Research - (2022) Volume 10, Issue 6
Correlation of Periapical Lesions among Diabetic vs. Non Diabetic Patients
Jagadheeswari Ramamoorthy and Mahalakshmi J*
*Correspondence: Mahalakshmi J, Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences (SIMATS), Saveetha University, India, Email:
Abstract
Aim: To study the correlation of periapical lesions among Diabetic vs. Non diabetic patients Introduction: Periapical lesions are among the most frequently occurring pathological lesions of the alveolar bone. They occur in relation to the tissues around the apex of a tooth root, the periodontal membrane and the alveolar bone. They are usually the sequelae of pulpal inflammation or necrosis with inflammatory mediators spreading through the apical foramen to initiate a periapical lesion. Materials and method: The data of periapical lesions in Diabetic and Non diabetic patients was retrieved from Dental Information Archiving Software. The sample size was found to be 51. The collected data was tabulated in Excel and analysed with the help of SPSS version 23.0. The statistical tests used were Chi square and correlation analysis. The p value <0.05 was considered statistically significant. Results: Among the total number of patients with periapical lesions, 30% of them were diabetic and the remaining 70% of them were non diabetic. The association between Diabetic status of patients with periapical lesions and the gender of the patients was significant. Conclusion: The percentage of patients with periapical lesions as well as Diabetes was significant. Diabetic male patients had a higher prevalence of periapical lesions than females. The association between Diabetic status of patients with periapical lesions and the gender of the patients was found to be significant.
Keywords
Periapical lesions, Diabetes, Prevalence, Caries, Innovative technology
Introduction
Diabetes mellitus is considered a group of complex metabolic disorders caused due to deficiency in insulin secretion caused by dysfunction of pancreatic β-cell and/ or insulin resistance in liver and muscle [1]. The impact of Diabetes mellitus on periapical lesions, it’s a etiology and pathogenesis are needed to be analysed at molecular level. Dental Pulp of patients with Diabetes mellitus may have the tendency to limit collateral circulation, impaired immune response, increased risk of acquiring pulpal diseases or necrosis of the pulp. In molecular pathology, hyperglycemia may also be a stimulus for bone resorption, which inhibits differentiation of osteoblasts and reduces bone recovery [1,2].
Knowledge about how diabetes affects systemic and oral health has an everlasting importance, because it's going to imply not only systemic complications but also a better risk of oral diseases with a significant effect on pulp and periapical tissue. Endodontic treatment of diabetic patients with root canal infections is related to a decrease in success, and these patients may have increased flare-ups [3,4]. They must have endodontic treatment supported by careful assessments and effective antimicrobial regimens of the basic canal. However the association between poorly controlled diabetes and periapical lesions remains unclear [5].
Root canal treatment in patients with Diabetes mellitus should be performed using controlled strategies to stop dissemination of microorganisms through the utilization of intracanal disinfectants and decontamination before crown-down instrumentation. Nevertheless, these interventions are preventive measures [6]. Besides management, it's relevant in cases of uncontrolled or poorly controlled diabetes in patients who need dental treatment that the glycaemic control has to be established or the procedure has to be subject to medical clearance [7]. Antibiotic therapy must be adopted in emergency cases such as presence of oral infection/ dentoalveolar surgery to succeed in a minimal potential for postoperative infections and delayed wound healing. For adult patients with controlled diabetes and absence of systemic complications, dental treatment should be an equivalent as for nondiabetic patient treatment, and antibiotics must be prescribed only in high-risk situations, such as an acute oral infection [8].
Our team has extensive knowledge and research experience that has translated into high quality publications [9-28]. The aim of the study is to study the correlation of periapical lesions among Diabetic vs. Non diabetic patients.
