Original Article - (2019) Volume 7, Issue 2
Comparison of the Effectiveness of Unified Transdiagnostic Therapy (UP-C) with Cognitive Behavioral Therapy (CBT) on Depression Anxiety Symptoms in Child Workers: ''Child Labour"
Leila Salek Ebrahimi1, Mohsen Saberi Isfeedvajani2,3, Abolfazl Mohammadi4, Sogand Ghasemzadeh5, Abbas Masjedi Arani1* and Seyed Hasan Saadat6
*Correspondence: Abbas Masjedi Arani, Faculty of Medicine, Department of Clinical Psychology, Shahid Beheshti University of Medical Sciences, Tehran, Iran, Email:
Abstract
Background: The presented study investigated the efficacy and rationale of the unified protocol for transdiagnostic treatment of emotional disorders (UP-C) for providing a transdiagnostic based therapeutic strategy as a comparison with cognitive-behavioral therapy (CBT).
Methods: All subjects (female children) with a principal anxiety disorder and depression were included in the study (15 patients), implicating 3-month follow-up period. Furthermore, all subjects were randomly assigned to receive UP-C, and CBT, following a wait-list control. Female children age ranged from 8 years to 11 years. In the current study, child workers ages 8 years-11 years and post-treatment and three months’ follow-up data were then considered for statistical analysis.
Results: Findings revealed that effect of kind of group on depression anxiety was remarkably significant, depression and anxiety were changed significantly in different stages of pre-treatment, post-treatment and follow-up. Moreover, a significant difference was found between the pre-treatment and the post-treatment in the CBT and UP-C group. Additionally, the result presented herein, indicated the decreasing trend of depression anxiety in the two intervention groups (CBT and UP-C). The decrease in both depression anxieties in the UP-C group were found to be greater when comparing with the CBT group. But, these trends were significantly greater in UP-C group.
Conclusion: UP-C was effective in depression anxiety regulation as compared with CBT group and resulted in a significant decline in depression anxiety symptoms. UP-C showed higher therapeutic efficacy on indices of depression anxiety as compared to CBT. Although UP-C exhibited promising results, however further greater RCTs are required to evaluate UP-C effectiveness in different conditions and other co-occurring psychological conditions.
Keywords
Depression anxiety, Female, Therapeutic, Children, Statistical analysis
Introduction
Emotional disorders (depression and anxiety disorders) represent one of the largest causes of impotence universal and are extremely prevalent mental health problems with a lifetime prevalence of up to 29% for anxiety disorders and 19% for depressive disorders and comorbidity rates ranging among 40% and 80 % [1,2]. Anxiety disorders are among the disorders that affect children and adolescents. Almost 6.5% of children and adolescents (CYP) experience anxiety disorders all over the word [3]. Children are suffering from a wide range of anxiety disorders (e.g., generalised anxiety disorder, separation anxiety disorder, social phobia, agonophobia, etc.) [4]. Clinical levels of fear and anxiety can cause severe discomfort to children and their families; they are capable of affecting their level of functioning (e.g., poorer academic and social performance, sleep problems, etc.) [5-10].
The high prevalence of anxiety disorders causes significant economic burden on society [11]. Of course, a wide range of prevalence (from 2.6% to 41.2%) has been reported in various studies [5].
Reports have indicated that boys at younger ages may show anxiety disorders in comparison to girls. The prevalence of age-related anxiety disorders is believed to be an upward trend [12-14]. Separation anxiety disorder is common in early childhood, while social-l phobia is more often seen in adolescence [15].
Appropriate psychological therapies are now provided in CYP for anxiety disorders. Cognitive-behavioral therapy (CBT) is considered to be a valid therapeutic approach for anxiety disorders in CYP [16], but the benefits of treatment are not available to most anxious people [17-19].
CYP are usually faced with remarkable barriers accessing mental health services, e.g., economic conditions in the low and middle income countries, referral procedures, lower ratio of mental health professionals to resident, long distances, waiting times, referral procedures, costs, privacy concerns, social stigma, fear of peer rejection [20-24].
Effective CBT treatment for CYP with anxiety disorders can be able to prevent further consequences [25-27]. Additionally, the evaluation of long term outcomes appears to be necessary in providing the effectiveness of treatment in CYP with anxiety disorders [27,28].
It is nevertheless of great importance to performed easily available, early therapeutic approach for anxious CYP. The long-term effects of CBT have been previously revealed for mixed anxiety disorders in children [29-32]. Various formats for CBT have been decided including internet based CBT (ICBT) and group cognitive behavioral therapy (GCBT) [27].
Previous studies have indicated that internet-based ICBT can be applicably used for patients without assess to inperson therapies, especially in terms of anxiety disorders, depression and sleep disorders [33-35]. ICBT is describe to be effectively useful tool in treating many mental health disorders with cost effective manner in rural and urban areas, across different cultures and languages with a global scale [36]. However, long-term outcome are remarkably different as reported previously (i.e., lack of the principal anxiety diagnosis, etc.) [32].
On the other hand, the effectiveness of GCBT has been previously evaluated for developing therapeutic approach in patients with anxiety disorders [37,38].
