Research - (2021) Volume 9, Issue 5
Correlation Between the Doppler Study with Fetal Outcome and Analysis of the Association of Abnormal Doppler Velocimetry in Perinatal Outcome
A Padmaja Rani, K Saraswathi and K Vani*
*Correspondence: K Vani, Department of Obstetrics & Gynecology, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email:
Abstract
BA prospective, randomized study was designed to find if there is any correlation between the doppler study with fetal outcome and analysis of the association of abnormal doppler velocimetry in perinatal outcome. In the present study, 46% of them had gestational hypertension, 28% had mild preeclampsia, 24% had severe preeclampsia and 3% had eclampsia. A hundred patients diagnosed to have gestational hypertension with gestational age beyond 26 weeks were studied and subjected to color doppler ultrasonography.
Keywords
Doppler study, Correlation, Perinatal outcome, Eclampsia doppler ultrasonography, Gestational hypertension
Introduction
Depending upon the country, the various Hypertensive disorders constitute 5 -10% of pregnancies. The word Eclampsia derived from a Greek word meaning 'to shine forth' because of the visual phenomena accompanying the condition. The associated seizures were believed to be due to blood poisoning (or) toxins derived from pregnancy-Hence the term Toxemia of Pregnancy. In 1781 Eclampsia was described as a condition associated with seizures. In 1827 it was recognized albuminuria in addition relating to Eclampsia. Later with the advancement of science, the emphasis was laid more on genetic, haematological, biochemical hormonal and immunological explanations. Researchers have concluded that preeclampsia could be due to simple recessive trait. In Doppler velocimetry in Preeclampsia, others in 1986 studied the correlations of severity of preeclampsia with pregnancy outcome. They concluded that when the Uterine Artery Systolic - Diastolic ratio was more than 2.6 during the III trimester, incidence of fetal distress during delivery is high. According to him, about 67% of hypertensive patients with abnormal umbilical blood flow deliver growth retarded babies. Some researchers reported that an increased Uterine artery RI without a notch poorly correlates with adverse fetal outcome. He concluded that hypertensive pregnant women were divided into four groups based on the presence or absence of a Uterine notch or Umbilical artery RI. The presence of both was associated with most severe complications. In his study, perinatal mortality was 21% and 74% of fetuses were growth retarded. Abnormal umbilical artery Doppler velocimetry characterized by absent or reverse end diastolic flow signifying increased impedance has been uniquely associated with fetal growth restrictions. (ACOG 2000). Among the several parameters employed to evaluate the changes in velocity waveforms, the simplest and the most employed is the S/ D ratio. Umbilical artery Doppler velocimetry as a predictor of fetal hypoxia and acidosis at birth. He observed a significant association between the absence of end diastolic flow in umbilical artery and hypoxia and acidosis. The clinical implications of Doppler ultrasound analysis of the Uterine and Umbilical arteries. when abnormal waveforms persist, fetal growth retardation and adverse perinatal outcome are likely. He said about the significance of absent end diastolic velocity in umbilical artery velocity waveforms. According to National Centre for Health Statistics, Gestational hypertension was identified in 3.7 % of pregnancies. It is one of the commonest medical disorders diagnosed by obstetricians in clinical practice2. Gestational Hypertension is a common medical disorder of pregnancy approximately 70% of which are primigravidas. Gestational Hypertension is defined as Blood pressure> 140/90 mmHg for the first-time during pregnancy with no proteinuria, and BP returns to normal within 12 weeks postpartum. So the final diagnosis is made only postpartum. It may have other signs and symptoms of preeclampsia. In Preeclampsia this condition is best described as a pregnancy specific syndrome of reduced organ perfusion secondary to vasospasm and endothelial activation. Chronic Hypertension first diagnosed after 20 weeks gestation and persistent after 12 weeks post-partum.
Despite extensive research, the exact cause of pre-eclampsia remains unknown, and it has been aptly referred to as the 'disease of theories'41. But there are histological evidence which prove that the pathogenesis of the disease involves abnormal development of small uterine vessels. There is incomplete or absence of trophoblastic invasion of the spiral arteries42.Uterine artery blood flow reflects hemodynamic changes that occur at the maternal side of the placenta43. These physiologic changes of the placental bed spiral arteries extend only to the deciduo myometrial junction. In pre-eclampsia the spiral arteries may remain unconverted throughout their decidual and myometrial length. In fetal cerebral circulation in gestational hypertension oxygen crosses the placenta through a process of facilitated diffusion. As the number of arterioles in the tertiary stem villi is decreased in gestational hypertension, the total surface area for diffusion is also decreased. As a result, there is reduced transfer of oxygen and nutrients to the fetus across the placenta. The first response of a fetus faced with a reduced supply of nutrients from the placenta is to reduce its metabolic needs by slowing growth velocity. Further deterioration of fetal oxygen supply leads to 'acidosis'. The gestational hypertension leading to hypoxemia fetal circulation undergoes a sequence of changes in response to hypoxemia. The initial response observed with Doppler ultrasound is cerebral vascular dilatation. This encourages an increased flow of blood with the highest oxygen concentration to the developing fetal brain. Venous Doppler studies become abnormal at a later stage. The increased after load, especially on the right side of the heart ultimately manifest in the changes seen in the inferior vena cava, ductus venosus and hepatic veins [1-25].
Materials and Methods
This is a prospective study conducted on hundred patients with clinically diagnosed pregnancy induced hypertension for the evaluation of the effectiveness of Doppler studies in hypertension complicating pregnancy with relevance to perinatal outcome undertaken at Sree Balaji Medical College and Hospital, Chromepet, Chennai, in the Department of Obstetrics and Gynaecology, during the period from August 2010 to September 2012.
Inclusion criteria
All antenatal cases more than 26 weeks of gestation clinically diagnosed as pregnancy induced hypertension.
Exclusion criteria
✓ All antenatal cases with chronic hypertension.
✓ All antenatal cases less than 26 weeks of gestation clinically diagnosed as pregnancy induced hypertension.
✓ All antenatal cases with abnormal Doppler findings without pregnancy induced hypertension.
✓ Intrauterine death at the time of first Doppler examination.
✓ Patients who cannot be followed up.
The first scan was performed in each case as soon as the patient was registered in order to avoid any influence of treatment on Doppler sonogram. The gestational age was confirmed by menstrual history and ultrasound examination and was followed by color Doppler examination. Consent was taken from the patient or the guardian.