Materials and Methods
This is a Retrospective cross sectional study conducted in a University setting. The study setting had certain advantages like flexibility in data collection and less expenditure. However it had few disadvantages as it is an unicentric study and has geographical limitations. The ethical approval for the current study was obtained from the Institutional Review Board. The data of patients diagnosed with periapical lesions were retrieved from the case sheets of patients. The required data from August 2020 to January 2021 were collected and reviewed. The sample size was found to be 51. The inclusion criteria for the study were patients with periapical lesions and Diabetes mellitus and those who had undergone endodontic or surgical treatment. Exclusion criteria were the incomplete data and were excluded from the study.
The necessary data such as Age, Gender and the Diabetic status of patients with periapical lesions were collected and tabulated in Excel. The data was cross verified by the analyzer. The tabulated data from Excel was imported to SPSS version 23.0 for statistical analysis. The data was represented by the means of bar graphs and the statistical tests used were Chi square and correlation analysis. The correlation between periapical lesions among Diabetic vs. Non diabetic patients were analysed. Statistical significance was set at p<0.05.
Results
The data of patients with periapical lesions was collected from DIAS. Patients were grouped based on their Age, gender and diabetic status. The data was taken from August 2020 to January 2021. 56% of the patients who had periapical lesions were males and 44% of patients were females (Figure 1). 22% of patients belong to the 20-40 years age group, 58% of patients belong to the 40-60 years age group and 20% of patients belong to the 60-80 years age group (Figure 2). Among the total number of patients with periapical lesions, 30% of them were diabetic and the remaining 70% of them were non diabetic (Figure 3). Among the diabetic patients who had periapical lesions, 18% of them were males and 12% of them were females. Among non-diabetic patients who had periapical lesions, 38% of them were males and 32% of them were females. The association between Diabetic status of patients with periapical lesions and the gender of the patients was significant (p<0.05) (Figure 4). Among the diabetic patients who had periapical lesions, 4% belonged to the 20-40 years age group, 20% belonged to the 40-60 years age group and 6% belonged to the 60-80 years age group. Among non-diabetic patients who had periapical lesions, 18% belonged to the 20-40 years age group, 38% belonged to the 40-60 years age group and 14% belonged to the 60- 80 years age group. The association between Diabetic status of patients with periapical lesions and their age group was not significant (Figure 5).
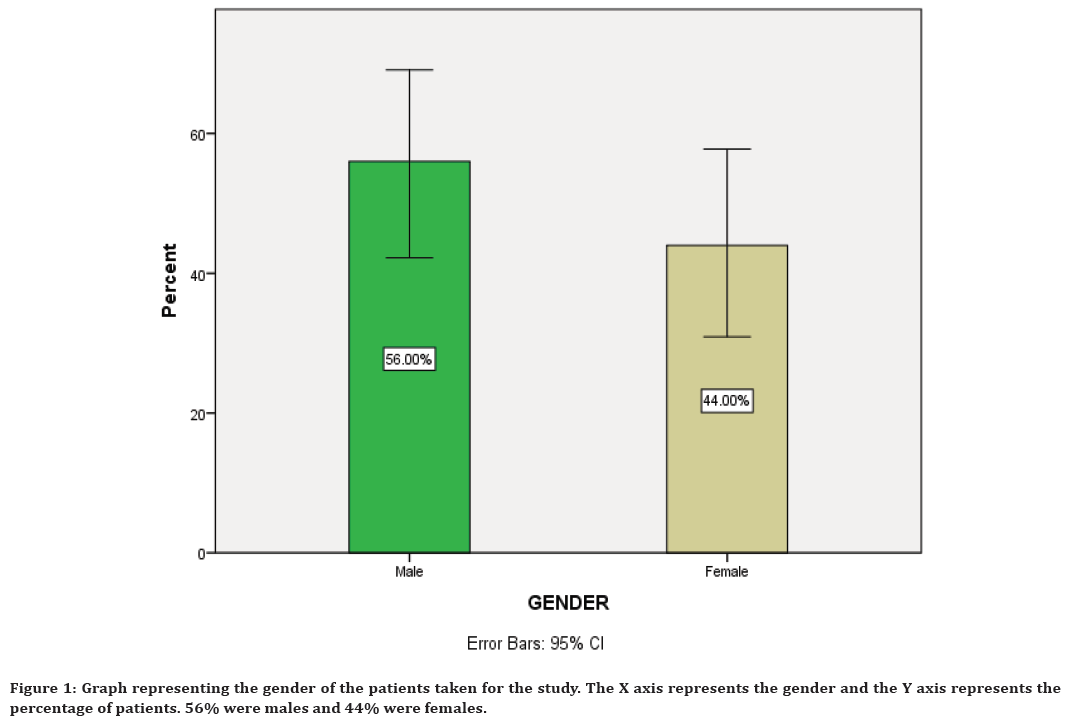
Figure 1. Graph representing the gender of the patients taken for the study. The X axis represents the gender and the Y axis represents the percentage of patients. 56% were males and 44% were females.