CBT group-based interventions have been performed for activating favorable access to evidence-based therapies and good clinical efficiency where group models are capable of providing opportunities for reinforcement, and social support. However, further investigations are required to clarify fidelity and adaptation in establishing a well CBT group program [39].
Disorders in Adolescents (UP-A) and Unified Protocol for Transdiagnostic Treatment of Emotional Disorders in Children (UP-C), which had efficacy for treatment of both depression anxiety [40]. However, further studies are needed to evaluate cognitive-behavioral transdiagnostic therapy based on unified approach in a specific culture as a comparison with CBT.
Therefore, in this study, authors aimed the efficacy and rationale of UP-C for providing a transdiagnostic based therapeutic strategy as a comparison with CBT.
Materials and Methods
This was a semi-experimental research with pre-test, post-test and control group. The statistical population was all of the child labourers in Tehran. The participants were 45 girls aged between 8 years-11 years. They were members of an Institute for the empowerment of child Labourers named "Mehromah" in Tehran, during April to December in year 2018. Sampling was done purposefully. Participants were selected by semi-structured interviews for Kiddie Schedule for Affective Disorders and Schizophrenia and lifetime version (K-SADS-PL) [41], and according to inclusion and exclusion criteria. Finally, 45 child workers who had pre-clinical symptoms of depression anxiety were selected.
This interview was used to exclude other psychiatric disorders. This semi-structured interview tool was developed by Kaufman et al. [42] to assess the current and past course of psychiatric symptoms and disorders in children and adolescents based on the DSM-IV criteria. The average time required to conduct this interview is 45 minutes, which is usually increased to 90 minutes in patients. Validity and reliability of the Persian version of this tool have been approved for 112 individuals in the clinical section of the child and adolescent department of Roozbeh Hospital [43].
Demographic characteristics questionnaires as well as Revised Children’s depression anxiety Scale-(RCADS-25) were completed and the relevant pre-test scores were also recorded.
The RCADS is a 47-item questionnaire, developed by Ebesutani et al. [44]. It is a self-report scale that assesses a range of psychological disorders in child and adolescent according to DSM-IV criteria. It yields an overall score for anxiety and depressive symptoms. It has been reported to have acceptable reliability and validity in clinical and non-clinical adolescent samples. The Internal consistency of the scale was 0.83 [45].
During an introductory session before the intervention, the consent was signed by both the child and one of her parents. The demographic characteristics questionnaire, the R-CADS revised scale of children’s depression anxiety (R-CADS) was completed and their pre-test scores were recorded. In the next step, the participants were randomly assigned in to three groups. The experimental groups received the Unified Transdiagnostic Therapy. The other group received Cognitive-Behavior Therapy and control group did not receive any formal intervention. After completion of the intervention (post-test) and also three months after it (Follow up), the questionnaires were completed again. All participants in all groups were present in all treatment sessions and were not absent. In addition, all participants participated in all three stages of pre-test, post-test and Follow up (Figure 1).
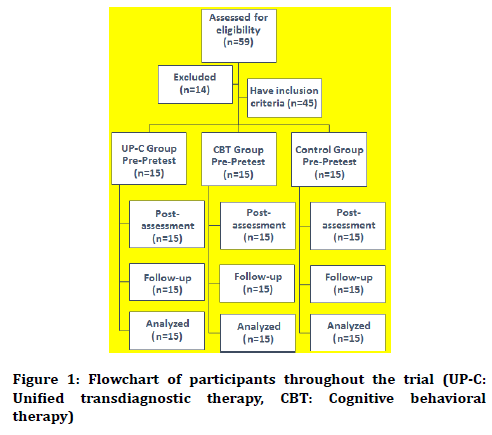
Figure 1. Flowchart of participants throughout the trial (UP-C: Unified transdiagnostic therapy, CBT: Cognitive behavioral therapy)
Inclusion criteria included: 1) Membership in Children's Empowerment Center in Tehran, affiliated to the Child Labor Assistance Network, 2) Having pre-clinical symptoms of depression anxiety, 3) Age range from 8 to 11 years, 4) The voluntary participation of research participants based on the written informed consent.
Exclusion criteria included: 1) Having a psychiatric disorder in the clinical setting, 2) Having chronic medical condition, 3) Receive similar psychological intervention simultaneously with the implementation of this research, 4) Simultaneous use of medication with intervention or within one month before intervention, 5) Dissatisfaction of individuals or their parents with the continuation of treatment during the intervention. Anxiety-depression was the score that the subject received in the R-CADS questionnaire.
Statistical analysis
The sample size of the present study was based on Cohen table (test power of 0.08), the alpha level of 0.05 (twoway test), effect size 0.8 in each group of 10, and considering the probability of falling, 15 people in each group and a total of 45.
In the present study, the data was analyzed using SPSS-25 software. The results of statistical analysis are presented in two parts including descriptive and inferential results. In the descriptive section, the demographic and main variables were described. In the inferential section, the questions and hypotheses of the research were investigated and the differences between the groups were then evaluated using repeated measurements analysis of variance (ANOVA).