Method of study
The Doppler Ultrasonogram is a new noninvasive technique that we have used in this study to determine the qualitative aspects of uteroplacental and fetal circulation. Fetus is relatively inaccessible to any form of antenatal wellbeing studies. It may be prudent to consider delivery of the fetus, once presumptive evidence of hypoxia is demonstrated. This is best accomplished with Doppler studies which can reliably predict adverse perinatal outcome in pregnancy induced Hypertension. The phenomenon of the Doppler effect is also observed when an ultrasound beam encounters blood flow. With blood circulation millions of red blood cells (RBC'S) act as moving scatterers of the incident ultrasound. In this circumstance the erythrocytes act first as moving receiver and then as moving sources. The Doppler frequency shift reflects but does not directly measure blood velocity. Doppler ultrasound can generate wide range of hemodynamic information from simple recognition of the presence of flow to the velocity profile of flow, quantification of flow, and assessment of downstream vascular impedance. Doppler ultrasound velocimetry is one of the non-invasive techniques for flow quantification in humans. (The other being recently introduced time domain processing approach). The maximum Doppler frequency shift waveform represents the temporal changes in the peak velocity of the red cell movement during the cardiac cycle. Techniques have been developed for analyzing this waveform in an angle independent manner. Most of these analytic techniques involve deriving Doppler indices or ratios from the various combination of the peak systolic, end diastolic, and temporal mean values of the maximum frequency shift envelope. Because these parameters are taken from the same cardiac cycle, these ratios are virtually independent of the angle of insonation. A unique characteristic of uteroplacental, fetoplacental and cerebral circulation in the fetus is the continuing forward flow during diastole. This feature develops progressively in fetoplacental circulation so that the perfusion of vital organs is uninterrupted throughout the cardiac cycle. The essential effect of this phenomenon includes not only the progressive increase in the end diastolic component of the flow velocity but also a concomitant decrease in the pulsatality, which is the difference between the maximum systole and the end diastolic components. The pulsatility of the flow velocity was originally investigated using Doppler ultrasound in the peripheral vascular system.
Indices of uterine artery waveform analysis
Uterine artery Doppler waveforms are most analyzed by simple semiquantitative techniques. They are based on maximum Doppler shift frequencies, which vary during the cardiac cycle. Evaluation of the change in maximal Doppler shift over time provides information on the impedance of the circulatory bed.
SID Ratio or A/B Ratio: Peak systole divided by end diastole. SID ratio showed a gradual decrease from a mean of 2.6 at 28 weeks to 1.6 at 40 weeks gestation.
Pulsatility Index (PI): which is the most complex of the three. It is calculated by peak systole minus end-diastole divided by mean value of the area under the curve over one cardiac cycle (S-D/ mean velocity). It requires a computer program that calculates the area under the curve.
Resistance index (RI) or Pourcelot ratio: Peak systole minus end diastole divided by peak systole (S-D/S).
The increase in flow resistance within the uterine arteries results in an abnormal waveform pattern which is represented by either an increase RI or PI or by the presence of unilateral or bilateral diastolic notch when the uterine artery systolic/ diastolic (SID) ratio was >2.6 during the third trimester, the birth weight at delivery was lower than normal and the incidence of fetal distress (low APGAR score and still birth) higher. Therefore, increased uterine resistance in hypertensive pregnant women should indicate that the fetus is significantly compromised.
Color flow mapping has allowed us to interrogate specific sites of the uterine circulation like arcuate, radial and the spiral arteries. Studies have shown that there is a drop in resistance from the proximal to the distal branches of the uterine circulation, the uterine artery having the highest impedance and the spiral arteries least.
Uterine artery waveform notch
The uterine artery Doppler waveform has an early diastolic notch in the non-pregnant state. It also persists in the pregnant state until 20-28 weeks of gestation40.Presence of a notch is a significantly better predictor of poor pregnancy outcome than the SID ratio or the resistance index (RI). It has been reported that an increased uterine artery RI without a uterine notch poorly correlates with adverse perinatal outcome50. The complexity of the uteroplacental circulation makes accurate identification of the vessel under study difficult with either continuous wave or duplex Doppler ultrasound. Flow velocity waveforms are obtained from the lateral lower quadrants of the uterus, angling the transducer on either side of the uterus towards the cervix. Signals achieved in this way are assumed to be originating from the uterine arteries. The uterine arteries are more accurately identified using color Doppler: the region lateral to the lower uterus is examined and the external iliac artery and the adjacent vein are identified. The uterine artery crosses the external iliac artery on its course from the internal iliac artery to the body of the uterus. It is important to angle the transducer to improve the angle of insonation while maintaining vessel identification on the color Doppler. Spectral waveforms are obtained by placing the pulse Doppler range gate within the vessel at this point. In the non-pregnant state, the uterine artery is a high resistance vessel. It shows a high resistance waveform. Low diastolic flow and early diastolic notching is a normal fetus of the non-pregnant uterine circulation.
With pregnancy, trophoblastic invasion of the spiral arteries takes place converting the high resistance flow pattern into that of a low resistance pattern characterized by increase in diastolic flow and disappearance of the notch. It is essential to study both the uterine arteries because of variations in placentation. In cases of a laterally located placenta, the placental side uterine artery is the main supplier, that it has a lower resistance as compared to the opposite uterine artery. Examination of both the uterine arteries is an indispensable element of Doppler examination to assess placental performance and risk to the fetus51.When the placenta is centrally located, there is equal contribution by both the uterine arteries. In case of a unilateral placenta, if the degree of contribution by the opposite uterine artery is deficient, it can facilitate the development of preeclampsia, IUGR or both. Therefore, before studying the uterine artery, it is imperative to know the side of the placenta and determine the "placental side uterine artery".
Color Doppler ultrasound examination for hemodynamical changes of uterine arteries, umbilical vessels and middle cerebral artery revealed utero-placental-fetal circulation function directly. It is one of the best methods for monitoring IUGR and used for early diagnosis of IUGR. The main pathophysiological changes of IUGR are uteroplacental- fetal circulation obstruction and placental dysfunction.In abnormal pregnancies due to lack of trophoblastic invasion, there is increased resistance in the p1acental bed. This increased resistance is reflected back in the uterine arteries. These uterine arteries are characterized by
✓ Low diastolic flow.
✓ An early diastolic notch.
✓ Biphasic deceleration slope.
✓ High indices.
During the course of pregnancy, the uterine artery changes from a high resistance pattern with no notches. Disappearance of notch will happen first in the uterine artery which is directly under the placenta. Normally the notch is seen until 28 weeks of gestation. Persistence of notch after 28 weeks is an indicator of hypertensive complications/ IUGR or both. Persistence of notch indicates unaltered vasospasm. After delivery, the uterine artery does not return to its pre pregnant level for 4-6 weeks.
