Research - (2021) Volume 9, Issue 1
Comparison of Lympho-Vascular Invasion and Blood Vessel Invasion as a Prognostic Predictor in Carcinomas of the Breast
Abstract
The significant prognostic variables related with bosom malignant growth are far off metastasis and repeat. Both lympho-vascular attack (LVI) and vein intrusion (BVI) are significant courses for metastases to common center points of the lymph and essential metastases. Despite the noteworthiness of vascular interruption as a prognostic factor, there is a flawed point in using vascular assault as a histopathological worldview. The purpose of this examination was to perceive BVI LVI in the perception and rehash of chest damage using an explicit immunohistochemical recolation of the endothelial subtype explicit immuno-histochemical recolor (D2-40 and CD31).
Keywords
Breast malignant growth, CD31 antigen, Monoclonal neutralizer D2-40, Prognosis, Survival
Introduction
Breast cancer is one of the most diagnosed cancers and the leading cause of deaths from cancer among women worldwide [1]. Breast carcinoma has been extensively studied upon and with the availability of vast evidence-based data and literature various treatment modalities have been introduced to treat this life-threatening disease. Although incidence rates are higher in the West, the highest burden for breast cancer is in middle-income countries [2]. Majority of the breast carcinomas are usually asymptomatic, and the usual mode of presentation is an incidental palpable lump or pain and rarely, they present with nipple discharge and skin changes [3]. Breast carcinomas have varying levels of invasion and aggressiveness irrespective of the duration of presentation.
Lymph node metastasis is considered as one of the most important prognostic factors for breast carcinomas [4]. Thus, the recognition of peritumoural lymphatic vessel invasion on histological sections is especially important. In any case, notwithstanding the importance of venous intrusion as a prognostic factor, there is still consideration of the use of venous assault (BVI) as a histopathological basis. Along these lines, the point of this examination was to recognize the job of LVI and BVI in the visualization and repeat of intrusive bosom malignant growth utilizing an endothelial subtype explicit immuno-histochemical recolor (D2-40 and CD31).
Materials and Methods
From 2014 to 2018, information from diagrams and neurotic reports just as tissues from backto- back patients with obtrusive carcinoma of the bosom at Sree Balaji Medical College and Hospital were investigated. Patients who got who had encountered neoadjuvant treatment Similarly, to support the use of D2-40 stains as unambiguous markers in clinical settings, further arranged exams with greater people are essential. Tumor determination was through immunohistochemistry. The test included 80 patients. The median follow-up period was months (35 ±1.02). The patient’s qualities are summarized in Table 1. Tumor size and nodal status were determined by the American Joint Committee on Cancer's TNM system criteria and histological evaluation was conducted using the Bloom and Richardson change in Nottingham to examine criteria [5].
| Characteristics | No. of Patients (%) 80 (100) |
|---|---|
| Age (yr) | |
| <50 | 38 (47.5) |
| ≥50 | 42 (52.5) |
| Tumour size (T stage) | |
| 1 | 41 (51.2) |
| 2 | 33 (41.3) |
| 3 | 4 (5) |
| 4 | 2 (2.5) |
| Lymph node status | |
| 0 | 41 (51.3) |
| 01-Mar | 18 (22.5) |
| 04-Sep | 9 (11.2) |
| ≥10 | 12 (15) |
| Histologic grade | |
| 1 | 15 (19.2) |
| 2 | 28 (35.9) |
| 3 | 35 (44.9) |
| Estrogen receptor status | |
| Positive | 51 (63.7) |
| Negative | 29 (36.3) |
| Progesterone receptor status | |
| Positive | 45 (56.3) |
| Negative | 35 (43.7) |
| HER2/neu expression | |
| Positive | 24 (30) |
| Negative | 56 (70) |
| Ki-67 expression (%) | |
| <20 | 17 (21.5) |
| ≥ 20 | 62 (78.5) |
| D2-40 LVI | |
| Positive | 8 (10) |
| Negative | 72 (90) |
| CD31 BVI | |
| Positive | 18 (22.5) |
| Negative | 62 (77.5) |
| H&E LVI | |
| Positive | 5 (6.2) |
| Negative | 75 (93.8) |
| Recurrence | |
| Yes | 9 (11.3) |
| No | 71 (88.7) |
Table 1: The patient’s qualities.