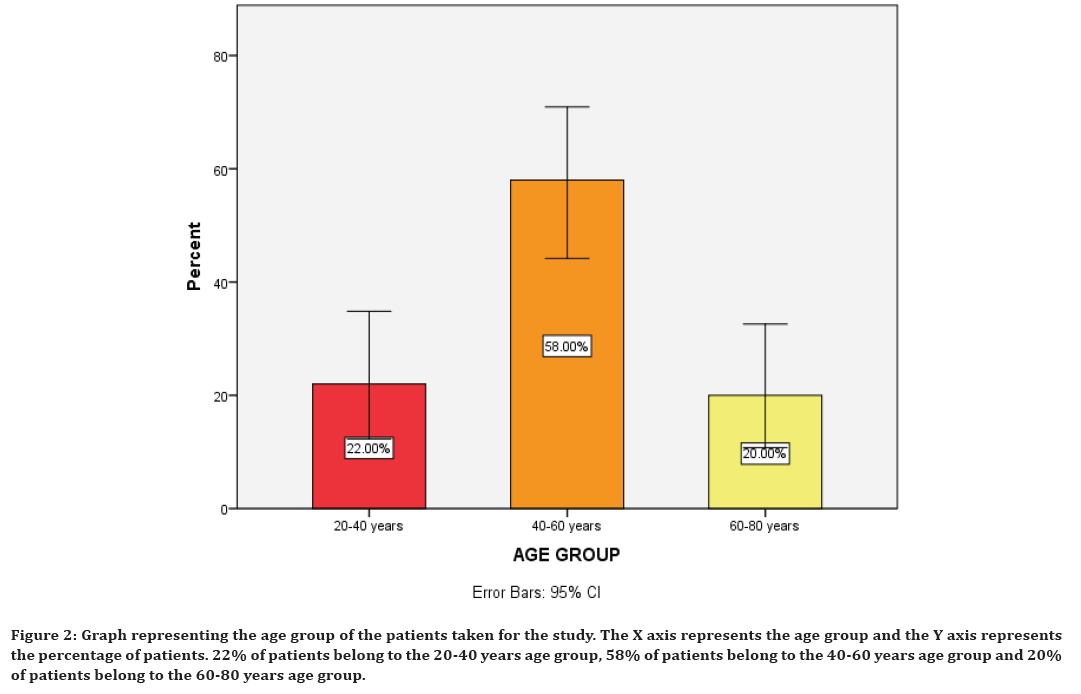
Figure 2. Graph representing the age group of the patients taken for the study. The X axis represents the age group and the Y axis represents the percentage of patients. 22% of patients belong to the 20-40 years age group, 58% of patients belong to the 40-60 years age group and 20% of patients belong to the 60-80 years age group.
