Research - (2021) Volume 9, Issue 11
Correlation of Mental Foramen Position and Type of Occlusion among Saudi Orthodontic PatientsâA Radiographic Study
*Correspondence: Ahmed Abdullah Saeed Bahamid, Department of Preventive Dentistry, College of Dentistry, Riyadh Elm University, Riyadh, Saudi Arabia, Email:
Abstract
Background: The knowledge of anatomy of mental foramen and its surrounding structures is of great significance while administering local anesthesia either for diagnostic, surgical or operative procedures like performing periapical surgery in the mental region of the mandible. Aim- This study strives to determine the shape, position, symmetry of MF and its continuity with the inferior dental canal (IDC) on a digital panoramic view and to find its correlation with Angle’s molar relations among the orthodontic patients in Saudi Arabia. This study also focuses on determining the correlation of inter-foramen distance in both genders in Riyadh population of Saudi Arabia. Subjects and methods- Panoramic radiographs (N=315) of orthodontic patients aged between 18-45 years seeking care at three different clinics of Riyadh Elm University were examined in this study. The assessment of occlusion was based on Angle’s molar relationships. The data obtained was then analyzed statistically. Result- A total of (N=315) panoramic radiographs belonging to the patients were screened for the mental foramen parameters. Most of the panoramic radiographs belonged to the female patients 176 (55.9%) having Saudi nationality 310 (98.4%) undergoing fixed orthodontic treatment 314 (99.7%). Majority of the radiographs were belonged to the patients having Angle’s class I occlusion. Mental foramen showed significant changes in position, symmetry, shape and continuity across different class of malocclusion, however, no such differences were observed in regards to gender. Conclusion- Accurate and adequate knowledge is important for dental practitioners regarding variations in anatomical and morphological appearance and position of the Mental Foramen for the isolation of mental nerves and vessels so as to perform safer mental nerve blocks in surgical interventions. The commonest MF position was aligned between the 1st and 2nd premolars.
Keywords
Anatomy, Mental foramen, Malocclusion, Orthodontic treatment, Angle’s molar relationship
Introduction
The mental foramen (MF) is a funnel-shaped aperture on the lateral side of the mandible's body at the terminal of the mental canal, which is the anterior limit of the inferior alveolar canal [1]. The opening is directed outward, upward, and posteriorly. The mental bundle passes through the MF and supplies sensory innervations and blood supply to the soft tissues of the chin, lower lip, and gingiva on the same mandibular side. The location of the MF is crucial in clinical dentistry for delivering local or regional anaesthetic, conducting orthodontic tooth movement/surgery, conducting periapical surgery, and implant insertion in the mandible's mental area. Sometimes the MF is mistaken as a radiolucent lesion in the periapical region of the mandibular premolar teeth [2]. In orthodontic treatment, mental paraesthesia is an uncommon occurrence. Nonetheless, the research indicates that there are clinical scenarios in which there is a higher risk of developing mental paraesthesia during orthodontic treatment, particularly when fixed appliances are employed [3].
The location of the MF has been observed to vary in various genders and ethnic groups with varied craniofacial skeletal and dental occlusion [3]. According to research on different populations, the most prevalent site of MF is its alignment with the second premolar, followed by its position between the first and second premolars [4]. The most often used diagnostic modality is panoramic radiography. The benefit of this approach is that it provides for a more exact positioning of the MF in both horizontal and vertical dimensions and provides for a better view of the whole body of the mandible [5].
Until now best to our knowledge, there is lack of information on the correlation between mental foramen and occlusion among patients undergoing orthodontic treatment in Saudi Arabia. Hence there is a need to explore this relationship among orthodontic patients so that the correct diagnosis and appropriate treatment can be done and the positive prognosis can be improved.
Aim of the study
The purpose of this radiographic study is to report any correlation between Angle’s molar relationship and the position of mental foramen bilaterally among orthodontic patients seeking care at university dental clinics in Riyadh City, Saudi Arabia.
Material and Methods
Study design
It was a retrospective analysis of the panoramic radiographs.