Procedure
3-4 μm thick segments from each square were put on Poly-L-Lysine covered slides and air dried. The slides were heated at 60°C for 1 hour in tourist oven. Slides were deparaffinized and rehydrated. Trisodium citrate cradle was readied - 1000ml, pH - 6.0. Trisodium citrate cushion was filled the weight cooker with slide bearer. Segments were left in the Tris cushion for around 7-8 minutes or 2 whistles. Slides were then washed in faucet water for 3-5minutes followed by refined water. Endogenous peroxidase was extinguished by dunking slides into a crisp fluid arrangement of 3% peroxide for 15 minutes. Slides were then washed in faucet water for 3-5 Minutes, and refined water followed. Slides were flushed at that point Tris support for every 5 minutes, three changes.
Recognition of antigens in paraffin areas
The essential counter acting agent was included at a weakening chose generally for thirty minutes to 60 minutes. Areas were absorbed Tris cushion for 10 minutes (2 x 5 moment washes). Auxiliary counter acting agent was then included and left for thirty minutes. Areas were again absorbed Tris support for 10 minutes (2 x 5 moment washes). An answer of chromogen, 3,3'- diaminobenzidine (DAB) at 1mg/ml was made in Tris and included. The areas were washed in faucet water. The segments were washed with wash support and counterstained with haematoxylin and again flushed in water for 5 moment.
LVI was Positive when tumor emboli were recognized in D2-40 and H&E recolored vessels, and positive for BVI when tumor emboli were interpreted unequivocally in CD31-recolored vessels (Figure 1). Reports were compared with various parameters such as tumor size, metastasis rate in the lymph center point, hormonal receptor level, human epidermal progression factor receptor2 HER2/new enunciation and rehash.
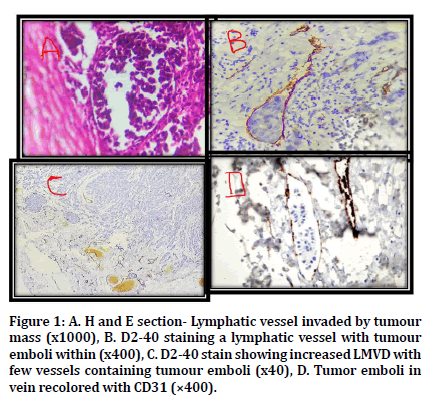
Figure 1. A. H and E section- Lymphatic vessel invaded by tumour mass (x1000), B. D2-40 staining a lymphatic vessel with tumour emboli within (x400), C. D2-40 stain showing increased LMVD with few vessels containing tumour emboli (x40), D. Tumor emboli in vein recolored with CD31 (×400).
Measurable investigation
Coordinated the quantifiable examination using SPSS 12.0 adaptation of the code (SPSS Inc., Chicago, USA). Associations of clinicopathological parameters and rehash with D2-40, CD31, and H and E recoloring were analyzed using chi-square tests. A p-regard of <0.05 was perceived as vital precisely [6].
Results
All patients were female and reached between 28 and 76 years of age (mean, 49.4±10.727). D2- 40 and H&E recolor recognized LVI separately in eight (10 per cent) and five (5.2 per cent) tumors. CD31 recolor perceived BVI in 18 tumors (22.5%). Seven tumors were healthy both for D2-40 LVI and CD31 BVI. Recolored LVI vitality was linked to clinicopathological influences between D2-40 and H&E - Rehashes were connected For D2-40 perceived positive LVI and H&E recolor (independently p=0.014, p=0.037).D2-40 LVI tumors Positive center point metastasis (p=0,022), higher histological (p=0,022) and negative ER (p=0,017) were associated.. Parameters ultimately correlated with the inspiration for H&E recolor LVI included), TNM genius (p=0.036), nodal status (p=0.019) and ER status (p=0.037).
Discussion
Chest carcinoma is known since ages and first recorded chronicled note about chest carcinoma is by the Egyptians in 3000 BC5. It is by and by considered as one of the most broadly perceived illnesses in women and one of the most outstanding purpose behind threatening development passing in women6. As mentioned previously, in situations where BVI could not be interpretedIn the past, LVI was sensed using H and E recolor. Nonetheless, new markers in the healthy histochemical system were found near advances. Using D2-40 as a marker, a few evaluations found LVI to be a notable prognostic factor in chest cancer [7].
