Research - (2019) Volume 7, Issue 2
Correction of Severe Spinal Deformities Using Posterior Osteotomy in Young Patients: What are the Outcomes?
Mohammad Reza Etemadifar1, Mehdi Koushkzari1*, Ali Andalib1 and Mahsa Behnemoon2
*Correspondence: Mehdi Koushkzari, Department of Orthopedic Spine Surgery, Isfahan University of Medical Sciences, Iran, Email:
Abstract
Background: Surgical treatment of severe spinal deformities is a big challenge for most spine surgeons. From both patient and surgeon's perspectives, balanced correction without major complications is the goal. Several strategies have been used to reach this aim. Posterior spine osteotomies (POs) eliminate longer hospital stays for traction and obviate the need for combined anterior and posterior approaches thus minimizing complications. There are potential complications associated with POs especially three column osteotomies.
Methods: This is a retrospective-cohort-study conducted on 57 patients with severe rigid spinal deformity who underwent POs from 2013-2017. Patients' demographics (e.g. age, sex), type and severity of spinal deformity, type of osteotomy including smith Peterson osteotomy (SPO), pedicle subtraction osteotomy (PSO) and vertebral column resection (VCR), duration of surgery, bleeding in perioperative period and neurological deficit were evaluated. Patients have been followed for at least two years for Cobb angles and complications such as infection and device failure.
Results: In this study, 57 patients with mean age of 21.80 ± 7.50 years were included. Etiologies were idiopathic, congenital or syndromic. For scoliotic patients, coronal Cobb angle changed from 73.21 ± 10.09 pre-operatively to 16.40 ± 6.25 after two years (p-value<0.001). For kyphotic patients, sagittal Cobb angle improved from 80.28 ± 26.59 to 45.71 ± 6.57 (pvalue< 0.001). In kyphoscoliotic cases, coronal and sagittal Cobb angles improved from 43.75 ± 22.86 and 71.25 ± 8.53 to 13.75 ± 4.78 and 36.25 ± 4.78 respectively (p-value=0.003). 10 percent of patients had transient root symptoms. There was no spinal cord lesion, and 4 patients suffered deep infections.
Conclusion: Posterior-only approaches with POs have successful outcomes in treatment of severe spinal deformities including scoliosis, kyphosis or kyphoscoliosis.
Keywords
Spinal deformity, Posterior osteotomy, Spinal deformity, Kyphosis, Scoliosis
Introduction
Severe spinal deformity is a rare condition that beside its negative impact on a person's appearance can cause significant pulmonary function limitations and neuromuscular disorders [1]. This demanding and prospective deformity is defined as abnormal sagittal and coronal curvature of spine [2] and involves all age ranges and genders while due to more flexible spinal column of youth, its related disabilities among elderly and youth don’t have similar pattern. Thus, the aim of the treatment in juvenile cases in addition to achieving patient’s satisfaction due to having less deformed spine is to balance coronal and sagittal support and prevention of future complications such as spinal cord compression [3].
There is still a great concern and controversies in selecting the best options of treatment in severe rigid spinal deformities. Variety of surgical methods has been recommended while the outcomes and complications of them are controversial. These methods include anterioronly, circumferential (anterior and posterior) and posterior-only approaches. The best technique should be selected by a surgeon based on type of deformity, aim of operation, curve magnitude, surgeons' abilities and experience [4-6].
Osteotomy techniques including pedicle subtraction osteotomy (PSO), Smith-Peterson osteotomy (SPO) and vertebral column resection (VCR) are the most common approaches that enable the surgeon to achieve better spinal correction and have considerably developed during recent decades [1,2,7]. In SPO technique we have only posterior elements resection, while PSO involves wider range of vertebral resection including pedicles and vertebral body. So, the range of deformity correction in PSO approach is greater than SPO [2,8].
Some of the studies suggest that VCR as a three-column circumferential technique, is the most efficient approach with best correctional outcomes; while others do not prefer this technique as the first choice because of being a difficult approach in its nature and having high complication rates [1,9]. In the current study, we have assessed outcomes of posterior osteotomy spinal deformity correction approaches regarding their correction ability and complications in educational hospitals of Isfahan, Iran.