Results
Age
Table 1 shows frequency percentage of age in three groups. The age of subjects ranged from 8 years to a maximum of 11 years. In the UP-C group and in the control group, two-thirds of children, 67% were 8 years or 9 years old. In the CBT, 53% of children, 8 subjects were included as 8 years or 9 years of age. The age of 11 years in all groups had the least frequency.
| Control group | Cognitive-Behavioral Group | Transdiagnostic Therapy Group | Age | |||
|---|---|---|---|---|---|---|
| % | Frequency | % | Frequency | % | Frequency | |
| 26.7 | 4 | 40 | 6 | 33.3 | 5 | 8 years |
| 40 | 6 | 13.3 | 2 | 33.3 | 5 | 9 years |
| 20 | 3 | 26.7 | 4 | 20 | 3 | 10 years |
| 13.3 | 2 | 20 | 3 | 13.3 | 2 | 11 years |
| 100 | 15 | 100 | 15 | 100 | 15 | Total |
Table 1: Frequency of subjects' age status by group
Academic level
Table 2 shows the frequency of educational level by group. The results revealed that the lowest level is the third grade of primary school, and the highest was found to be the sixth grade.
| Control group | Cognitive-Behavioral Group | Transdiagnostic Therapy Group | Grade | |||
|---|---|---|---|---|---|---|
| % | Frequency | % | Frequency | % | Frequency | |
| 26.7 | 4 | 40 | 6 | 33.3 | 5 | Third stage |
| 40 | 6 | 13.3 | 2 | 33.3 | 5 | Fourth quarter |
| 20 | 3 | 26.7 | 4 | 20 | 3 | Fifth grade |
| 13.3 | 2 | 20 | 3 | 13.3 | 2 | Sixth Grade |
| 100 | 15 | 100 | 15 | 100 | 15 | Total |
Table 2: Frequency of students' educational level by group
The findings presented herein demonstrated that twothirds of the subjects (67%) of two groups of UP-C and control group had third and fourth grade of primary school, and 53% of the CBT group were in the third or fourth grade of primary school. The lowest frequency was observed in the UP-C group with the sixth grade of primary school (13%), followed by CBT group (the fourth grade; 13%) and control group (sixth grade; 13%).
Main variables
The main variables are described in Table 3 and the results are reported separately by the groups and the treatment stages. The results were reported using Central Tendency (mean) and scattered (standard deviation) statistics.
| Variable | Stage | Groups | ||
|---|---|---|---|---|
| UP-C | CBT | Control Group | ||
| Stress And Depression | Pre-Treatment | 67.53 ± 4.25 | 67.87 ± 4.46 | 67.67 ± 4.37 |
| Post-Treatment | 67.87 ± 4.12 | 65.80 ± 4.71 | 67.87 ± 5.38 | |
| Follow-Up | 62.27 ± 3.73 | 65.73 ± 4.70 | 67.60 ± 5.21 | |
Table 3: Describing the main variables by groups and the test steps
Investigating the means of depression in the anxiety variable showed that the mean depression anxiety in the control group was not different significantly. The highest difference was observed between the pre-treatment and the post-treatment in the UP-C group. Investigating the means show that the difference between the mean of pretreatment and post-treatment in the UP-C group was determined as 5.66, followed by 2.07 in the CBT group and 0.20 in the control group.
In the following, assumptions of repeated measurements ANOVA were investigated.
Study of statistical assumptions
The repeated measures ANOVA has several assumptions that, if these assumptions are true, the results will be reliable. These pre-assumptions include:
1. There should be no outlier. The box plot has been used to examine outliers in the present study.
Before data analysis and testing the hypotheses, in the stage of the data checking and screening, the values of outliers were investigated. Individuals with unusual sizes in a single or in a combination of variables are called outliers. The presence of outliers can affect the results of the analysis in an undesirable manner. For this reason, most statisticians suggest that outliers should be eliminated before analyzing the data.
Univariate outlier values were detected using Box Plot. The results of the test for detecting outliers using the Box Plot (Figure 2) exhibited that none of the subjects can be considered as extreme and all scores within the range are acceptable and there is no univariate data or outlier that distorts the results.
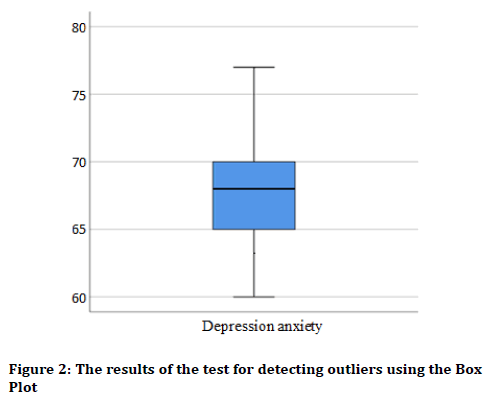
Figure 2. The results of the test for detecting outliers using the Box Plot
Depression anxiety
The distribution of dependent variables in groups should be normal. This assumption was evaluated using kurtosis and skewness statistics and the Shapiro–Wilk test. Results are reported in Table 4.
| Variable | The significance level Shapiro-Wilk test | Skewness | |
|---|---|---|---|
| Stress and depression | 0.334 | 0.344 | 0.099 |
Table 4: Investigating the normality of distribution of variables using skewness and kurtosis values
In terms of skewness and kurtosis measures, if the values of these statistics are between -2 and +2, are known as the standard normal distribution. In the Shapiro-Wilk test, if the level of significance exceeds the 0.05, it indicates the distribution of variables is normal.
