patients from the period of November 2017 to September 2019 which strives to illuminate the features of renal infection including Acute pyelonephritis (focal/ diffuse), Chronicpyelonephritis (focal/ diffuse), Xanthogranulomatous pyelonephritis, Emphysematous pyelonephritis, Renaltuberculosis, Pyonephrosis, Renal abscess and Pararenal abscess. The study included 60 patients who were referred to Department of Radiology in Sree Balaji Medical College from various departments (Urology, Nephrology, General Surgery, General Medicine) for radiological evaluation of clinical symptoms indicative of renal infection. CT(non-contrast or contrast-enhanced) was done for all patients.
The minimum age was 17 years and the maximum was 88 years. In present study renal infections were found to be more common in older age groups with maximum patients (28%) within age group of 51-60 years. This is similar to the findings by Lim et al. [8].
The study included 33 females (66%) and 17 males (34%), showing renal infection being more common in females. This is similar to study by Kassem et al. [9], while in s6tudy by Lim S.K. the infection was found to be more common in males. In another study by Dhamotharan et al. [10], renal infection was found to be more common in females as well.
Certain risk factors were taken into consideration which have been observed to be of significance for the development of renal infections. These included Diabetes mellitus which was found to be most common, seen in about 30 patients (60%). This is similar to study by Lim S.K et al. in his study of hundred and thirty patients out of which 97.9% had diabetes mellitus. Tandogdu et al. [11] stated the importance of immunosuppression as a risk factor in developing renal infection in patients with diabetes and renal transplant. In present study diabetes mellitus was followed by immunosuppression due to various causes such as chemotherapy, chronic steroids, organ transplant patients, HIV infection and was seen in 5 patients (10%). The present study included only two patients with congenital renal anomalies namely autosomal dominant polycystic kidney disease and horseshoe kidney which accounted for 4% of study population adding to the risks factors. Bo-Kyung et al. and Glodny et al. [12,13] in their study showed no statistical significance between horseshoe kidney and renal infections. Bhandarkar et al. [14] in a retroscopic study on 20 patients with horseshoe kidney found significant association with renal infection and horseshoe kidney.
Lantinga et al. [15] in their study identified renal infection as an important complication in patients with autosomal dominant polycystic kidney disease. Choelho et al. [16] has documented difficulty in diagnosis of renal and perinephric abscess since the patients presented with vague symptoms of long duration which did not correlate with severity. The spectrum of clinical symptoms is similar to the present study with different frequency, but burning micturition followed by fever was found to be the commonest symptom in Choelho et al. [16] and Kassem et al. [9].
The patients included in the present study had renal clinical symptoms with commonest being fever seen in 44 patients (88%), followed by abdominal pain and dysuria both accounting for 78% of patients (39 patients). Least common complaint was hematuria seen in 17 patients (34%). In our study most patients had symptoms duration of more than 15 days (60%) which inturn reflects delay in recognition of perinephric and renal abscess. Choelho et al16 has noted similar delays. Considerable similarities with Choelho et al.[16] and Kassem et al.[9] study were found as regards patient characteristics, predisposing conditions and localisation.
Majority of patients underwent medical treatment (70%). Two patients, one with diagnosis of emphysematous pyelonephritis and another one with xanthogranulomatous pyelonephritis underwent nephrectomy.14% patients underwent percutaneous drainage and 12% underwent surgical treatment similar to the Kassem et al. [9]study.
Conclusion
In the present study we conclude that CT plays a vital role in diagnosis of various Renal Infections, the effect they have on renal function and the associated complications. The present study we illuminate the features of renal infection including Acute pyelonephritis , Chronic pyelonephritis, Xanthogranulomatous pyelonephritis, Emphysematous pyelonephritis, Renal tuberculosis, Pyonephrosis , Renal abscess and Para-renal abscess.
We have managed to predict that patients with complaints of flank pain, dysuria, recurrent urinary tract infections, and fever lasting for duration of 15 days or more should undergo contrast enhanced CT as long as there are no contraindications for contrast administration. Whereas patients with contraindication to CT contrast administration can benefit from noncontrast CT scan in evaluation of parenchymal calcification, calculi, obstructed collecting system which might require urgent drainage and decompression or gas within the parenchyma which requires emergency treatment.
Patients with uncontrolled diabetes mellitus with history of recurrent urinary tract infections or renal calculi, symptoms of flank pain, dysuria and fever, should be considered as high risk. These patients should be closely followed up with contrast enhanced or non-contrast CT scan, depending on their renal function.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Das CJ, Ahmad Z, Sharma S, et al. Multimodality imaging of renal inflammatory lesions. World J Radiol 2014; 6:865–873.
- Kawashima A, Sandler CM, Goldman SM. Imaging in acute renal infection. BJU Int 2000; 86:70-79.
- Loffroy R, Guiu B, Watfa J, et al. Xanthogranulomatous pyelonephritis in adults: Clinical and radiological findings in diffuse and focal forms. Clin Radiol 2007; 62:884-90.
- Quaia E, Martingano P, Cavallaro M, et al. Diagnostic Imaging; Multislice CT urography characterizes renal TB. 2011.
- Gardiner RA, Gwynne RA, Roberts SA. Perinephric abscess. BJU Int 2011; 3:20-23.
- Geeting GK, Shaikh N. Renal abscess. J Emerg Med 2006; 31:99-100.
- Demertzis J, Menias CO. State of the art: Imaging of renal infections. Emerg Radiol 2007; 14:1322.
- Lim SK, Foo Cheong NG. Acute Pyelonephritisand renal abscesses in adults-correlating clinical parameterswith radiological (computer tomography)severity. Ann Acad Med Singapore 2011; 40:407-13.
- Kassem TW. Role of multidetector CT in assessment of inflammatory renal diseases. Med J Cairo Univ 2016; 84.
- Dhamotharan VM, Ramadurai S, Gopalan S, et al. Study of the clinical profile of patients with CT proven acute pyelonephritis in a tertiary care hospital. Med Res Chron 2016; 3:64–68.
- Tandogdu Z, Cai T, Koves B, et al. Urinary tract infections in immunocompromised patients with diabetes, chronic kidney disease, and kidney transplant. Eur Urol Focus. 2016; 2:394-39.
- Je BK, Kim HK, Horn PS. Incidence and spectrum of renal complications and extrarenal diseases and syndromes in 380 children and young adults with horseshoe kidney. Am J Roentgenol 2015; 205:1306-14.
- Glodny B, Petersen J, Hofmann KJ, et al. Kidney fusion anomalies revisited: clinical and radiological analysis of 209 cases of crossed fused ectopia and horseshoe kidney. BJU Int 2009; 103:224-235.
- Bhandarkar KP, Kittur DH, Patil SV, et al. Horseshoe kidney and associated anomalies: Single institutional review of 20 cases. Afr J Paediatr Surg 2018; 15:104-107.
- Lantinga MA, Casteleijn NF, Geudens A, et al. Management of renal cyst infection in patients with autosomal dominant polycystic kidney disease: A systematic review. Nephrol Dialysis Transplantation 2017; 32:144–150.
- Coelho RF, Schneider-Monteiro ED, Mesquitaj L, et al. Renal and perinephric abscesses: Analysis of 65consecutive cases. World J Surg 2007; 31:431-6.
Author Info
Sanjivanee Ingole and Prabakaran M*
Department of Radio Diagnosis, Sree Balaji Medical College & Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Sanjivanee Ingole, Prabakaran M, CT Evaluation of Infective Renal Pathologies, J Res Med Dent Sci, 2021, 9 (4): 337-342.
Received: 20-Mar-2021 Accepted: 08-Apr-2021