Ethical approval
Study approval was obtained from the Research Center of Riyadh Elm University. Data was collected anonymously by considering the file numbers.
Study sample
Panoramic radiographs of orthodontic patients aged between 18-45 years seeking care at three different clinics of Riyadh Elm University were examined in this study.
Sample size
Assuming common position of the mental foramen between first and the second premolar 71.5% cases. The minimum sample size was 315 radiographs with a 5% level of significance and 5% absolute error [6].
Exclusion criteria
• Non-visualization of the mental foramen bilaterally on OPG.
• Presence of impacted premolar.
• Patients with missing teeth and congenitally missing premolar.
• Presence of a radiolucent lesion in the lower jaw anywhere around mental foramen of the mandible.
Recording the position of the mandibular foramen
The position of MF was recorded relative to the adjacent mandibular teeth.
Position 1: anterior to apex of the first premolar. Position 2: at the apex of the first premolar.
Position 3: between the apices of the first and second premolars.
Position 4: The apex of the second premolar.
Position 5: between the apices of the second premolar and the first molar. Position 6: at the mesial half of the first molar
The position of MF was reported on the basis of gender and symmetry or asymmetry. Symmetrical: if mental foramina on both sides had the same anterio-posterior position relative to the teeth.
Asymmetrical: if mental foramina on both sides had different anterio-posterior position relative to the teeth.
Continuity of the foramen was studied on both sides as per Yosue and Brooks classification as: Type I: mental canal is continuous with the mandibular canal.
Type II: foramen is distinctly separated from the mandibular canal. Type III: diffuse with distinct border of foramen.
Type IV: unidentified group.
The shape of MF was recorded as: oval, round and irregular.
The distance between two foramina was measured from their centers. This inter-foramen distance was measured in millimetre using Dental Imaging software.
Angle’s molar relationship classification [7]
Molar relationship was recorded based on the patient’s record at the time of screening.
Class I: Those malocclusions exhibiting normal mesiodistal relation of jaws and dental arches were indicated as normal locking of first permanent molar.
Class II: A distal relation of the lower arch when related to the upper arch, the lower first permanent molar locking more than one-half of a cusp distal to normal relation with the upper permanent molar.
Class III: A mesial relation of the lower arch when related to the upper arch, the lower first molar locking more than one half of a cusp mesial to normal relation with the upper first molar.
All the information was then collected in the excel sheet and was subjected to statistical analysis.
Statistical analysis
A descriptive statistics of frequency distribution and percentages were calculated for the categorical variables. The relationship between categorical variable were assessed using Chi- square test and Fisher’s exact test. A value of P ≤ 0.05 was considered statistically significant. All data was analyzed using the statistical software (SPSS v. 25.0 IBM, Armonk, NY, USA).
Results
A total of (N=315) panoramic radiographs belonging to the patients were screened for the mental foramen parameters. The study characteristics are described in Table 1. Most of the panoramic radiographs belonged to the female patients 176(55.9%) having Saudi nationality 310 (98.4%) undergoing fixed orthodontic treatment 314 (99.7%). Majority of the radiographs were belonged to the patients having Angle’s class I occlusion.
| Characteristics | n | % | |
|---|---|---|---|
| Gender | Male | 139 | 44.10% |
| Female | 176 | 55.90% | |
| Nationality | Saudi | 310 | 98.40% |
| Non-Saudi | 5 | 1.60% | |
| Orthodontic Treatment | Removable | 1 | 0.30% |
| Fixed | 314 | 99.70% | |
| Invisalign | 0 | 0.00% | |
| Angle’s Classification of Occlusion | Class I | 177 | 56.20% |
| Class II | 64 | 20.30% | |
| Class III | 74 | 23.50% | |
| Age in years (mean ± SD) 23.50±5.20 | |||
Table 1: Study characteristics (N=315).