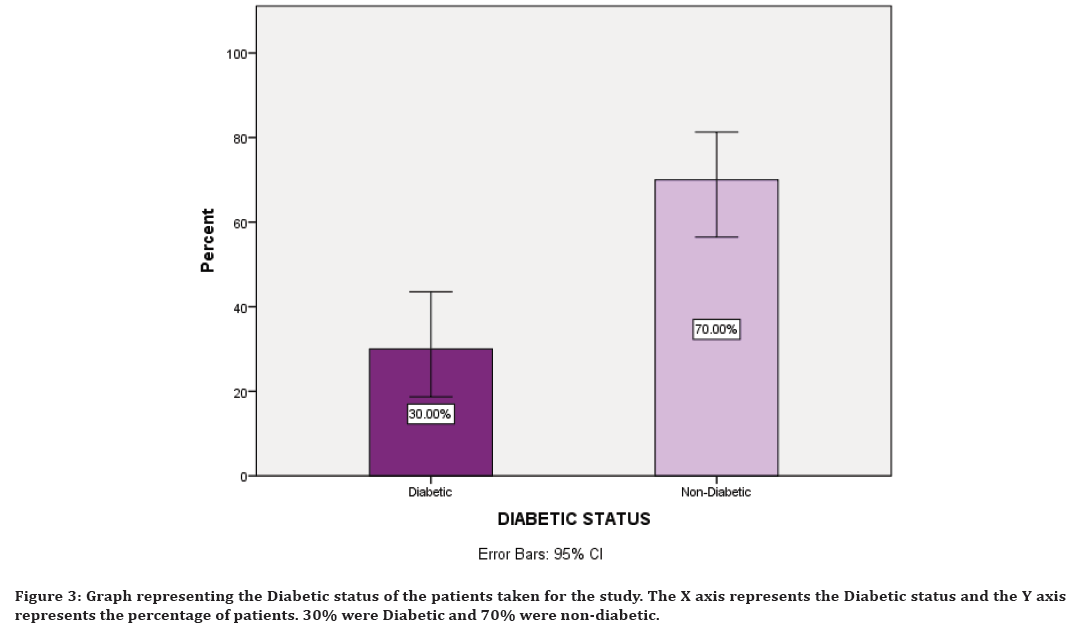
Figure 3. Graph representing the Diabetic status of the patients taken for the study. The X axis represents the Diabetic status and the Y axis represents the percentage of patients. 30% were Diabetic and 70% were non-diabetic.
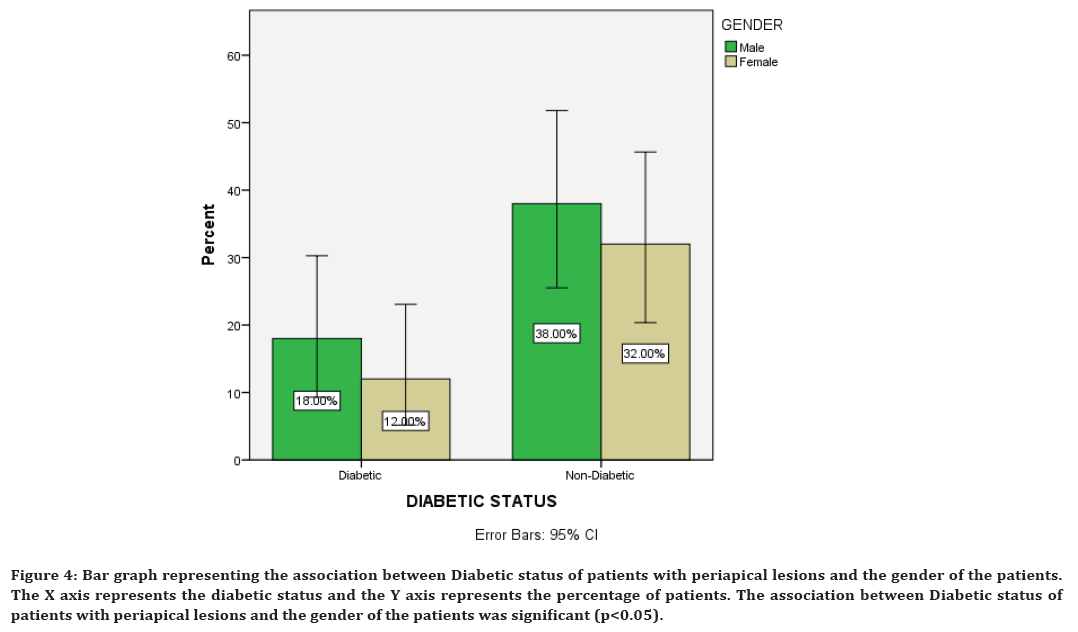
Figure 4. Bar graph representing the association between Diabetic status of patients with periapical lesions and the gender of the patients. The X axis represents the diabetic status and the Y axis represents the percentage of patients. The association between Diabetic status of patients with periapical lesions and the gender of the patients was significant (p<0.05).