Materials and Methods
This is a retrospective cohort study conducted on 57 patients with severe rigid spinal deformities referred to the clinic in 2013-2017 and underwent osteotomy surgical procedures with posterior-only approach. Severe spinal deformity includes those deformities that are rigid or have less than 50% flexibility during bending radiography in preoperative assessment [10]. Inclusion criteria were documented spinal deformity based on clinical and imaging findings, presence of 2 years followup records and the patients' consent for participation in the study. The spine surgeon chooses the type of the surgery based on the severity and the type of the deformity; as we used SPO in less rigid, VCR in more rigid cases and PSO is reserved for patients with moderate rigidity. Demographic information of patients (including age and gender), type of spinal deformity (scoliosis, kyphosis and kyphoscoliosis), previous history of spinal surgery, type of current spinal surgery (SPO, PSO and VCR), bleeding during procedure and perioperative complications were entered in a checklist. The study protocol was approved by Ethic Committee of Isfahan University of Medical Sciences (#IR.MUI.MED.REC. 1397.235) (Project code 397380). Patients' physical examinations including motor and sensory function of limbs were recorded. Pre and postoperative upright coronal and sagittal global spine x-rays were performed in all patients, and radiographic parameters, including Cobb coronal and sagittal angle was measured. All of this information was also obtained within 6 months and two years of follow up. Postoperative correction was measured as following:
(Preoperative Cobb angle-Postoperative Cobb angle)*100/Preoperative Cobb angle
We needed the pre and post-operative radiographies only in the deformed segments, not the whole spine. Obtained data were analyzed using SPSS-25 (IBM; The United States). Descriptive data were presented in mean and percentages. For analytics, Friedman Test, Kruskal-Wallis Test and Fisher's Exact Test were utilized. p-value<0.05 was considered significant.
Results
A total number of 57 patients including 28 males (49.71%) and 29 females (50.9%) with mean age of 21.80 ± 7.50 years (range: 8 years-38 years) were entered this study. Table 1 presents demographic information of studied population according to their type of spinal deformity.
| Variables | Type Of Deformity | |||
|---|---|---|---|---|
| Scoliosis (n=32) | Kyphoscoliosis (n=4) | Kyphosis (n=21) | ||
| Age (year) | Mean ± SD | 20.78 ± 6.86 | 17.25 ± 4.27 | 23.29 ± 7.37 |
| Gender N (%) | Female | 21 (72.4) | 3 (10.3) | 5 (17.2) |
| Male | 11 (39.3) | 1 (3.6) | 16 (57.1) | |
| Type of Surgery N (%) | VCR | 21 (56.6) | 2 (50.0) | 3 (14.3) |
| PSO | 10 (31.3) | 0 (0.0) | 10 (47.6) | |
| Asymmetric SPO | 1 (3.3) | 2 (50.0) | 8 (38.1) | |
| Type of spinal deformity N (%) | Congenital scoliosis | 11(34.4) | 0 (0.0) | 11(34.4) |
| Idiopathic scoliosis | 16 (50.0) | 0 (0.0) | 0 (0.0) | |
| Neuromuscular scoliosis | 4 (12.5) | 0 (0.0) | 0 (0.0) | |
| Paralytic scoliosis | 1 (3.1) | 0 (0.0) | 0 (0.0) | |
| Congenital kyphoscoliosis | 0 (0.0) | 4(100.0) | 0 (0.0) | |
| Congenital kyphosis | 0 (0.0) | 0 (0.0) | 4 (14.3) | |
| Ankylosing Spondilitis | 0 (0.0) | 0 (0.0) | 5 (23.8) | |
| Scheuermann's kyphosis | 0 (0.0) | 0 (0.0) | 13 (61.9) | |
Table 1: Demographic information of studied population based on type of spinal deformity
We observed significant improvement of both coronal and sagittal Cobb angle among all 3 groups of the studied patients (including scoliosis, kyphosis and kyphoscoliosis) during 2 years follow up Table 2. In scoliotic patients coronal Cobb angle improved significantly from 73 to 16, and in those with kyphosis sagittal Cobb angle changed from 80 to 45; finally in kyphoscoliotic patient's coronal and sagittal Cobb angle changed from 43 to 13 and 71 to 36 respectively. Figures 1 and 2 show pre and post-operative images in two of the patients (one with severe congenital kyphoscoliosis and the other with severe neuromuscular scoliosis) as an example. According to Table 2, the Cobb angle in all the patients have changed dramatically in comparison to preoperative Cobb angles; these changes have been unchanged during 2 years follow up because of the nature of a fused spine, indicating acceptable results of this type of surgery.