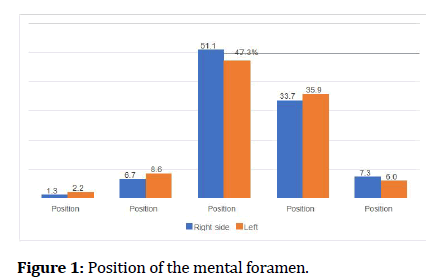
The position, shape and continuity of the mental foramen on both right and left sides are displayed in Table 2. Location of the mental foramen in position 3 (between the apices of the first and second premolars) is common on right 161(51.1%) and left side 149 (47.3%) (Figure 1). Similarly, round shape of the mental foramen was found to common on right 147 (46.7%) and left side 146 (46.3%), followed by irregular and oval shapes. Most of the OPGs showed type I (mental canal is continuous with the mandibular canal) continuity of the mental foramen on right 142 (45.1%) and left 137 (43.5%) followed by type II, type III and type IV.
| Variables | Right side | Left side | |||
|---|---|---|---|---|---|
| Position | Position 1: anterior to apex of the first premolar | 4 | 1.30% | 7 | 2.20% |
| Position 2: at the apex of the first premolar | 21 | 6.70% | 27 | 8.60% | |
| Position 3: between the apices of the first and second premolars | 161 | 51.10% | 149 | 47.30% | |
| Position 4: the apex of the second premolar | 106 | 33.70% | 113 | 35.90% | |
| Position 5: between the apices of the second premolar and the first molar | 23 | 7.30% | 19 | 6.00% | |
| Position 6: at the mesial half of the first molar | 0 | 0.00% | 0 | 0.00% | |
| Shape | Round | 147 | 46.70% | 146 | 46.30% |
| Oval | 26 | 8.30% | 33 | 10.50% | |
| Irregular | 142 | 45.10% | 136 | 43.20% | |
| Continuity | Type I: mental canal is continuous with the mandibular canal | 142 | 45.10% | 137 | 43.50% |
| Type II: foramen is distinctly separated from the mandibular canal | 127 | 40.30% | 130 | 41.30% | |
| Type III: diffuse with distinct border of foramen. | 28 | 8.90% | 30 | 9.50% | |
| Type IV: unidentified group | 18 | 5.70% | 18 | 5.70% | |
Table 2: Mental foramen related information (N=315).
Figure 1: Position of the mental foramen.
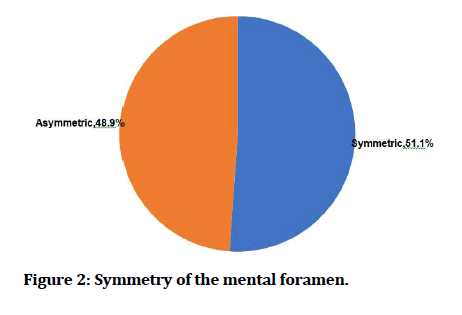
In general, more than half of the mental foramen was symmetric 51.1% and 48.9% were asymmetric (Figure 2). While 196 (62.2%) OPGs showed lower anterior crowding (Table 3).
| Yes | 196 | 62.20% |
| No | 119 | 37.80% |
Table 3: The presence of lower anterior teeth crowding.
Figure 2:Symmetry of the mental foramen.
Mental foramen position, symmetry, shape and continuity did not reveal any significant differences between male and female genders (p>0.05). Whereas mental foramen on left side (p=0.027), symmetry (p=0.003), and continuity of mandibular foramen on right side(p<0.001) and left side (p<0.001) showed significant difference with regards to angle’s classification of occlusion (Table 4).