Various indices have been used to describe the uterine artery waveform eg: systolic/ diastolic ratio, RI and PI. These indices in due course of pregnancy should show a fall in their values. Failure of trophoblastic invasion results in increased resistance to flow, a low diastolic velocity and consequent increase in indices causing uteroplacental insufficiency. Abnormal Doppler values indicative of a failure to modify the uterine circulation in early pregnancy are associated with preterm delivery, development of proteinuric PIH and SGA fetus. The upper limit of systolic/ diastolic ratio is approximately 2.6. The systolic/ diastolic ratio more than 2.6 after 26 weeks of gestation suggests that full trophoblastic invasion "' s not occurred and mother and fetus are at risk for adverse outcome.The upper limit of RI value is about 0.58. Increased values of RI indicate that there is increased risk of IUGR. The RI value will be lower from placental side and from distal accurate than proximal uterine arteries52. The difference between the systolic/ diastolic ratio of both uterine arteries should not exceed 1 normally. A difference of more than 1 indicates preeclampsia and IUGR53. Pathological Doppler velocimetry of the uterine and uteroplacental circulation is a powerful predictor of proteinuric PIH and /or IUGR in high-risk pregnancies. Doppler examination of uterine and umbilical arteries can detect at mid pregnancy, the severe forms of PIH and SGA fetuses.
Uterine arteries
Uterine artery blood reflects hemodynamic changes that occur on the maternal side of the placenta43.Pregnancy results in marked changes in the uterine artery waveform. The resistance to blood flow in both uterine arteries decreases gradually from early pregnancy until the end of the second trimester. Hence, the systolic-diastolic values do not change from 28th week.
Umbilical artery
Umbilical artery flow velocity waveform correlates the hemodynamic changes in the fefoplacental circulation or in other words reflect downstream (placental) vascular resistance. With the aid of color flow, the umbilical arteries can be detected as early as 8-10 weeks. A characteristic umbilical artery FVW has a rapid upstroke during systole and a gradual decline during diastole, while maintaining a continuous forward flow. A decrease in peripheral resistance results in an increased end diastolic velocity. Conversely, increased peripheral resistance.
Site of doppler interrogation
Several studies have shown that the location of Doppler sampling site in the umbilical cord affects the Doppler waveform and is reflected in the Doppler indices. Abnormal umbilical artery FVWs represents a failure of development of adequate placental vasculature, with normal umbilical artery FVWs (seven to eight arterioles per high power field). About 40% of hypertensive pregnancies have increased resistance in the umbilical artery (>2 SD of normal values). An extreme situation of impaired umbilical blood flow is an absence of end-diastolic flow velocity. There is an ominous association between the absent end-diastolic velocity and adverse perintal outcome. Perinatal morbidity includes preterm birth and low birth weight infants, which are mostly attributable to fetal or maternal complications mandating early intervention. In these conditions, fetal heart rate monitoring and Doppler studies of the middle cerebral arteries may provide more information regarding the fetal state. It is noted that the evidence of developing AEDV/REDV was lesser in pregnancies complicated by hypertension alone, than if pregnancies were complicated by fetal growth retardation and hypertension together.
The insonation angle should be: ss than 60°. Approximately twelve waveforms should be averaged, the indices should be ideally taken at the mid cord or at placental insertion. The indices are highest at the fetal abdomen and lowest at the cord insertion into the placenta. The wall filter should be set at 100 MHz. If there is absent end diastolic velocity, it may lower to 50 MHz. The umbilical artery waveform is a simple waveform with no systolic or diastolic notching and with a large amount of diastolic flow velocity. During the normal course of pregnancy there is an overall increase in placental size with resulting increase in number of tertiary stem villi. The number of small aterial channels in these tertiary villi keeps on increasing causing a decrease in resistance to diastolic flow. This decrease in resistance is reflected as an increase in diastolic velocity. Before 16-18 weeks of gestation, the placental circulation is a high resistance bed, and the indices are on the higher side. During the latter half of gestation, there should be a normal fall in the indices. In abnormal pregnancies, because of high resistance in the placental bed there will be reduced, absent or reversed end diastolic flow velocity. Absent end diastolic velocity is clearly abnormal. Most abnormal umbilical flow velocity wave forms represent a failure of development of an adequate placental vasculature. Fetuses that are growth retarded with abnormal flow velocity have half as many tertiary arterioles. The most used indices for the umbilical artery are systolic/ diastolic, RI and PI. SID ratio decreases from a mean of 3.08 at 28 weeks to 2.1 at 40 weeks. The mean value of RI decreases from 0.67 at 28 weeks to 0.52 at 40 weeks. PI also fall from 1.02 at 28 weeks to 0.69 at 40 weeks gestation55. An abnormal Doppler wave form analysis of umbilical artery (systolic/ diastolic ratio more than 3) is the more accurate predictor of poor out come in SGA fetuses56. Abnormal umbilical artery Doppler waveforms were found m higher number of hypertensives as compared to normotensives. Hypoplastic umbilical vessels are associated with an increase in placental vascular resistance that may be the consequence of under development in response to a chronic reduction in placental blood flow.With increase in SID umbilical artery ratio, birth weight percentile decreased59. In patients with IUGR fetuses, those with normal umbilical artery findings does not require any intervention.The absence of end diastolic velocity in the umbilical artery is a distinctly abnormal finding that identifies a high resistance feto placental circulation rather than the normally low resistance system and adverse fetal outcome.
Absent end diastolic flow uniformly heralded adverse perinatal outcome and in severity it is next to reverse flow, which is rare. Reverse flow is a morbid event and is the most severe velocity flow abnormality seen. Fetuses with absent end diastolic flow have low birth weight, will be born earlier and have a high incidence of IUGR, PIH and a low APGAR score. Absent end diastolic velocity may precede clinical signs of stress by long periods of time. Absent end diastolic velocities are also seen in SGA fetus, fetal trisomies and fetal distress etc.In patients with AEDV and REDV, erinatal mortality was 50% and the rest 50% are IUGR babies.
Middle cerebral artery
The fetal cerebral blood flow is a high impedance low flow circulation. It is a more sensitive parameter of fetal oxygenation status than umbilical blood flow. With color Doppler technology it is now possible to investigate the main cerebral arteries and to evaluate vascular resistance of the same46. In response to prolonged fetal hypoxic stress, circulatory adaptation occurs, resulting in redistribution of the cardiac output to provide constant oxygen supply to brain and other essential organs like heart and adrenal glands.
Cerebral doppler indices
To quantify the vascular resistance, the indices used are the same as that of uterine and umbilical arteries.