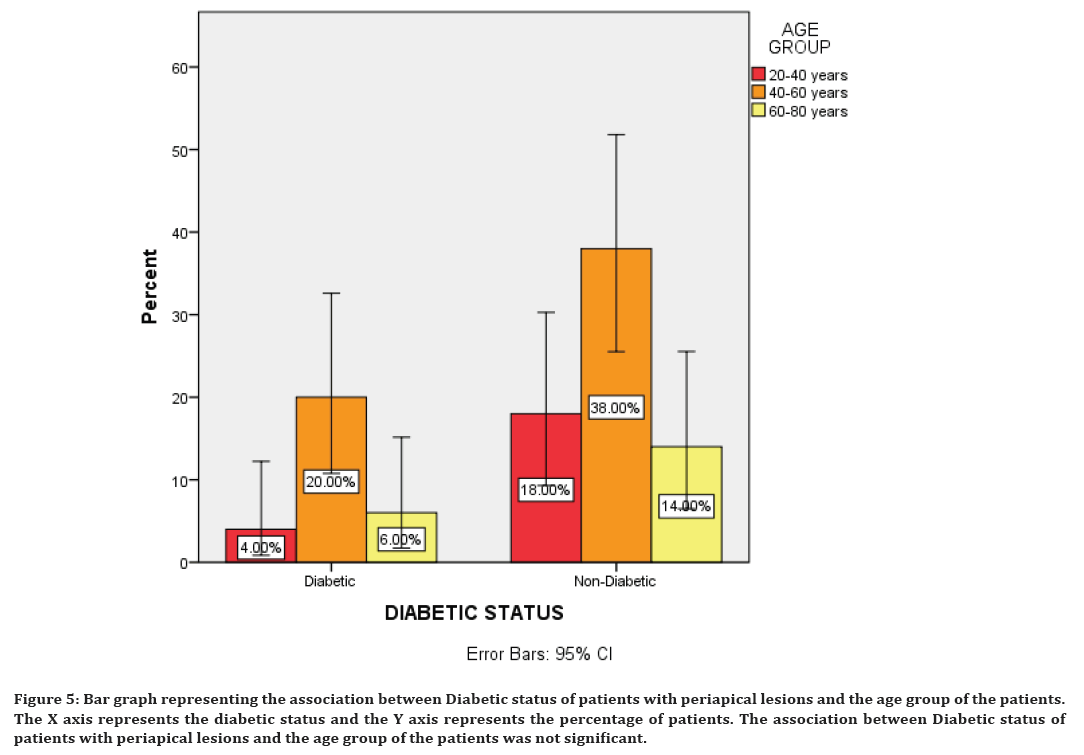
Figure 5. Bar graph representing the association between Diabetic status of patients with periapical lesions and the age group of the patients. The X axis represents the diabetic status and the Y axis represents the percentage of patients. The association between Diabetic status of patients with periapical lesions and the age group of the patients was not significant.