Given that all variables are obtained between -2 to +2, and the skewness values for all variables are obtained between -2 to +2, it can be concluded that, all variables have normal or near normal distribution; therefore, distribution of all variables can be considered as normal distribution.
According to the results of Shapiro-Wilk test, the significance level for all variables was considered to be greater than the value of 0.05, indicating normal distribution.
The error covariance should be also identical. The last assumption of the variance on repeated measures is that the covariance of the dependent variables error should be the identity matrix. This test is similar to the Levine test in relation to the homogeneity of the variance of the two groups.
Mauchly's sphericity test is used to test this assumption, and if the significance level of this test exceeds 0.05, the assumption is confirmed. In the present study, this assumption was not confirmed in any of the tests. As a result, according to statistical texts, an epsilon correction should be used, which means that the results of the Huynh-Feldt correction were reported.
Investigating the effectiveness of interventions
Comparison of the effectiveness of interventions on depression anxiety
The results of analysis of variance on repeated measures have been reported in Tables 5-7. In Table 5, the Intrasubject results were presented to examine the effect of time (mean difference at different stages) and the results among the subjects (the effect of two types of intervention on the average) aimed to investigate the effect of the groups.
| Effect source | Sum of squares | Degrees of freedom | Average squares | F-value | p-value | Effect size |
|---|---|---|---|---|---|---|
| Group | 469.57 | 2 | 234.79 | 18.89 | 0.001> | 0.48 |
| Time | 3.87 | 1 | 3.87 | 5.69 | 0.022 | 0.122 |
| Time and group | 1.66 | 2 | 0.83 | 1.22 | 0.306 | 0.056 |
Table 5: The test of the analysis of variance on repeated measures to compare the effects of time and group
| Group | Comparison | Difference in averages | Standard error | p-value |
|---|---|---|---|---|
| Transdiagnostic Therapy | Pre-test with post-test | 5.67 | 0.814 | 0.001> |
| Pre-test with follow-up | 5.27 | 0.568 | 0.002 | |
| Post-test and follow-up | -0.4 | 0.363 | 0.288 | |
| Cognitive-behavioral therapy | Pre-test with post-test | 2.07 | 0.521 | 0.001 |
| Pre-test with follow-up | 2.13 | 0.568 | 0.002 | |
| Post-test and follow-up | 0.067 | 0.182 | 0.719 | |
| Control | Pre-test with post-test | -0.2 | 0.439 | 0.655 |
| Pre-test with follow-up | 0.07 | 0.483 | 0.892 | |
| Post-test and follow-up | 0.267 | 0.371 | 0.484 |
Table 6: Paired comparison of mean depression anxiety in different stages by groups
| Stages | Mean | Mean | Mean | F-value | p-value |
|---|---|---|---|---|---|
| Transdiagnostic group | Cognitive-behavioral group | Control group | |||
| Pre-test | 67.53 | 67.87 | 67.67 | 0.022 | 0.979 |
| Post-test | 61.87 b | 65.80 ab | 67.87 a | 6.14 | 0.005 |
| Follow up | 62.27 b | 65.73 ab | 67.60 a | 5.22 | 0.009 |
Table 7: Comparison of mean depression anxiety in three groups with Tukey post hoc test
Table 5 demonstrated the corrected results associated with the Huynh-Feldt test. This test examines whether the average depression anxiety was different at different stages (pre-treatment, post-treatment, and follow-up). Regarding to the results, the time showed a significant effect on depression anxiety (p<0.05 and F=5.69). This means that the mean depression anxiety has changed significantly in different stages of pre-treatment, posttreatment and follow-up. The effect size or partial eta square is 0.122. The interaction of time and group was also significant (p<0.05). It has been revealed that the effect of time on different groups (UP-C, CBT, and control) was different.
According to the Inter-subjects results, the effect of the group (interventions made) on depression anxiety was significant (p<0.05 and F=18.89). This means that the treatment has been effective in depression anxiety and interventions have led to a significant change in mean depression anxiety in post-treatment and follow-up. The effect size obtained is equal to 0.480, as indicated in Table 5, it can be concluded that the level of depression anxiety has changed significantly between at least two groups.
According to the results presented herein, there is a significant difference between the pre-treatment and the post-treatment in UP-C group and CBT group (p<0.05). Furthermore, in both therapy groups, there was a significant difference between pre-treatment and followup (p<0.05). No significant difference was found between the different stages in the control group (p>0.05). In addition, post-treatment and follow-up scores in both treatment groups was not different significantly and was almost the same (p>0.05) (Table 6).
Figure 3 is the linear diagram of depression anxiety, reported by groups. The trend diagrams show a decreasing trend of depression anxiety in the two treatment groups. The decrease in depression anxiety in the Transdiagnostic group (UP-C) is greater than the cognitive behavioral group (CBT). Scores in the control group do not show a marked change in the stages.