✓ Pulsatility index (Pl).
✓ Systolic/ Diastolic (SID) ratio.
✓ Resistance index (RI).
Results and Discussion
In the present study, out of 100 cases of Hypertension Complicating Pregnancy, 58 cases showed positive Doppler indices in any of the three vessels studied. The remaining 42 cases showed normal Doppler indices in all the three vessels studied. The following were the results of the study (Tables 1 and 2). 36 % cases show abnormal MCA Doppler findings in the present study (Figure 1).
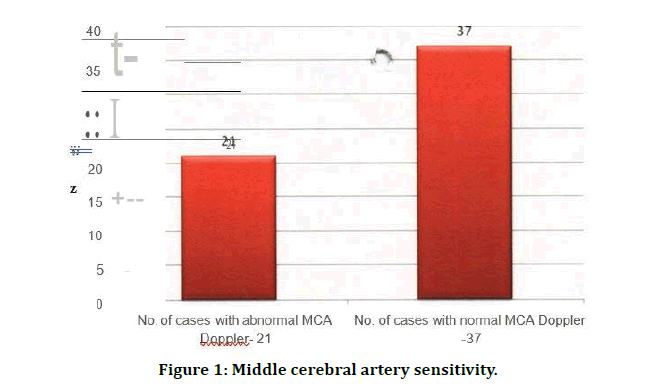
Figure 1: Middle cerebral artery sensitivity.
Table 1: Middle cerebral artery sensitivity.
| Parameters | No. of cases | Percentage |
|---|---|---|
| No. of cases with abnormal MCA Doppler | 21 | 36.21 |
| No. of cases with normal MCA Doppler | 37 | 63.79 |
| Total | 58 | 100 |
Table 2: Sensitivity of various vessels studied.
| Parameters | No. of cases | Percentage |
|---|---|---|
| Uterine artery | 43/58 | 72.41 |
| Umbilical artery | 42/58 | 74.13 |
| Fetal MCA | 21/58 | 36.21 |
The Doppler study of umbilical artery is most sensitive of all the vessels under the study. Umbilical artery flow velocity waveforms correlate with hemodynamic changes in the fetoplacental circulations. Increased impedance to the blood flow in the umbilical artery is significantly associated with IUGR and perinatal n=rbidity and mortality. The present study shows that the umbilical artery flow velocity study to be significant in detecting abnormal perinatal outcome. 28% of the cases showed decreased liquor on ultrasonography, while about 70% showed normal amount of liquor (Table 3 and Figure 2).
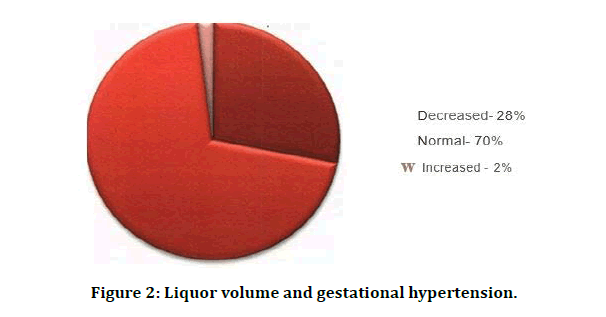
Figure 2: Liquor volume and gestational hypertension.
Table 3: Liquor volume and gestational hypertension.
| Liquor | No. of cases | Percentage |
|---|---|---|
| Decreased | 28 | 28 |
| Normal | 70 | 70 |
| Increased | 2 | 2 |
| Total | 100 | 100 |
Pritchard and colleagues in 1984 Reported that in severe preeclampsia, plasma creatinine may be elevated up to several times the non-pregnant value (Figure 3). Uric acid is the product of purine metabolism. Elevated Serum urine acid levels are due to decreased renal rate excretion. In the present study increased serum uric acid levels were found more in mild and severe preeclampsia cases.
Figure 3: Sr. Creatinine in gestational hypertension.
In 1990 researchers have found that plasma uric acid values exceeding 5-9 mg/dl at 24weeks had a positive predictive value for preeclampsia of 33%. In 1976 researchers suggested that serum uric acid is a useful indicator of the risk (Table 4).
Table 4: Sr. Uric acid (mg/di).
| Sr. Uric acid (mg/di) | No. of Cases | Percentage |
|---|---|---|
| < 3.5 | 49 | 49 |
| 3.6 -4.5 | 25 | 25 |
| 4.6- 6.0 | 17 | 17 |
| > 6.0 | 9 | 9 |
| Total | 100 | 100 |
Of the 30 vaginal deliveries, 6 were spontaneous, one case was induced with misoprostol and 12 cases with Prostaglandin E2 gel. All the cases were monitored antenatally by ante partum surveillance and CTG. ARM and Oxytocin acceleration was done in as per necessary with close monitoring of fetal heart rate. 3 cases required forceps extraction and 2 in cases vacuum application.
Of the total cases, 16 women had previous LSCS, had repeat LSCS. in cases with abnormal CTG pattern and fetal distress, 14 cases of failed induction, Emergency LSCS was done (Table 5 and Figure 4).
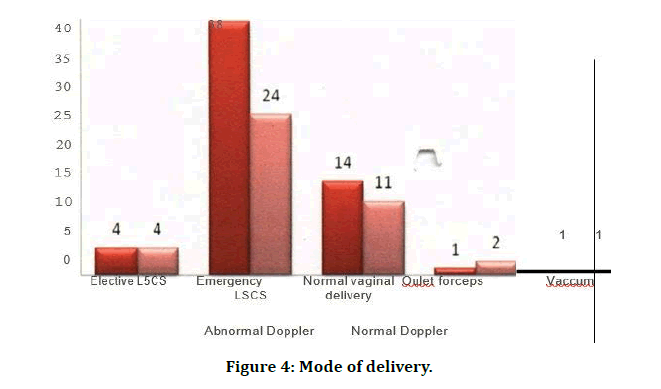
Figure 4: Mode of delivery.
Table 5: Mode of delivery.
| Mode of delivery | No. of cases (Abnormal doppler) | No. of cases (Normal doppler) | Total |
|---|---|---|---|
| Elective LSCS | 4 | 4 | 8 |
| Emergency LSCS | 38 | 24 | 62 |
| Normal vaginal delivery | 14 | 11 | 25 |
| Oulet forceps appilication | 1 | 2 | 3 |
| Vaccum assisted | 1 | 1 | 2 |
| Total | 58 | 42 | 100 |
Healthy baby X2 - 3.08 and NICU X2 - 20.46 (p<0.01) , highly significant. In the present study, babies of 63.79% (37/58) with abnormal Doppler indices had NICU stay which indicates adverse perinatal outcome with abnormal Doppler compared to normal Doppler. In the present study, 16.67% (7/42) of the babies born to cases with normal Doppler indices had NICU stay (Table 6 and Figure 5).