| Mental foramen | Gender | Angle's classification | ||||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | p | Class I | Class II | Class III | p | ||
| Position Right side | Position 1 | 0.70% | 1.70% | 0.071 | 1.70% | 0.00% | 1.40% | 0.812 |
| Position 2 | 4.30% | 8.50% | 7.30% | 4.70% | 6.80% | |||
| Position 3 | 48.90% | 52.80% | 49.20% | 50.00% | 56.80% | |||
| Position 4 | 41% | 27.80% | 35.60% | 34.40% | 28.40% | |||
| Position 5 | 5.00% | 9.10% | 6.20% | 10.90% | 6.80% | |||
| Position Left side | Position 1 | 2.20% | 2.30% | 0.939 | 2.80% | 1.60% | 1.40% | 0.027 |
| Position 2 | 7.90% | 9.10% | 7.90% | 9.40% | 9.50% | |||
| Position 3 | 49.60% | 45.50% | 44.60% | 39.10% | 60.80% | |||
| Position 4 | 33.80% | 37.50% | 41.20% | 40.60% | 18.90% | |||
| Position 5 | 6.50% | 5.70% | 3.40% | 9.40% | 9.50% | |||
| Symmetry | Symmetric | 54% | 48.90% | 0.369 | 42.90% | 65.60% | 58.10% | 0.003* |
| Asymmetric | 46% | 51.10% | 57.10% | 34.40% | 41.90% | |||
| Shape right side | Round | 45.30% | 47.70% | 0.347 | 46.90% | 54.70% | 39.20% | 0.401 |
| Oval | 10.80% | 6.30% | 7.90% | 9.40% | 8.10% | |||
| Irregular | 43.90% | 46.00% | 45.20% | 35.90% | 52.70% | |||
| Shape left side | Round | 42.40% | 49.40% | 0.302 | 45.80% | 53.10% | 41.90% | 0.695 |
| Oval | 12.90% | 8.50% | 11.30% | 9.40% | 9.50% | |||
| Irregular | 44.60% | 42.00% | 42.90% | 37.50% | 48.60% | |||
| Continuity Right side | Type I | 43.90% | 46.00% | 0.925 | 53.70% | 34.40% | 33.80% | <0.001* |
| Type II | 40.30% | 40.30% | 29.40% | 57.80% | 51.40% | |||
| Type III | 10.10% | 8.00% | 8.50% | 7.80% | 10.80% | |||
| Type IV | 5.80% | 5.70% | 8.50% | 0.00% | 4.10% | <0.001* | ||
| Continuity Left side | Type I | 41.70% | 44.90% | 0.893 | 52.50% | 25.00% | 37.80% | |
| Type II | 41.70% | 40.90% | 29.40% | 64.10% | 50.00% | |||
| Type III | 10.80% | 8.50% | 9.00% | 10.90% | 9.50% | |||
| Type IV | 5.80% | 5.70% | 9.00% | 0.00% | 2.70% | |||
Table 4: Relationship between mental foramen variables with gender and angles classification.
Mental foramen showed significant changes in position, symmetry, shape and continuity across different class of malocclusion. However, no such differences were observed with regards to the gender.
Discussion
The mental foramen (MF) is an important landmark during planning for any surgery. An irritation to the inferior alveolar nerve due to an elongated styloid process during mandibular movement which can results in a progressive loss of sensation in the mental nerve[8]. Hence to prevent such mishap a knowledge of the site of the mental foramen in the patients will allow for accurate delivery of local anesthesia for dental procedures and avoids damage to the nerve in surgical procedures, such as periapical surgery, implantation, cyst enucleation, periodontal surgery, mandibular bony osteotomy [9]. Additionally, good interpretation of anatomical landmarks in oral pathology and forensics can be aided. For all of the above-mentioned reasons, the horizontal location and position of the mental foramen have been studied utilizing panoramic radiographs or dry skulls. With respect to detecting the anatomical structure, the cadaveric dissection methods are more accurate than radiographic methods. It has been suggested that the most common position of MF examined on 525 dry mandibles was in 43.66% located in front of the apex of the root of the second premolar that was position 4[10]. A different position of mental foramen has recently been reported to have existed between the population of different or even of the same geography. In this study, the position of the mental foramen in patients undergoing orthodontic treatment in the Riyadh city population was studied using panoramic radiographs rather than other plane films. Consequently, a more accurate interpretation of the location of the mental foramen in both the horizontal and vertical dimensions was allowed by using panoramic radiographs [11,12].
The patients’ ages were between 18 and 25 years because the position of MF changes with age and loss of alveolar bone. All the patients had permanent set of dentition, because in mixed dentition, permanent tooth buds might obscure the mental foramen. Panoramic radiographs were used in this study because the MF was seen more consistently on the wide field of view in these radiographs than on the periapical, which do not reveal the position of MF if it falls below the edge of the film [13]. Phillips et al demonstrated that the size of the foramen on panoramic radiographs was slightly larger than that reported on periapical radiographs, but they stated that the horizontal position of the MF on panoramic radiographs generally agreed with the position reported on periapical radiographs [11].