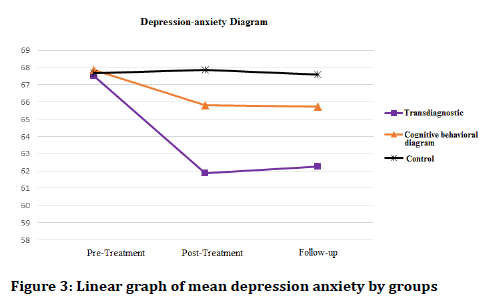
Figure 3. Linear graph of mean depression anxiety by groups
The results of Intera-group comparison are shown in Table 7. The scores of pre-treatment, post-treatment and follow up scores in three groups is compared using Tukey's pocket post hoc test. Regarding to the post hoc test results, the mean pre-treatment in the three groups is almost the same (p>0.05).
Based on the findings presented herein, the mean posttreatment stage was found to be significantly different in the three groups (p<0.05). According to the results of the paired comparison, the mean of the CBT was significantly lower than that of the control group (p<0.05). But, no difference was observed between the UP-C and the CBT groups with the control group. The lowest mean in the post-intervention was related to the UP-C group.
According to the results, the mean follow-up stage was revealed to be significantly different in the three groups (p<0.05). Based on the findings of the paired comparison, the mean of the UP-C group was significantly lower as compared to the control group (p<0.05). Additionally, no significant difference was found between the UP-C group and the CBT group with the control group. The lowest average in the follow-up phase was revealed to be related to the UP-C.
Discussion
This study was aimed to present the efficacy and rationale for providing a transdiagnostic based therapeutic strategy to aid in the development of this approach. In the current study, 15 children ages 8 years-11 years with subclinical symptoms of depression anxiety were divided in 3 group, and post-treatment and three months’ follow-up data was then considered for statistical analysis. The data presented here indicated that effect of time and kind of group on depression and anxiety was statistically significant as indicated in Table 4. This means that the mean depression and anxiety have changed significantly in different stages of preintervention, post-intervention and follow-up.
The results show that there is a significant difference between the pre-treatment and the post-treatment in the CBT and UP-C group. In addition, there was a significant difference between pre-treatment and follow-up in both intervention groups. Furthermore, the results demonstrated the decreasing trend of depression anxiety in the two treatment groups. The decrease in depression and anxiety in the UP-C group was found to be greater than the CBT group. As a matter of fact, our findings revealed a remarkable decease in depression and anxiety among subjects who received UP-C.
These results are consistent with variety of studies [46-48], which evaluated outcome of UP-C; found that transdiagnostic treatment can be affectively useful for treating a range of emotional disorders. The effectiveness of CBT treatment in decreasing further consequences of anxiety disorders in CYP has been reported [25-27]. The long-term effects of CBT have been suggested for mixed anxiety disorders in children [29-32]. However, it is of great importance to performed easily available, early therapeutic approach for anxious patients.
An increasing body of evidences suggests RCT results effectiveness of the UP with anxious and depressed adults [46,49]. Recently, developmental modifications of the UP have been conducted for younger children (6 years-12 years old) by using a group intervention protocol, where promising initial findings were found from an open trial investigation [50].
Transdiagnostic approaches including UP-C and UP-A has been provided as a set of core treatment principles focuses on targeting multiple disorders, particularly emotional disorders as a maladaptive coping strategy [40]. Previous studies indicated the effectiveness of transdiagnostic treatment for improving anxiety disorders [51]. Transdiagnostic strategy has been indicated to be potentially capable of conferring both clinical and practical advantages based on a single diagnostic manual [52]. Transdiagnostic approach is simultaneously capable of addressing symptoms of cooccurring situation via targeting common processes [53,54]. Transdiagnostic treatments have been previously described to address comorbidity [55]. The efficacy of UP-C and UP-A has been revealed for anxiety disorders [40,48,49,56]. A study indicated favorable effect of UP-A has been reported on outcome measures over time for treatment of adolescent depression anxiety [57]. Another study by Kennedy et al. [40], revealed that predictors of outcome for transdiagnostic intervention were potentially different when comparing with CBT for anxiety. In addition to disorder-specific CBT for anxiety [58], UP-C has been indicated to be preferably introduced for children with depressive disorder and externalizing symptoms at clinical and subclinical levels [58], where this approach showed flexibly for targeting a range of emotional disorders.
Furthermore, large effect sizes have been demonstrated for UP in anxiety and comorbid depressive disorders, as well as overall clinical severity when comparing with wait-list at post intervention, suggesting ample evidence for a transdiagnostic strategy to the emotional disorders [49]. Additionally, UP-C has been reported to be appropriately treatment of a range of anxiety disorders, including obsessive compulsive disorder, generalized anxiety disorder, panic disorder with agoraphobia, social anxiety disorder with effect sizes in comparison with a therapeutic approach based on disorder-specific symptoms [59]. Similar to outcomes of CBT, transdiagnostic intervention contributed to remarkable symptoms [57,58,60].