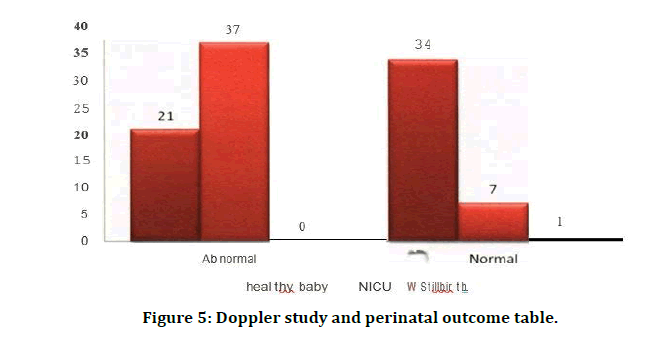
Figure 5: Doppler study and perinatal outcome table.
Table 6: Doppler study and perinatal outcome.
| Healthy baby | NICU | Stillbirth | Total | |||||
|---|---|---|---|---|---|---|---|---|
| Doppler | No. | % | No. | % | No. | % | No. | % |
| Abnormal | 21 | 36.21 | 37 | 63.79 | 0 | 0 | 58 | 58 |
| Normal | 34 | 80.95 | 7 | 16.67 | 1 | 2.38 | 42 | 42 |
| Total | 55 | 55 | 44 | 44 | 1 | 1 | 100 | 100 |
In the present study, 12 of cases (74.3%) with abnormal Doppler indices had APGAR score <7 when compared to 3 babies (7.14%) in normal cases (Table 7 and Figure 6). Comparison of birth weight percentage distribution is shown in Table 8 and Figure 7. In the present study, number of babies with SGA in abnormal Doppler indices group were 20 when compared to 8 in normal Doppler indices group (Table 9). Neonatal complications are mentioned in Table 10.
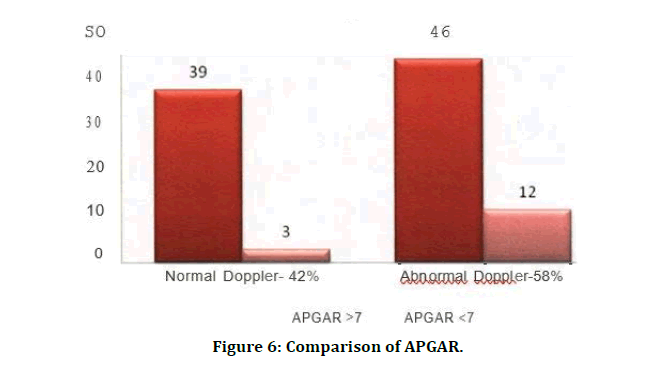
Figure 6: Comparison of APGAR.
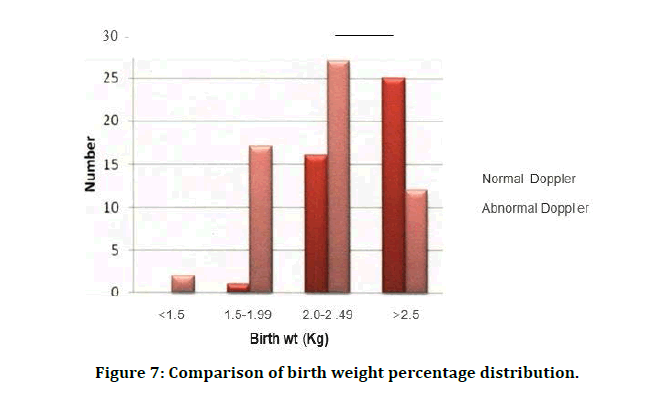
Figure 7: Comparison of birth weight percentage distribution.
Table 7: Comparison of APGAR.
| APGAR Score | Total | ||||
|---|---|---|---|---|---|
| 7 | <7 | ||||
| No. | Percent | No. | Percent | ||
| Normal | 39 | 92.86 | 3 | 7.14 | 42 |
| Abnormal | 46 | 79.31 | 12 | 74.3 | 58 |
| Total | 85 | 85 | 15 | 15 | 100 |
APGAR X2 - 3.51(p<0.01)
Table 8: Comparison of birth weight percentage distribution.
| Birth weight (Kg) | Normal | Abnormal | Total | |||
|---|---|---|---|---|---|---|
| No. | Percent | No. | Percent | No. | Percent | |
| < 1.5 | 0 | 0 | 2 | 3.45 | 2 | 2 |
| 1.5-1.✓ | 1 | 2.38 | 17 | 29.31 | 18 | 18 |
| 2.0-2.49 | 16 | 38.1 | 27 | 46.55 | 43 | 43 |
| 2.5 | 25 | 59.52 | 12 | 20.69 | 37 | 37 |
| Total | 42 | 100 | 58 | 100 | 100 | 100 |
Table 9: Distribution of cases among AGA/SGA.
| Abnormal | Normal | Total | ||||
|---|---|---|---|---|---|---|
| No. | Percent | No. | Percent | No. | Percent | |
| AGA | 38 | 65.52 | 34 | 80.95 | 72 | 72 |
| SGA | 20 | 34.48 | 8 | 19.05 | 28 | 28 |
| Total | 58 | 100 | 42 | 100 | 100 | 100 |
Table 10: Neonatal complications.
| Abnormal | Normal | |||
|---|---|---|---|---|
| Types | No. | Percent | No. | Percent |
| Birth asphyxia | 6 | 10.91 | 1 | 5.56 |
| Meconium aspiration syndrome | 9 | 16.36 | 2 | 11.11 |
| Hyperbilirubinemia | 18 | 32.73 | 8 | 44.44 |
| Respiratory distress syndrome | 9 | 16.36 | 7 | 38.89 |
| Hypoxic ischemic encephalopathy | 6 | 10.91 | 0 | 0 |
| Hypoglycemia | 6 | 10.91 | 0 | 0 |
| Sepsis | 1 | 1.82 | 0 | 0 |
| Total | 55 | 100 | 18 | 100 |
This is a prospective study done in the department of Obstetrics and Gynaecology, Sree Balaji Medical College and Hospital, Chromepet, Chennai. Study duration is for two years, from August 2010 to September 2012. This study is done in a population of 100 pregnant women with gestational hypertension. The percentage of normal and abnormal dopplers of present study correlated well with the other studies. Present study has shown majority of cases (72.41%) with abnormal umbilical artery SID ratio, w is comparable to the study conducted, while 56.9% cases had abnormal uterine artery SID ratio, corresponding with the results ofU. Umbilical artery flow velocity waveforms correlate with hemodynamic changes in the fetoplacental circulations. Increased impedence to the blood flow in the umbilical artery is significantly associated with IUGR and perinatal morbidity and mortality. The present study shows that the study of umbilical artery flow velocity is significant in detecting abnormal perinatal outcome.