In our series of 315 panoramic radiographs, the position of mental foramen was most commonly both in males and females in line with the most commonly were between first and second premolar. No cases were found in positions 6. This present study result coincides with observations made by Ngeow et al. [1]. The previous study showed that 95% of mental foramen was reported the position of the 3 and 4. Studies done on North American and Caucasian populations reported the area between the two premolars as the most common location of the mental foramen[1,14,15]. The present study on the position of mental foramen was inconsistent with findings of Yosue and Brooks, & Gupta and Soni et al. [12,16]. The Panoramic study of position of mental foramen was also observed in Tanzanian adult black male [17], Malay population [1], Brazilian et al. [18], Sankar et al. [19], Malawian mandible [20], Ukoha in southeastern Nigerian[21], Singh et al. [22] in Indian adult human skull, Jasser et al. observed most common position as in line with the longitudinal axis of second premolar followed with location between first and second premolar in radiographs study of Saudi Arabians [23].
The variations in the position of MF can occur due to dental loss and ageing. Green also reported that gender influences the position of MF, which is more anterior in the Caucasoid groups [24]. Moreover, genetics is an important factor in the morphological characteristics of dental structures [11]. According to Yesilyurt et al. the position of MF may vary in different ethnic groups and gender as seen in the present study [25]. The accurate identification and anatomical location of the mental foramen is very important for diagnostic purposes and clinical dentistry. The differences in the bilateral positions of the MF may occur if the MF is funnel shaped in the buccal cortex of the mandible. The mental canal passes from the posterior to the superior border of the mandible. In the present study, round shaped MF was most commonly reported in the study population of Riyadh city. Very few were unidentified, which were excluded from the study. The literature also supports this finding [26]. In the present study, the relationship of the MF position with Angle’s molar was studied as there were reported cases of mental nerve paraesthesia in orthodontically treated cases. The position 3 of the MF was most commonly recorded in Angle’s Classes I and II molar relationship. No case of Angle’s Class III was noted with position 4 of MF. The results were consistent with studies by Gangotri et al. [15] The weakness of the study was the use of panoramic radiographs for localization of the MF, as distortion and magnification factors inherent in the orthopantomogram techniques were not taken into consideration and moreover the study id only from one country, so the results are not highly generalizable. Further multicentric studies with larger population are warranted.
Conclusion
This study well concludes the Correlation between Angle’s molar relation with MF position as significant for Classes I and II, but not for Class III. The most common positions of MF came out to be position number 3 i.e., between the 1st and 2nd premolar. Adding to it, the most common shape of MF was round and symmetric in nature. In context to the continuity of MF with the mandibular foramen, it was continuous on both the sides. Accurate and adequate knowledge is important for dental practitioners regarding variations in anatomical and morphological appearance and position of the Mental Foramen for the isolation of mental nerves and vessels so as to perform safer mental nerve blocks in surgical interventions.
References
- Ngeow WC, Yuzawati Y. The location of the mental foramen in a selected Malay population. J Oral Sci 2003; 45:171–175.
- Al-Faleh W, Zahrni AA. Observer agreement on radiographic assessment of mental foramen appearance in panoramic radiographs. Pak Oral Dent J 2005; 25:225–8.
- Baxmann M. Mental paresthesia and orthodontic treatment. Angle Orthod 2006; 76:533–537.
- Shah PP, Parikh KK, Shah MJ, et al. Radiographic study of mental foramen in a selected Indian population in Kheda district, Gujarat. J Indian Acad Oral Med Radiol 2013; 25:13.
- Verma P, Bansal N, Khosa R, et al. Correlation of radiographic mental foramen position and occlusion in three different Indian populations. West Indian Med J 2015; 64:269.
- Rathod SB, Nimbal AV, Chillalshetti SK, et al. Panoramic Radiographic study on location of mental foramen in patients of orthodontic treatment. South East Asia J Med Sci 2019; 3:1–4.