It should be taken in to consideration that a large number of studies support the short-term efficacy of the UP as an intervention approach for anxiety and comorbid depressive disorders, the evaluation of the sustainability of intervention gains obtained by such approaches are considered to be critical, because no guarantee can be provided that observed findings be similar to focused CBT interventions [46]. The challenges implicated in aiming a transdiagnostic approach should be considered including selection of subjects for disorder, group normalization, and measures for assessment, design of control treatment group, and analysis [61]. In agreement with our data, results of a study by Arnfred et al. support the application of UP group therapy in depression, and social anxiety disorder compared to diagnosis specific CBT [62] as well as in another research by Mohammadi et al. showed that the UP-T was effective on reduction of depressive symptoms as well as an increase of emotion regulation skills [63]. So, we expect that it will be much more feasible to implement group therapy for depression and anxiety disorders in smaller clinics, within Mental Health Service outside the main cities and in the primary sector. At this point, the application of only one manual will support focused training and supervision, hence increasing the expertise of therapists. In larger clinics, the use of UP could also make it possible to compose groups based on other characteristics than diagnoses i.e. gender, age or life events. Lastly, the use of UP-T for those patients, frequently seen in the depression and anxiety disorders, with comorbidity in the form of two equally important disorders might be particularly advantageous.
On the other hand, several limitations have limited further interoperation. First, the sample size can lead to lack of significant differences in some analyses, 20% drop out in sample size was occurred because of session’s procedure. Future larger-scale efficacy trials are required to reproduce presented findings for emotional disorders in children receiving UP-C. On the other hand, longerterm follow-up is needed to evaluate sustainability of the UP in subjects who finished a full course of UP.
Conclusion
The findings of the current study are the evidence of the applicability and efficacy of this treatment in patients with depression anxiety symptoms in child workers. UPC was found to be superior to CBT therapy in decreasing depression anxiety symptoms in child workers. UP-C was capable of addressing a broad range of symptoms for depression anxiety in child workers. Future research might focus on possible improvements of the UP-C, and a particular focus on those patients who might not benefit from either both methods.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this article.
References
- González-Robles A, García-Palacios A, Baños R, et al. Effectiveness of a transdiagnostic internet-based protocol for the treatment of emotional disorders versus treatment as usual in specialized care: Study protocol for a randomized controlled trial. Trials 2015; 16:488.
- Newby JM, McKinnon A, Kuyken W, et al. Systematic review and meta-analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clin Psychol Rev 2015; 40:91-110.
- Polanczyk GV, Salum GA, Sugaya LS, et al. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry 2015; 56:345-65.
- Klein RG. Anxiety disorders. J Child Psychol Psychiatry 2009; 50:153-62.
- Cartwright-Hatton S, McNicol K, Doubleday E. Anxiety in a neglected population: Prevalence of anxiety disorders in pre-adolescent children. Clin Psychol Rev 2006; 26:817-33.
- Strauss CC, Frame CL, Forehand R. Psychosocial impairment associated with anxiety in children. J Clin Child Psychol 1987; 16:235-9.
- Ialongo N, Edelsohn G, Werthamer-Larsson L, et al. Social and cognitive impairment in first-grade children with anxious and depressive symptoms. J Clin Child Psychol 1996; 25:15-24.
- Seligman LD, Ollendick TH. Cognitive-behavioral therapy for anxiety disorders in youth. Child Adolesc Psychiatr Clin N Am 2011; 20:217-38.
- Mychailyszyn MP, Mendez JL, Kendall PC. School functioning in youth with and without anxiety disorders: Comparisons by diagnosis and comorbidity. Sch Psychol Rev 2010; 39:106-21.
- Peterman JS, Carper MM, Elkins RM, et al. The effects of cognitive-behavioral therapy for youth anxiety on sleep problems. J Anxiety Disord 2016; 37:78-88.
- Greenberg PE, Sisitsky T, Kessler RC, et al. The economic burden of anxiety disorders in the 1990s. J Clin Psychiatry 1999; 60:427-35.
- Esbjørn BH, Hoeyer M, Dyrborg J, et al. Prevalence and co-morbidity among anxiety disorders in a national cohort of psychiatrically referred children and adolescents. J Anxiety Disord 2010; 24:866-72.
- Kendall PC, Compton SN, Walkup JT, et al. Clinical characteristics of anxiety disordered youth. J Anxiety Disord 2010; 24:360-65.
- Ewing DL, Monsen JJ, Thompson EJ, et al. A meta-analysis of transdiagnostic cognitive behavioural therapy in the treatment of child and young person anxiety disorders. Behav Cogn Psychother 2013; 43:562-77.
- Wittchen HU, Stein MB, Kessler RC. Social fears and social phobia in a community sample of adolescents and young adults: Prevalence, risk factors and co-morbidity. Psychol Med 1999; 29:309-23.
- Higa-McMillan CK, Francis SE, Rith-Najarian L, et al. Evidence base update: 50 years of research on treatment for child and adolescent anxiety. J Clin Child Adolesc Psychol 2016; 45:91-113.
- Lawrence D, Johnson S, Hafekost J, et al. The mental health of children and adolescents: Report on the second Australian child and adolescent survey of mental health and wellbeing. Australia: Commonwealth of Australia 2015.
- Merikangas KR, He JP, Burstein M, et al. Service utilization for lifetime mental disorders in U.S. adolescents: Results of the national comorbidity survey-adolescent supplement (NCS-A). J Am Acad Child Adolesc Psychiatry 2011; 50:32-45.