In the present study, 24 out of 100 cases (24%) had persistent diastolic notch (Table 11). According to Thaler et al an early diastolic notch persists after 26 weeks of gestation in 25-40% of hypertensive pregnant women. Presence of the notch is a significantly better predicator of poor pregnancy outcome than the SID Ratio (or) the RI. Others noted that the Ute: artery notch was a good predictor of poor perinatal outcome - increased rate of IUGR, Caesarean delivery for fetal distress and preterm delivery.
Table 11: Uterine artery persistent diastolic notch.
| Studies | Persistence of diastolic notch |
|---|---|
| Previous study | 25-40% |
| Present study | 24% |
Uric acid is the product of purine metabolism. Elevated Serum urine acid levels are due to decreased renal rate excretion. In the present study increased serum uric acid levels were found more in pre-eclampsia cases than in cases with gestational hypertension. It was found that estimating plasma uric acid levels at 24weeks was not a good predictor of pre-eclampsia. All the cases were monitored by ante partum surveillance. In the present study, 30 women had vaginal deliveries. Of these, 6 had spontaneous onset of labor while others were induced. One case was induced with misoprostol and 12 cases with Prostaglandin E2 gel, after assessing their Bishop's score. Indication for induction, was severe preeclampsia. During labor, ARM and Oxytocin acceleration was done when required with close monitoring of fetal heart rate. Three cases required forceps and in 2 cases vacuum was applied. Of the total 100. cases, 16 women had previous LSCS, so repeat LSCS was done for them. In rest of 64 cases emergency LSCS was done in view of either abnormal CTG pattern, fetal distress or failed induction.
In the present study, babies of 63.79% (37/58) with abnormal Doppler indices had NICU admission which indicates adverse perinatal outcome with abnormal Doppler compared to normal Doppler group, in which 16.67% (7/42) of the babies had NICU admission. These studies, 55.1% of cases with abnormal Doppler indices had NICU admission (Table 13).
Table 12: Percentage of women with oligohydramnios.
| Percentage of cases with oligohydramnios | ||
|---|---|---|
| Studies | Normal dopplers | Abnormal dopplers |
| Previous study | 4.47 | 12.40% |
| Present study | 10% | 18% |
Table 13: Abnormal doppler indices and NICU stay.
| Studies | Abnormal Doppler | NICU admission |
|---|---|---|
| Previous study | 55% | 55.10% |
| Present study | 58% | 63.79% |
In study, in correlation of perinatal outcome, birth weight and Doppler findings in 100 hypertensive women, 92.10% of SGA babies and 32.25% of cases with AGA babies had abnormal uterine artery Doppler. In present study, 38 out of 72 (52.78%) AGA babies had abnormal Doppler study and 20 out of 28 (71.43%) SGA babies had Doppler abnormality (Table 14).
Table 14: Abnormal doppler indices and birth weight.
| Studies | Abnormal doppler | AGA | SGA |
|---|---|---|---|
| Previous study | 55% | 32.25% | 92.10% |
| Present study | 58% | 52.78% | 71.43% |
In the present study, maternal complications encountered were 6%- abruption placentae, 3% eclampsia and most of the cases needed induction of labour and majority of cases went in for operative delivery. In the present study, of the 58 women with abnormal Doppler indices, 55 babies born to them had adverse perinatal outcome in terms of neonatal complications which included birth asphyxia, Meconium aspiration syndrome, hyperbilirubinemia, Respiratory distress syndrome, etc. of the mentioned neonatal complications, majority of them had hyperbilirubinemia-18/55, while it was only 8 babies abnormal Doppler indices had hyperbilirubinemia.
In normal fetuses, there is little diastolic flow in middle cerebral artery and the systolic/ diastolic ratio is normally more than 4 throughout the pregnancy. The diastolic flow velocity increases slightly during gestation, resulting in some diminution of systolic/ diastolic ratio as a function of gestational age. The mean PI in middle cerebral artery at 28 weeks of gestation is 1.6±0.4 and at 40 weeks it is 1.2±0.4 with a significant reduction after 32 weeks of gestation. There is redistribution of fetal blood flow in response to hypoxia with a selective increase in the blood flow to the brain, heart, adrenal glands at the expense of viscera. This reduction reflects the morphological findings in IUGR, with the head continuing to grow at the expense of a relatively smaller abdomen. Fetal outcome is thought to be related both to the severity and duration of hypoxia, as well as the gestation age at delivery. It is assumed that hypoxia will tend to increase with increasing gestation age in fetuses with growth retardation and that this will lead to a greater redistribution of blood flow.
The fetus with significant reduction of umbilical flow should have dilated cerebral flow. If it does not, it is critically ill or not hypoxic. If it is not hypoxic, it may have congenital heart disease, and the reduced peripheral flow is caused by reduced forward flow, not increased resistance. Abnormal cerebral (MCA)/ umbilic l artery pulsatility ratio help m distinguishing small distressed fetuses from the small relatively healthy ones. Normally the ratio of PI of MCA/ umbilical artery is 2:1. If it is one it indicates IUGR. SGA fetuses with an abnormal umbilical artery PI have cerebral sparing effect as their PI was less than normal.
Doppler flow measurement of MCA provides useful information about perinatal outcome, especially in the high risk pregnancies. In suspected IUGR, while an abnormal umbilical artery PI is a better predictor of adverse perinatal outcome, than an abnormal MCA or renal artery Pl. A normal PI of MCA may help to identify fetuses without major adverse perinatal outcome, especially before 32 weeks of gestation. The blood flow characteristic can be quantified by various Doppler indices like the systolic/ diastolic ratio (S/D), resistance index (RI) and the pulsatility index (Pl), which can be taken on any vessels.
Most of the cases were followed up postnatal, 11 cases, all of them had severe preeclampsia, needed post-natal antihypertensives for a period of one to two weeks. In the present study, maternal complications encountered were 6%- abruption placentae, 3% eclampsia and most of the cases needed induction of labour and majority of cases went in for operative delivery. In the present study, of the 58 women with abnormal Doppler indices, 55 babies born to them had adverse perinatal outcome in terms of neonatal complications which included birth asphyxia, Meconium aspiration syndrome, hyperbilirubinemia, Respiratory distress syndrome, etc. of the mentioned neonatal complications, majority of them had hyperbilirubinemia-18/55, while it was only 8 babies abnormal Doppler indices had hyperbilirubinemia (Figure 8 and Figure 9).