Discussion
Diabetes mellitus may interfere in dental pulp healing, because of the inhibition of Dentin bridge formation and an increase in pulp inflammation after pulp exposure sealed with Mineral Trioxide aggregate. Evidence of reduced immune response to pathogens in periapical tissue besides an increased susceptibility to residual lesions after root canal treatment was found among Diabetic patients. In some previous studies they found a higher prevalence of periapical lesions in Diabetic patients when compared to Non diabetic patients [29,30].
In this study, Male diabetic patients were found to have a higher incidence of periapical lesions than female diabetic patients. Periapical cysts have been reported as the most prevalent periapical lesion of the jaw. In animal models it was also found that Diabetes mellitus interferes in the healing of the pulp tissue. Uncontrolled diabetes mellitus is also known to increase the clinical rate of Endodontic treatment failure. Studies have also shown increased periapical radiolucency after root canal treatment seen in patients with poor diabetes mellitus control [31].
In nondiabetic patients, microorganisms and their metabolic products from infected or necrotic pulps affect the periapical tissues which lead to a chronic periapical lesion with hard tissue resorption and periodontal ligament destruction. The severity of the periapical tissue-response is directly proportional to the number and virulence of the microorganisms. When pulp microorganisms migrate into the periapical tissue, they are surrounded by polymorph nuclear neutrophils or epithelial plugs, as an immune-inflammatory response against the evolution of the infections [32,33].
With hyperglycemia, polymorph nuclear leukocyte function is decreased, due to problems with chemotaxis, phagocytosis, and leukocyte adherence. This may lead to worsening of infection [34]. In addition, T-cell function appears to be depressed, which can also have numerous systemic effects. While hyperglycemia has been proven to increase chances of infection, the effect on periapical disease is far less conclusive [35]. In previous studies it has been proposed that periapical lesions will not heal, and may actually increase in size following endodontic treatment in uncontrolled diabetic patients [36]. In a 1989 study, it was demonstrated that Swedish people with long-duration insulin-dependent diabetes mellitus (Type 1) have an increased prevalence of endodontically treated teeth with lesions compared to those with shortduration IDDM or those who did not have diabetes [36,37].
Limitations of the Study
This study is limited by a few factors. The sample size can be expanded and it is also a short duration study. Some of the patients may be left undiagnosed. The study also has geographical limitations since it is a hospital setting. However, various difficulties were faced when studying the periapical lesions, which includes doctors or clinicians with variations in levels of knowledge, skill and experience, inconsistencies in judgments and research bias.
Future Scope of the Study
A large sample size of patients from different ethnicities would give better results for the study. Other epidemiological studies covering extended time periods would help in collecting important information and validate the findings further. The significance of correlation between diabetic status and periapical lesions during the examination of the patient, especially for older adults should be considered. Further studies on periapical lesions should have adequate sample size for an accurate determination of the association between periapical lesions and diabetic status of the patients.
Conclusion
Within the limits of the study, we observed that association between Diabetic status of patients with periapical lesions and the gender of the patients was significant. In this study, male Diabetic patients had a higher prevalence of periapical lesions than females. The percentage of diabetic patients with periapical lesions was significant. As these periapical lesions constitute a potential oral health risk, the issue needs to be addressed in the community by applying screening tools for asymptomatic cases.
Acknowledgement
The authors would like to acknowledge the help & support rendered by the Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University for their constant assistance with the research.
Funding
The present project is sponsored by Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University and Ashok Leyland Private Limited, Chennai.
Conflict of Interest
None declared.
References
- Gupta A, Aggarwal V, Mehta N, et al. Diabetes mellitus and the healing of periapical lesions in root filled teeth: A systematic review and meta-analysis. Int Endod J 2020; 53:1472–84.
- Brignardello-Petersen R. Insufficient evidence for the association between diabetes mellitus and healing of periapical lesions. J Am Dent Assoc 2017; 148:e198.
- Segura-Egea JJ, Martín-González J, Cabanillas-Balsera D, et al. Association between diabetes and the prevalence of radiolucent periapical lesions in root-filled teeth: Systematic review and meta-analysis. Clin Oral Investig 2016; 20:1133–1141.