- Heiervang E, Stormark KM, Lundervold AJ, et al. Psychiatric disorders in Norwegian 8- to 10-year-olds: An epidemiological survey of prevalence, risk factors, and service use. J Am Acad Child Psy 2007; 46:438-47.
- Hill C, Creswell C, Vigerland S, et al. Navigating the development and dissemination of internet cognitive behavioral therapy (iCBT) for anxiety disorders in children and young people: A consensus statement with recommendations from the iCBT Lorentz Workshop Group. Internet Interv 2018; 19:1-10.
- Salloum A, Johnco C, Lewin AB, et al. Barriers to access and participation in community mental health treatment for anxious children. J Affect Disord 2016; 196:54-61.
- Collins KA, Westra HA, Dozois DJ, et al. Burns Gaps in accessing treatment for anxiety and depression: Challenges for the delivery of care. Clin Psychol Rev 2004; 24:583-616.
- Gulliver A, Griffiths KM, Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: A systematic review. BMC Psychiatry 2010; 10:113.
- Stjerneklar S, Hougaard E, Nielsen AD, et al. Internet-based cognitive behavioral therapy for adolescents with anxiety disorders: A feasibility study. Internet Interv 2018; 11:30-40.
- Puleo CM, Conner BT, Benjamin CL, et al. CBT for childhood anxiety and substance use at 7.4-year follow-up: A reassessment controlling for known predictors. J Anxiety Disord 2011; 25:690-6.
- Wolk CB, Kendall PC, Beidas RS. Cognitive-behavioral therapy for child anxiety confers long-term protection from suicidality. J Am Acad Child Adolesc Psychiatry 2015; 54:175-9.
- Kodal A, Fjermestad K, Bjelland I, et al. Long-term effectiveness of cognitive behavioral therapy for youth with anxiety disorders. J Anxiety Disord 2018; 53:58-67.
- Chambless DL, Hollon SD. Defining empirically supported therapies. J Consult Clin Psychol 1998; 66:7-18.
- Benjamin CL, Harrison JP, Settipani CA, et al. Anxiety and related outcomes in young adults 7 to 19 years after receiving treatment for child anxiety. J Consult Clin Psychol 2013; 81:865-76.
- Barrett PM, Duffy AL, Dadds MR, et al. Cognitive-behavioral treatment of anxiety disorders in children: Long-term (6-year) follow-up. J Consult Clin Psychol 2001; 69:135-41.
- Ginsburg GS, Becker EM, Keeton CP, et al. Naturalistic follow-up of youths treated for pediatric anxiety disorders. JAMA Psychiatry 2014; 71:310-8.
- Kendall PC, Safford S, Flannery-Schroeder E, et al. Child anxiety treatment: Outcomes in adolescence and impact on substance use and depression at 7.4-year follow-up. J Consult Clin Psychol 2004; 72:276-87.
- Dever FT, Hunter PV, Hadjistavropoulos T, et al. Ethical and legal considerations for internet-based psychotherapy. Cogn Behav Ther 2010; 39:173-87.
- Mewton L, Smith J, Rossouw P, et al. Current perspectives on internet delivered cognitive behavioral therapy for adults with anxiety and related disorders. Psychol Res Behav Manag 2013; 7:37-45.
- Karbasi A, Haratian A. The efficacy of internet-based cognitive behavioral therapy on the anxiety disorders among adolescent girls. Adv Biomed Res 2018; 7:13.
- Kumar V, Sattar Y, Bseiso A, et al. The effectiveness of internet-based cognitive behavioral therapy in treatment of psychiatric disorders. Cureus 2017; 9:e1626.
- Lau WY, Chan CK, Li JC, et al. Effectiveness of group cognitive-behavioral treatment for childhood anxiety in community clinics. Behav Res Ther 2010; 48:1067-77.
- Lumpkin PW, Silverman WK, Weems CF, et al. Treating a heterogeneous set of anxiety disorders in youths with group cognitive behavioral therapy: A partially nonconcurrent multiple-baseline evaluation. Behav Ther 2002; 33:163-77.
- McHugh RK, Murray HW, Barlow DH. Balancing fidelity and adaptation in the dissemination of empirically supported treatments: The promise of transdiagnostic interventions. Behav Res Ther 2009; 47:946-53.
- Kennedy SM, Tonarely NA, Sherman JA, et al. Predictors of treatment outcome for the unified protocol for transdiagnostic treatment of emotional disorders in children (UP-C). J Anxiety Disord 2018; 57:66-75.
- Birmaher B, Ehmann M, Axelson DA, et al. Schedule for affective disorders and schizophrenia for school-age children (K-SADS-PL) for the assessment of preschool children-A preliminary psychometric study. J Psychiatr Res 2009; 43:680-6.
- Kaufman J, Birmaher B, Brent D, et al. Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): Initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 1997; 36:980-8.
- Ramezani FA, Gharaeei B, Salek EL. Effectiveness of computer-based intervention on improving social skills, face processing and emotion recognition in autistic students. New Psychol Res 2016; 43:81-103.
- Ebesutani C, Chorpita BF, Higa-McMillan CK, et al. A psychometric analysis of the revised child anxiety and depression scales-Parent version in a school sample. J Abnorm Child Psychol 2011; 39:173-85.