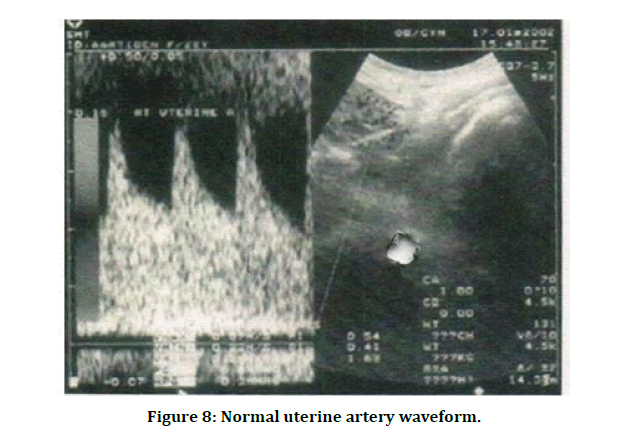
Figure 8: Normal uterine artery waveform.
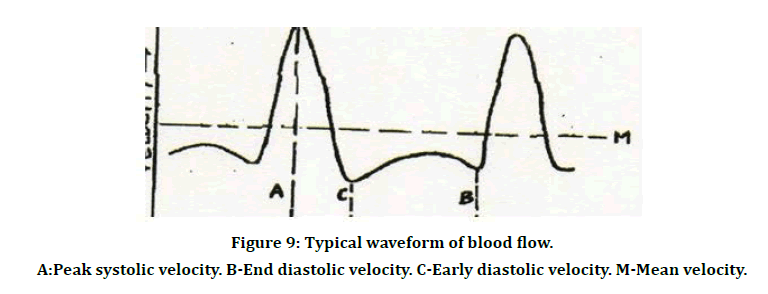
Figure 9: Typical waveform of blood flow.
A:Peak systolic velocity. B-End diastolic velocity. C-Early diastolic velocity. M-Mean velocity.
A:Peak systolic velocity. B-End diastolic velocity. C-Early diastolic velocity. M-Mean velocity.
Most of the cases were followed up postnatal, 11 cases, all of them had severe preeclampsia, needed post-natal antihypertensives for a period of one to two weeks. While on 13 women with gestational hypertension required postnatal antihypertensives for a period of one week [26-54].
Conclusion
Uterine, umbilical, and fetal middle cerebral arteries were studied AEDV and REDV in umbilical artery; in middle cerebral artery were considered abnormal. The results were correlated with parameters of perinatal outcome. In the present study increased serum uric acid levels were found more in mild and severe pre-eclampsia cases. Some of the cases showed decreased liquor on ultrasonography, while about little shows normal amount of liquor. There is no strong correlation between oligohydramnios and perinatal outcome. The results show abnormal doppler indices in one of the three vessels studied. The remaining cases showed normal Doppler indices in all the three vessels studied. All the cases were monitored by ante partum surveillance. In the present study, some women had vaginal deliveries. Of these, some had spontaneous onset of labor while others were induced. Indication for induction, was severe pre-eclampsia. During labor, ARM and Oxytocin acceleration was done when required with close monitoring of fetal heart rate. Three cases required forceps and in 2 cases vacuum was applied. There was 1 still birth in a woman normal Doppler index, m which fetal heart sound was absent at the time of admission itself. Most of the cases were followed up postnatal, all of them had severe preeclampsia, needed postnatal antihypertensives for a period of one to two weeks.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Chesley LC. A short history of eclampsia. Obstet Gynecol 1974; 43:500-602.
- Hypertension in pregnancy. ACOG Technical Bulletin. 1996; 219:1-8.
- Myers JE, Baker PN. Hypertensive diseases and eclampsia. Current Opinion Obstetr Gynecol 2002; 14:119-125.
- Walsh SW. Pre-eclampsia: An imbalance m placental prostacycline and thromboxane production. Am J Obstet Gynecol 1985; 152:335-340.
- Newnham JP, O'Dea MRA, Reid KP, et al. Doppler flow velocity waveforms analysis in high risk pregnancies: A randomized controlled trial. Br J Obstet Gynaecol 1991; 98:956-963.
- Baker DW. Pulsed ultrasonic doppler blood flow sensing IEEE trans sonic ultrasonics. IEEE SU 1970; 170-185.
- Angelsen BAJ, Kristofferson K. On ultrasonic MTI measurement of velocity profiled in blood flow. Trans Biomed Eng 1979; 26:665 -771.
- Namekawa K, Kasai C, Tsukamoto M, et al. Imaging of blood flow using auto correlation. Ultrasound Med Biol 1982; 8:138.
- Callaghan DA, Rowland TC, Goldman DE. Ultrasonic doppler observation of the fetal heart. Obstet Gynecol 1964; 23:637.
- FitzGerald DE, Drumm JE. Noninvasive measurement of the fetal circulation using ultrasound : A new method. Br Med J 1977; 2:1450-1451.
- MaCallum WD, Olson RF, Daigle RE, et al. Real time analysis of doppler signals obtained from the fetoplacental circulation. Ultrasound Med 1977; 3:1361-1364.
- Gill RW. Pulsed Doppler with B-mode 1magmg for quantitative blood flow measurements. Ultrasound Med Biol 1979; 5;223-227.
- Eik-Nes SH, Brubakk AO, Ulstein. Measurement of human fetal blood flow. Br Med J 1980; 28:283.
- Campbell S, Diaz Recasens J, Griffin DR, et al. New doppler technique for assessing uteroplacental blood flow. Lancet 1983; 1:675.
- Chiba Y, Utsu M, Kanzaki T, et al. Changes in venous flow and intra-tracheal flow in fetal breathing movements. Ultrasound Med Biol 1983; 11:43
- Maulik D, Nanda NC, Saini VD. Fetal Doppler echocardiography: methods and characterization of normal and abnormal hemodynamics. Am J Cardiol 1984; 53: 572.
- Arbeille P, Tranquart F, Body G, et al. Evolution de la circulation arterielle ombilicale et cerebrale du la foetus au cours de la grossesse. Prog Neonatol 1986; 6:30.
- Wladimiroff JW, Tonge HN, Stewart PA. Doppler ultrasound assessment of cerebral blood flow in the human fetus Br J Obstet Gynaecol 1986; 93:471.