- Blair ES. A cephalometric roentgenographic appraisal of the skeletal morphology of class i, class ii, div. 1, and class ii, div. 2 (angle) malocclusions. Angle Orthod 1954; 24:106–119.
- Bagoji IB, Hadimani GA, Patil BG, et al. Bilateral elongated styloid process: its anatomical embryological and clinical implications. Int J Med Res Health Sci 2013; 2:273-276.
- Rowe AH. Damage to the inferior dental nerve during or following endodontic treatment. Br Dent J. 1983(5);155(9):306–7.
- Gershenson A, Nathan H, Luchansky E. Mental foramen and mental nerve: changes with age. Acta Anat 1986; 126:21–28.
- Phillips JL, Weller RN, Kulild JC. The mental foramen: 2. Radiographic position in relation to the mandibular second premolar. J Endod 1992; 18:271–274.
- Yosue T, Brooks SL. The appearance of mental foramina on panoramic radiographs. I. Evaluation of patients. Oral Surg Oral Med Oral Pathol 1989; 68:360–364.
- Chandra A, Singh A, Badni M, et al. Determination of sex by radiographic analysis of mental foramen in North Indian population. J Forensic Dent Sci 2013; 5:52–55.
- Shankland WE. The position of the mental foramen in Asian Indians. J Oral Implantol 1994; 20:118–123.
- Gangotri S, Patni VM, Sathwane RS. Radiographic determination of position and symmetry of mental foramen in central Indian Population. J Indian Acad Oral Med Radiol 2011; 23:101.
- Gupta S, Soni J. Study of anatomical variations and incidence of mental foramen and accessory mental foramen in dry human mandibles. Natl J Med Res 2012; 2.
- Fabian FM. Position, shape and direction of opening of the mental foramen in dry mandibles of Tanzanian adult black males. Ital J Anat Embryol Arch Ital Anat Ed Embriologia 2007; 112:169–77.
- Amorim MM, Prado FB, Borini CB, et al. The mental foramen position in dentate and edentulous brazilian’s mandible. Web Sci 2008.
- Sankar DK, Bhanu SP, Susan PJ. Morphometrical and morphological study of mental foramen in dry dentulous mandibles of South Andhra population of India. Indian J Dent Res Off Publ Indian Soc Dent Res 2011; 22:542–546.
- Igbigbi PS, Lebona S. The position and dimensions of the mental foramen in adult Malawian mandibles. West Afr J Med 2005; 24:184–9.
- Ukoha U, Umeasalugo K, Ofoego U, et al. Position, shape and direction of the mental foramen in mandibles in South-Eastern Nigeria. Int J Biomed Res 2013; 4:499.
- Singh R. Study of position, shape, size and incidence of mental foramenand accessory mental foramen in indian adult human skulls. Anat Int J Exp Clin Anat 2011; 5:23–29.
- Jasser NM, Nwoku AL. Radiographic study of the mental foramen in a selected Saudi population. Dento Maxillo Facial Radiol 1998; 27:341–343.
- Green RM. The position of the mental foramen: A comparison between the southern (Hong Kong) Chinese and other ethnic and racial groups. Oral Surg Oral Med Oral Pathol 1987; 63:287–290.
- Yesilyurt H, Aydinlioglu A, Kavakli A, et al. Local differences in the position of the mental foramen. Folia Morphol 2008; 67:32–35.
- Choi KS, Bae YC, Kim DY, et al. A radiographic study of the position and shape of mental foramen in panoramic radiographs. J Korean Acad Oral Maxillofac Radiol 2015; 27:189–201.
Author Info
Department of Preventive Dentistry, College of Dentistry, Riyadh Elm University, Riyadh, Saudi ArabiaCitation: Ahmed Abdullah Saeed Bahamid, Correlation of Mental Foramen Position and Type of Occlusion among Saudi Orthodontic Patients–A Radiographic Study, J Res Med Dent Sci, 2021, 9(11): 194-200
Received: 04-Oct-2021 Accepted: 08-Nov-2021