- Mohammadi A, Soleimani M, Mohammadi MR, et al. Unified protocol for transdiagnostic prevention of depression and anxiety in Iranian adolescents: Protocol development and initial outcome data. Iran J Psychiatry 2019; 88-101.
- Bullis JR, Fortune MR, Farchione TJ, et al. A preliminary investigation of the long-term outcome of the unified protocol for transdiagnostic treatment of emotional disorders. Compr Psychiatry 2014; 55:1920-7.
- Boisseau CL, Farchione TJ, Fairholme CP, et al. The development of the unified protocol for the transdiagnostic treatment of emotional disorders: A case study. Cogn Behav Pract 2010; 17:102-13.
- Ellard KK, Fairholme CP, Boisseau CL, et al. Unified protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cogn Behav Pract 2010; 17:88-101.
- Farchione TJ, Fairholme CP, Ellard KK, et al. Unified protocol for transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behav Ther 2012; 43:666-78.
- Bilek EL, Ehrenreich-May J. An open trial investigation of a transdiagnostic group treatment for children with anxiety and depressive symptoms. Behav Ther 2012; 43:887-97.
- McEvoy PM, Nathan P, Norton PJ. Efficacy of transdiagnostic treatments: A review of published outcome studies and future research directions. J Cog Psychotherapy 2009; 23:20-33.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub 2013.
- Sauer-Zavala S, Barlow DH. The case for borderline personality disorder as an emotional disorder: Implications for treatment. Clin Psychol Sci Pract 2014; 21:118-38.
- Steele SJ, Farchione TJ, Cassiello-Robbins C, et al. Efficacy of the unified protocol for transdiagnostic treatment of comorbid psychopathology accompanying emotional disorders compared to treatments targeting single disorders. J Psychiatr Res 2018; 104:211-6.
- Brown TA, Campbell LA, Lehman CL, et al. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. J Abnorm Psychol 2001; 110:585-99.
- Queen AH, Barlow DH, Ehrenreich-May J. The trajectories of adolescent anxiety and depressive symptoms over the course of a transdiagnostic treatment. J Anxiety Disord 2014; 28:511-21.
- Ehrenreich-May J, Rosenfield D, Queen AH, et al. An initial waitlist-controlled trial of the unified protocol for the treatment of emotional disorders in adolescents. J Anxiety Disord 2017; 46:46-55.
- Kennedy SM, Bilek EL, Ehrenreich-May J. A randomized controlled pilot trial of the unified protocol for transdiagnostic treatment of emotional disorders in children. Behav Modif 2018; 145445517753940.
- Hofmann SG, Smits JA. Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry 2008; 69:621-32.
- Chu BC, Crocco ST, Esseling P, et al. Transdiagnostic group behavioral activation and exposure therapy for youth anxiety and depression: Initial randomized controlled trial. Behav Res Ther 2016; 76:65-75.
- Gros DF. Design challenges in transdiagnostic psychotherapy research: Comparing transdiagnostic behavior therapy (TBT) to existing evidence-based psychotherapy in veterans with affective disorders. Contemp Clin Trials 2015; 43:114-9.
- Arnfred SM, Aharoni R, Hvenegaard M, et al. Transdiagnostic group CBT vs. standard group CBT for depression, social anxiety disorder and agoraphobia/panic disorder: Study protocol for a pragmatic, multicenter non-inferiority randomized controlled trial. BMC Psychiatry 2017; 17:37.
- Mohammadi F, Bakhtiari M, Masjedi AA, et al. The applicability and efficacy of transdiagnostic cognitive behavior therapy on reducing signs and symptoms of borderline personality disorder with co-occurring emotional disorders: A pilot study. Iran J Psychiatry Behav Sci 2018; 12:e9697.
Author Info
Leila Salek Ebrahimi1, Mohsen Saberi Isfeedvajani2,3, Abolfazl Mohammadi4, Sogand Ghasemzadeh5, Abbas Masjedi Arani1* and Seyed Hasan Saadat6
1Faculty of Medicine, Department of Clinical Psychology, Shahid Beheshti University of Medical Sciences, Tehran, Iran2Medicine, Quran and Hadith Research Center, Baqiyatallah University of Medical Sciences, Tehran, Iran
3Faculty of Medicine, Department of Community Medicine, Baqiyatallah University of Medical Sciences, Tehran, Iran
4Department of Psychiatry, Tehran, Iran
5Faculty of Psychology and Educational Sciences, Department of Psychology and Education of Exceptional Children, University of Tehran, Tehran, Iran
6Behavioral Sciences Research Center, Lifestyle Institute, Baqiyatallah University of Medical Sciences, Tehran, Iran
Citation: Leila Salek Ebrahimi, Mohsen Saberi Isfeedvajani, Abolfazl Mohammadi, Sogand Ghasemzadeh, Abbas Masjedi Arani, Seyed Hasan Saadat, Comparison of the effectiveness of unified transdiagnostic therapy (UP-C) with cognitive behavioral therapy (CBT) on depression anxiety symptoms in child workers: ''Child labour", J Res Med Dent Sci, 2019, 7(2): 122-130.
Received: 26-Mar-2019 Accepted: 15-Apr-2019