- Vyas S, Nicolaides KH, Campbell S. Renal artery flow¬ velocity waveforms in normal and hypoxemic fetuses. Am J Obstet Gynecol 1989; 1989; 161:168-172.
- Veille JC, Kanaan C. Duplex Doppler ultrasonographic evaluation of the fetal renal artery in normal and abnormal fetuses. Am J Obstet Gynecol 1989; 161:1 02-1507.
- Devore GR, Hornstein J, Siassi B, et al. Doppler color flow mapping in use the prenatal diagnosis in the human fetus Echocardiography 1985; 2:551-557.
- Maulik D, Nanda NC, Hsiung MC, et al. Doppler color flow mapping of the fetal heart. Angiology 1986; 37:628-632.
- Taylor KJW, Bums PN, Wells PNT, et al. Ultrasound Doppler flow studies of the ovarian and uterine arteries. Br J Obstet Gynaecol 1985; 92:240-246.
- Atkinson P, Woodcock JP. Doppler ultrasound. Academic Press, London. Gill RW ; Doppler ultrasound: Physical aspects. Semin Perinatol 1982; 11:292.
- Reid JM, Spencer I. Ultrasonic doppler technique for imaging blood vessels. Science 1972; 176:1235.
- Carroll BA, von Ramm OT. Fundamentals of current doppler technology. Ultrasound 1988; 275.
- Maulik D, Yarlagadda P. In vitro validation of doppler waveform indices. Maulik D, McNellis D (Eds). Perinatology Press, Ithaca, Ny, P 1987; 257.
- North RA, Ferrier CL long D, et al. Utreine artery doppler flow velocity waveforms in the second trimester for the prediction of pre-eclampsia and fetal growth retardation. Obstet Gynecol 1994; 83;378-86.
- Low JA. The current status of maternal and fetal blood flow velocimetry. Am J Obstet Gynecol 1991; 164:1049.
- Gary Cunningham F, Gnat NF, et al. Wenstrom williams obstetrics. 21st Edn 567:1136.
- Porcelot L. Applications cliniques de I examen Doppler transcutane In: Perommeau P, ed. Velocimetric ultrasonoic Doppler. Paris INSERM 1974; 213.
- Maulik D, Yarlagadda P. Components of variability of umbilical artetrial doppler velocimetry: A prospective analysis. Am J Obstet Gynecol 1989; 160:1406.
- Merritt CRB, Kremakau FW, Hobbins JC: Diagnostic ultrasound: Bioeffects and safety. Ultrasound Obstet Gynecol 1992; 2:366.
- Miller MW, Ziskin MC. Biological consequences of hyperthermia. Ultrasound Med Biol 1990; 15:707.
- Jauniaux E, Jurkovic D, Campbell S, et al. Investigation of placental circulations by color doppler ultrasonography. Am J Obstetr Gynecol 1991; 164:486-488.
- Thaler I, Manor D, Itskovitz J. C.aanges in uterine blood flow during human pregnancy. Am J Obstet Gynecol 1990; 162:121-125.
- Brosens I, Pijnenborg R, Bland JM, et al. Uteroplacental arterial changes related to interstitial trophoblastic migration in early pregnancy. Placenta 1983; 4:397-414.
- Campbell S, Kevin H, Kurt H. A color atlas of doppler ultrasonography in obstetrics-An induction to its use in maternal fetal medicine. Edited by Kevin H, Campbell S, London, 1995; 60.
- Schulman H, Fleischer A, Stem W. Umbilical velocity wave ratios in human pregnancy. Am J Obstet Gynecol 1984; 148:985-990.
- Rubin PC, Bronghton, Pipkin F. Pre-eclampsia the disease of theories. Br Med Bull 1994; 50:381-96.
- Redman CWG. Current topic: Pre-eclampsia and the placenta. Placenta 1991; 12:310-318.
- Trudinger BJ, Warwich B, Giles MB, et al. Flow velocity waveforms in the maternal uteroplacental and fetal umbilical placental circulation. Am J Obstet Gynecol 1985; 152:155-163.
- Zeeh PM, Arsali NS. Vascular changes in the decidua associated with eclamptogenic toxemia of pregnancy. Am J Clin Patho 1950; 20:1099-1109.
- Peeters LL, Sheldon RE, Jone MK, et al. Blood flow to fetal organs as a function of arterial ox en content. Am J of Obstet Gynecol 1979; 135:637-646.
- Arbeille P, Montenegro N, Tranquart F, et al. Assessment of the fetal cerebrovascular areas by color coded Doppler. Enchocardiography J 1990; 7:629-634.
- Fleischer A, Schulman H, Formahides G, et al. Uterine artery doppler primary in pregnant women with hypertension. Am J Obstet Gynecol 1986; 154:806-813.
- Trudinger BJ, Cook CM. Doppler umbilical and uterine flow waveforms in severe pregnancy hypertension. Br. J Obstet Gynecol 1990; 97:142-148.
- Chesley's hypertensive disorders m pregnancy. By Lindheimer MD, Roberts JM, Cunningham FG, et al. 3rd Edn 2009; 192.
- Thaler I, Weiner Z, Itskovitz J. Systolic or diastolic notch in the uterine artery blood flow velocity waveforms in hypertensive pregnant patients: Relationship to outcome. Obstet Gynecol 1992; 80:277-282.
- Joern H & Rath W. Comparison of doppler sonographic examination of the umbilical and uterine arteries in high risk pregnancies. Fetal Diagn Ther 1998; 13:150-153.
- Campbell S, Cooper D, Bewley S. Uteroplacental Doppler flow velocity waveforms. Br. J Obstet Gynecol 1989; 96:1040-1046.
- Farmakides, Schulman. Surveillance of the pregnant hypertensive patient with doppler flow velocimetry. Clin Obstetr Gynaecol 1992; 35:387-394.
- Karsdrop VH, Van Vingt JM. Clinical significance of absent or reversed end diastolic velocity waveforms in umbilical artery. Lancet 1994; 344:1664-1668.
- Khalid M, Wahab S, Kumar V, et al. Doppler indices in prediction of fetal outcome in hypertensive pregnant women. Nepal J Obstet Gynaecol 2011; 6:28-34.
Author Info
A Padmaja Rani, K Saraswathi and K Vani*
Department of Obstetrics & Gynecology, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: A Padmaja Rani, K Saraswathi, K Vani, Correlation Between the Doppler Study with Fetal Outcome and Analysis of the Association of Abnormal Doppler Velocimetry in Perinatal Outcome, J Res Med Dent Sci, 2021, 9 (5):156-169.
Received: 22-Apr-2021 Accepted: 18-May-2021 Published: 25-May-2021