| Deformity | Variable | Time | p- value | ||||
|---|---|---|---|---|---|---|---|
| Before | After Surgery | 3 month | 6 month | 2 years | |||
| Scoliosis | Coronal cobb (Mean ± SD) | 73.21 ± 10.09 | 17.34 ± 8.61 | 16.4 ± 6.25 | 16.4 ± 6.25 | 16.4 ± 6.25 | <0.001 |
| Kyphosis | Sagittal cobb (Mean ± SD) | 80.28 ± 26.59 | 43.66 ± 7.43 | 43.66 ± 7.43 | 45 ± 5.70 | 45.71 ± 6.57 | <0.001 |
| Kyphoscoliosis | Coronal cobb (Mean ± SD) | 43.75 ± 22.86 | 13.75 ± 4.78 | 13.75 ± 4.78 | 13.75 ± 4.78 | 13.75 ± 4.78 | 0.003 |
| Sagittal cobb (Mean ± SD) | 71.25 ± 8.53 | 36.25 ± 4.78 | 36.25 ± 4.78 | 36.25 ± 4.78 | 36.25 ± 4.78 | 0.003 | |
Table 2: Coronal and sagittal Cobb’s angle change during two-year follow-up of patients under posterior approach osteotomies.
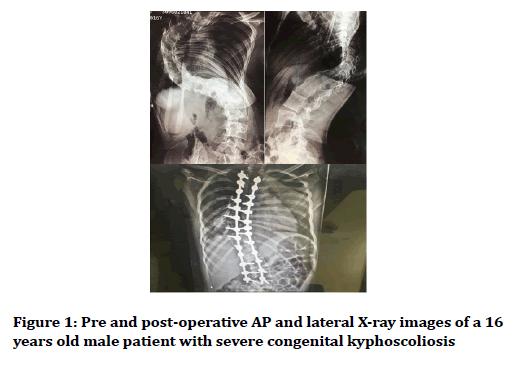
Figure 1. Pre and post-operative AP and lateral X-ray images of a 16 years old male patient with severe congenital kyphoscoliosis
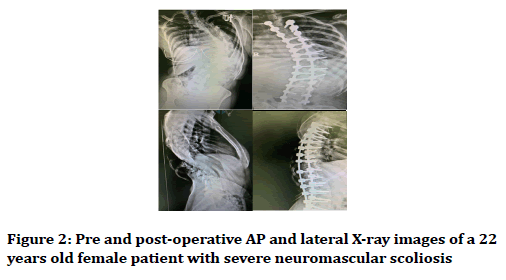
Figure 2. Pre and post-operative AP and lateral X-ray images of a 22 years old female patient with severe neuromascular scoliosis
We used neuro-monitoring in 15 patients and in approximately 10% of patients neurological impairment occurred during procedure. All of neurological deficit presentations were root associated and rehabilitated within two months. There was no spinal cord lesion, and 4 patients suffered deep infections required repeated irrigation and debridement. Proximal junctional failure occurred only among 3 out of 57 patients. In average 1100 cc bleeding occurred during operation leading to mean 1.4 unit of packed red blood cell transfusion. Table 3 represents all complications in details.
| Variables | Type of Deformity | |||
|---|---|---|---|---|
| Scoliosis (N=32) | Kyphoscoliosis (N=4) | Kyphosis (N=21) | ||
| Bleeding (ml) | Mean ± SD | 1187.18 ± 591.68 | 1750.00 ± 378.50 | 900.00 ± 518.65 |
| Blood transfusion (pack cells) | Mean ± SD | 1.40 ± 1.01 | 2.25 ± 0.1995 | 0.85 ± 0.79 |
| Infection | No | 30 (93.75) | 4 (100.0) | 19 (90.5) |
| Yes | 2 (6.2) | 0 (0.0) | 2 (9.5) | |
| Neurological impairment | No | 31 (96.9) | 3 (75.0) | 17 (81.0) |
| Yes | 1 (3.1) | 1 (25.0) | 4 (19.0) | |
| Proximal junctional failure | No | 30 (93.8) | 4 (100) | 20 (95.2) |
| Yes | 2 (6.2) | 0 (0) | 1 (4.8) | |
| Neuro-monitoring | No | 22 (68.8) | 1 (25.0) | 19 (90.5) |
| Yes | 10 (31.2) | 3 (75.0) | 2 (9.5) | |
Table 3: Complications associated with each type of spinal deformity following posterior osteotomy
Discussion
Treatment of spinal deformities is of great concern worldwide; the surgical procedures are demanding and are considerably invasive. Thus various techniques have been introduced with different success and failure rates [2,11,12]. Conservative medical therapies should be strongly considered instead of early surgical treatment. Only nonresponses to medical therapy, progressive deformities or neurological deficit occurrence should be considered for surgical procedures [13].