- Shlyakova AA, Strongin LG, Kudykin MN, et al. Clinical and pathogenetic features of lesions of the lower extremities in patients with type 2 diabetes mellitus and chronic venous insufficiency. Diabetes Mellitus 2016; 19:212–220.
- Uğur Aydın Z, Ocak MG, Bayrak S, et al. The effect of type 2 diabetes mellitus on changes in the fractal dimension of periapical lesion in teeth after root canal treatment: A fractal analysis study. Int Endod J 2021; 54:181–189.
- Ruiz XF, Duran-Sindreu F, Shemesh H, et al. Development of periapical lesions in endodontically treated teeth with and without periodontal involvement: A retrospective cohort study. J Endod 2017; 43:1246–1249.
- Smadi L. Apical periodontitis and endodontic treatment in patients with type II diabetes mellitus: Comparative cross-sectional survey. J Contemp Dent Pract 2017; 18:358–362.
- Al-Zahrani MS, Abozor BM, Zawawi KH. The relationship between periapical lesions and the serum levels of glycosylated hemoglobin and C-reactive protein in type 2 diabetic patients. Saudi Med J 2017; 38:36–40.
- Muthukrishnan L. Imminent antimicrobial bioink deploying cellulose, alginate, EPS and synthetic polymers for 3D bioprinting of tissue constructs. Carbohydr Polym 2021; 260:117774.
- PradeepKumar AR, Shemesh H, Nivedhitha MS, et al. Diagnosis of vertical root fractures by cone-beam computed tomography in root-filled teeth with confirmation by direct visualization: A systematic review and meta-analysis. J Endod 2021; 47:1198–1214.
- Chakraborty T, Jamal RF, Battineni G, et al. A review of prolonged post-COVID-19 symptoms and their implications on dental management. Int J Environ Res Public Health 2021; 18.
- Muthukrishnan L. Nanotechnology for cleaner leather production: A review. Environ Chem Lett 2021; 19:2527–2549.
- Teja KV, Ramesh S. Is a filled lateral canal-A sign of superiority? J Dent Sci 2020; 15:562.
- Narendran K, Jayalakshmi, Ms N, et al. Synthesis, characterization, free radical scavenging and cytotoxic activities of phenylvilangin, a substituted dimer of embelin. J Pharm Sci 2020; 82.
- Reddy P, Krithikadatta J, Srinivasan V, et al. Dental caries profile and associated risk factors among adolescent school children in an urban south-Indian City. Oral Health Prev Dent 2020; 18:379–386.
- Sawant K, Pawar AM, Banga KS, et al. Dentinal microcracks after root canal instrumentation using instruments manufactured with different NiTi alloys and the SAF system: A systematic review. Adv Sci Inst Ser E Appl Sci 2021; 11:4984.
- Bhavikatti SK, Karobari MI, Zainuddin SLA, et al. Investigating the antioxidant and cytocompatibility of Mimusops elengi Linn extract over human gingival fibroblast cells. Int J Environ Res Public Health 2021; 18.
- Karobari MI, Basheer SN, Sayed FR, et al. An In Vitro stereomicroscopic evaluation of bioactivity between neo MTA Plus, Pro Root MTA, biodentine & glass ionomer cement using dye penetration method. Materials 2021; 14.
- Rohit Singh T, Ezhilarasan D. Ethanolic extract of Lagerstroemia speciosa (L.) Pers., Induces apoptosis and cell cycle arrest in HepG2 cells. Nutr Cancer 2020; 72:146–156.
- Ezhilarasan D. MicroRNA interplay between hepatic stellate cell quiescence and activation. Eur J Pharmacol 2020; 885:173507.