Moderate cases of spinal deformity have been welltreated with posterior, anterior and their combination techniques while approach to severe rigid spinal deformities is more challenging [14]. Posterior approach for severe rigid spinal deformity correction has promoted in recent decades and its superiorities have been explained by different studies [15,16]. Spinal osteotomies are now the most favored approach for correction of the severe rigid spinal deformities. While this approach was primarily considered for antero-posterior procedures, posterior-only approach is more favored in recent years [17]. Findings of this study emphasizes on successful outcomes of sagittal Cobb angle correction following posterior osteotomic approach for patients with kyphotic with and/or without scoliotic deformities.
There is no unanimous approach for treatment of kyphotic spinal deformities, though various posterior approaches have been introduced since recent decades. Anterior, posterior and combined approaches are among accepted procedures while their selection is correlated with the degree of expected correction, etiology of the deformity, preferences of the surgeon [18,19]. Similar to this study, Mo et al. tried to assess different posterior approach osteotomies considering their ability of kyphotic deformity correction. They presented acceptable outcomes of kyphosis correction through all of mentioned techniques of SPO, PSO and VCR. However, their degree of correction and complications were different from this study. All of the techniques were successful regarding anatomic balance, spinal alignment correction and neurogenic deficit corrections [20]. Mentioned factors were presented by other authors as well [21-23].
The other aspect of this study was the coronal Cobb angle, assessed among those with scoliosis and kyphoscoliosis. Two-year follow-up of this study showed significant coronal Cobb angle improvement following different types of posterior osteotomies.
Enercan et al. performed a similar study in 2013 assessing variety of osteotomic techniques considering sagittal and coronal spinal deformity correction. The most successful outcomes were achieved through VCR surgery. A great concern they were struggling with was about sagittal alignment. In fact they presented that persistent spino-pelvic alignment for achieving long-term satisfactory outcomes is the most important issue that should be considered by expert surgeons. In this regard, further studies with long term follow-up periods are strongly recommended [2]. Several prior studies have assessed posterior osteotomies and declared successful outcomes [23-25].
Another issue that should be considered for making decision about surgical spinal deformity treatment is its complications. We have found considerable amount of blood loss yield to transfusion. Furthermore, in approximately 10% of patients neurological impairment occurred during procedure. All of neurological deficit presentations were root associated and rehabilitated within two months. In addition, 4 patients experienced deep infections following osteotomies. These complications including instability, neurological injuries and intraoperative complications have been abundantly reported as well [26,27]. In this study, proximal junctional failure occurred only among 3 out of 57 patients which is considerably fewer than what has been previously mentioned by other authors [28].
Conclusion
In general, considering coronal and sagittal Cobb angle correction along with low incidence of complications revealed successful outcomes of posterior-only osteotomy approach for treatment of severe rigid spinal deformities. Based on findings of the current study, posterior-only approach was accompanied with successful outcomes regarding correction of sagittal and coronal Cobb angle, with low incidence of complications in this two-years follow up cohort study.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- Yang C, Zheng Z, Liu H, et al. Posterior vertebral column resection in spinal deformity: A systematic review. Eur Spine J 2016; 25:2368-75.
- Enercan M, Ozturk C, Kahraman S, et al. Osteotomies/spinal column resections in adult deformity. Eur Spine J 2013; 22:254-64.
- Kim SS, Cho BC, Kim JH, et al. Complications of posterior vertebral resection for spinal deformity. Asian Spine J 2012; 6:257-65.
- Silva FE, Lenke LG. Adult degenerative scoliosis: Evaluation and management. Neurosurg Focus 2010; 28:E1.
- Dorward IG, Lenke LG. Osteotomies in the posterior-only treatment of complex adult spinal deformity: A comparative review. Neurosurg Focus 2010; 28:E4.
- Cho W, Lenke L. Vertebral osteotomies review of current concepts. Musculoskeletal Rev 2010; 5:46-9.
- Youssef J, Orndorff D, Patty C, et al. Current status of adult spinal deformity. Global Spine J 2013; 3:051-62.
- Barton C, Noshchenko A, Patel V, et al. Risk factors for rod fracture after posterior correction of adult spinal deformity with osteotomy: A retrospective case-series. Scoliosis 2015; 10:30.