- Romera A, Peredpaya S, Shparyk Y, et al. Bevacizumab biosimilar BEVZ92 versus reference bevacizumab in combination with FOLFOX or FOLFIRI as first-line treatment for metastatic colorectal cancer: A multicentre, open-label, randomised controlled trial. Lancet Gastroenterol Hepatol 2018; 3:845–855.
- Raj RK. β‐Sitosterol‐assisted silver nanoparticles activates Nrf2 and triggers mitochondrial apoptosis via oxidative stress in human hepatocellular cancer cell line. J Biomed Material Res 2020; 108:1899-1908.
- Vijayashree Priyadharsini J. In silico validation of the non-antibiotic drugs acetaminophen and ibuprofen as antibacterial agents against red complex pathogens. J Periodontol 2019; 90:1441–1448.
- Priyadharsini JV, Vijayashree Priyadharsini J, Smiline Girija AS, et al. In silico analysis of virulence genes in an emerging dental pathogen A. baumannii and related species. Arch Oral Biol 2018; 9493–98.
- Uma Maheswari TN, Nivedhitha MS, Ramani P. Expression profile of salivary micro RNA-21 and 31 in oral potentially malignant disorders. Braz Oral Res 2020; 34:e002.
- Gudipaneni RK, Alam MK, Patil SR, et al. Measurement of the maximum occlusal bite force and its relation to the caries spectrum of first permanent molars in early permanent dentition. J Clin Pediatr Dent 2020; 44:423–428.
- Chaturvedula BB, Muthukrishnan A, Bhuvaraghan A, et al. Dens invaginatus: A review and orthodontic implications. Br Dent J 2021; 230:345–350.
- Kanniah P, Radhamani J, Chelliah P, et al. Green synthesis of multifaceted silver nanoparticles using the flower extract of Aerva lanata and evaluation of its biological and environmental applications. Chemistry Select 2020; 5:2322.
- Rudranaik S, Nayak M, Babshet M. Periapical healing outcome following single visit endodontic treatment in patients with type 2 diabetes mellitus. J Clin Exp Dent 2016; 8:e498–504.
- Kosanwat T, Poomsawat S, Kitisubkanchana J. Non-endodontic periapical lesions clinically diagnosed as endodontic periapical lesions: A retrospective study over 15 years. J Clin Exp Dent 2021; 586–593.
- Fouad AF, Burleson J. The effect of diabetes mellitus on endodontic treatment outcome: Data from an electronic patient record. J Am Dent Assoc 2003; 134:43–51.
- Metzger Z. Macrophages in periapical lesions. Dent Traumatol 2000; 16:1-8.
- Yan MT. The management of periapical lesions in endodontically treated teeth. Australian Endod J 2006; 32:2-15.
- Valerius NH, Eff C, Hansen NE, et al. Neutrophil and lymphocyte function in patients with diabetes mellitus. Acta Med Scandinavica 2009; 211:463–467.
- Bender IB, Seltzer S, Freedland J. The relationship of systemic diseases to endodontic failures and treatment procedures. Oral Surg Oral Med Oral Pathol 1963; 16:1102-1115.
- Falk H, Hugoson A, Thorstensson H. Number of teeth, prevalence of caries and periapical lesions in insulin-dependent diabetics. Eur J Oral Sci 1989; 97:198–206.
- Britto LR, Katz J, Guelmann M, et al. Periradicular radiographic assessment in diabetic and control individuals. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003; 96:449–452.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Jagadheeswari Ramamoorthy and Mahalakshmi J*
Department of Conservative Dentistry and Endodontics, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences (SIMATS), Saveetha University, Chennai, Tamil Nadu, IndiaReceived: 26-May-2022, Manuscript No. JRMDS-22-65013; , Pre QC No. JRMDS-22-65013 (PQ); Editor assigned: 28-May-2022, Pre QC No. JRMDS-22-65013 (PQ); Reviewed: 14-Jun-2022, QC No. JRMDS-22-65013; Revised: 17-Jun-2022, Manuscript No. JRMDS-22-65013 (R); Published: 24-Jun-2022