- Lenke LG, Newton PO, Sucato DJ, et al. Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: A multicenter analysis. Spine 2013; 38:119-32.
- Bridwell KH, Lenke LG, Baldus C, et al. Major intraoperative neurologic deficits in pediatric and adult spinal deformity patients: incidence and etiology at one institution. Spine 1998; 23:324-31.
- Smith JS, Shaffrey CI, Ames CP, et al. Assessment of symptomatic rod fracture after posterior instrumented fusion for adult spinal deformity. Neurosurgery 2012; 71:862-8.
- Tang JA, Leasure JM, Smith JS, et al. Effect of severity of rod contour on posterior rod failure in the setting of lumbar pedicle subtraction osteotomy (PSO): A biomechanical study. Neurosurgery 2012; 72:276-83.
- Jo DJ, Kim YS, Kim SM, et al. Clinical and radiological outcomes of modified posterior closing wedge osteotomy for the treatment of posttraumatic thoracolumbar kyphosis. J Neurosurg Spine 2015; 23:510-7.
- Diab MG, Franzone JM, Vitale MG. The role of posterior spinal osteotomies in pediatric spinal deformity surgery: Indications and operative technique. J Pediatr Orthop 2011; 31:S88-98.
- Hamzaoglu A, Alanay A, Ozturk C, et al. Posterior vertebral column resection in severe spinal deformities: A total of 102 cases. Spine 2011; 36:E340-E4.
- Ozturk C, Alanay A, Ganiyusufoglu K, et al. Short-term X-ray results of posterior vertebral column resection in severe congenital kyphosis, scoliosis, and kyphoscoliosis. Spine 2012; 37:1054-7.
- Kose KC, Bozduman O, Yenigul AE, et al. Spinal osteotomies: Indications, limits and pitfalls. EFORT Open Rev 2017; 2:73-82.
- Schoenfeld AJ, Wood KB, Fisher CF, et al. Posttraumatic kyphosis: current state of diagnosis and treatment: Results of a multinational survey of spine trauma surgeons. Clin Spine Surg 2010; 23:e1-8.
- Munting E. Surgical treatment of post-traumatic kyphosis in the thoracolumbar spine: Indications and technical aspects. Eur Spine J 2010; 19:69-73.
- Mo AZ, Sama AA. Posterior osteotomies for kyphosis correction. Semin Spine Surg 2017.
- Bridwell KH. Decision making regarding Smith-Petersen vs. pedicle subtraction osteotomy vs. vertebral column resection for spinal deformity. Spine 2006; 31:S171-S8.
- Cho KJ, Bridwell KH, Lenke LG, et al. Comparison of Smith-Petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine 2005; 30:2030-7.
- Boachie-Adjei O, Bradford DS. Vertebral column resection and arthrodesis for complex spinal deformities. J Spinal Disord 1991; 4:193-202.
- Bradford DS, Tribus CB. Vertebral column resection for the treatment of rigid coronal decompensation. Spine 1997; 22:1590-9.
- Gill JB, Levin A, Burd T, et al. Corrective osteotomies in spine surgery. JBJS 2008; 90:2509-20.
- Suk SI, Chung ER, Kim JH, et al. Posterior vertebral column resection for severe rigid scoliosis. Spine 2005; 30:1682-7.
- Bradford D, Boachie-Adjei O. One-stage anterior and posterior hemivertebral resection and arthrodesis for congenital scoliosis. J Bone Joint Surg Am 1990; 72:536-40.
- Barton C, Noshchenko A, Patel VV, et al. Different types of mechanical complications after surgical correction of adult spine deformity with osteotomy. World J Meta-Anal 2017; 5:132-49.
Author Info
Mohammad Reza Etemadifar1, Mehdi Koushkzari1*, Ali Andalib1 and Mahsa Behnemoon2
1Department of Orthopedic Spine Surgery, Isfahan University of Medical Sciences, Isfahan, Iran2Department of Cardiology, Urmia University of Medical Sciences, Urmia, Iran
Citation: Mohammad Reza Etemadifar, Mehdi Koushkzari, Ali Andalib, Mahsa Behnemoon, Correction of severe spinal deformities using posterior osteotomy in young patients: What are the outcomes?, J Res Med Dent Sci, 2019, 7(2): 214-218.
Received: 04-Apr-2019 Accepted: 27-Apr-2019