For LVI, we used D2-40 to select his relationship with other clinicopathological factors and the conjecture. There was a colossal association between LVI and overall estimate which shows that the LVI area could be a basic marker for conjecture by D2-40 stain [8-10]. Despite a short subsequent period. To confirm findings from other trials, LVI-positive D2-40, and H&E-recolored tumors showed reduced DFS (p=0.008, 0.022, separately). Eight,9 The size of the tumor is one of the most grounded farsighted segments for close by rehash, and tumors more conspicuous than 2 cm are associated with DFS10. In our examination, there was every reservation of being a greater number of in the positive social potential of D2-40 LVI, cases with tumor estimates greater than 2 cm; in any case, no quantifiable importance was considered. In addition, tumor classification is correlated with increasingly deplorable perceptions as tumors display powerful behaviors in higher evaluations [11]. In our findings, the majority of histological review 3 of LVI-positive tumors was consistent with other reports [12], and this may be explained by the assumption that commanding tumors are increasingly appropriate for lymphatic vessels. Exclusively viewed was a huge association Among LVI and ER with 0.017 and 0.037 p-estimates for D2-40 and H&E recolour.. We suggest that prognostic value is given by the LVI skepticism in ER-positive tumors.
Axillary lymph center status is a noteworthy prognostic factor [11], and through the lymph structure the metastatic course is in Braun et al. [13]. Recording the relationship Between LVI and axillary center metastasis, essentially in small (T1) tumors using D2-40 as a marker. Moreover, Wong et al. [14] investigated the immensity of LVI in center negative tumors for the radiation precondition treatment or an axillary investigation to be envisaged. They concluded that LVI negative patients with small tumors had appropriate metastasis for the center point of the lymph and suggested that LVI positive patients receive full radiation therapy nearby axillary research. Likewise, BVI is a critical factor linked to spread of haematogenic tumor cells [15]. We found no significant interaction with other prognostic markers, and BVI was not linked to DFS or rehash.
Conclusion
Whether or not D2-40 and CD31 were gigantic prognostic components was the impetus driving this study. We are crucial to estimate but can also be significant in terms of treatment. If it is possible to fully determine the risk of a patient doing metastasis or rehash, the danger will individualize care. Attempts should be made to pick the prognostic value of LVI and BVI and to discover certain components of the forecast.The positive LVI perceived by D2-40 was a representational marker illustrating the trade and BVI had no significance whatsoever. Similarly, in order to support the use of D2- 40 stains as unambiguous markers in clinical settings, it is essential to have further arranged examinations with greater people.
Ethical Clearence
Nil.
Source of Funding
Self-funded.
Conflict of Interest
Nil.
References
- DeSantis CE, Bray F, Ferlay J, et al. International variation in female breast cancer incidence and mortality rates. Cancer Epidemiol Prevention Biomarkers 2015; 24:1495-1506.
- Kumar V, Abbas AK, Fausto N, et al. Robbins and Cotran pathologic basis of disease, professional edition e-book. Elsevier Health sciences 2014.
- Allred DC, Harvey JM, Berardo M, et al. Prognostic and predictive factors in breast cancer by immunohistochemical analysis. Modern Pathol 1998; 11:155-168.
- Robbins P, Pinder S, de Klerk N, et al. Histological grading of breast carcinomas: A study of interobserver agreement. Hum Pathol 1995; 26:873-879.
- Lakhtakia R. A brief history of breast cancer: Part I: Surgical domination reinvented. Sultan Qaboos University Med J 2014; 14:e166.
- Forman D, Ferlay J, Stewart BW, et al. The global and regional burden of cancer. World Cancer Report 2014; 2014:16-54.
- Cunnick GH, Jiang WG, Douglas-Jones T, et al. Lymphangiogenesis and lymph node metastasis in breast cancer. Molecular Cancer 2008; 7:23.
- Ito M, Moriya T, Ishida T, et al. Significance of pathological evaluation for lymphatic vessel invasion in invasive breast cancer. Breast Cancer 2007; 14:381-387.
- Valencak J, Heere-Ress E, Kopp T, et al. Selective immunohistochemical staining shows significant prognostic influence of lymphatic and blood vessels in patients with malignant melanoma. Eur J Cancer 2004; 40:358-364.
- Kuru B, Camlibel M, Gulcelik MA, et al. Prognostic factors affecting survival and disease-free survival in lymph node-negative breast carcinomas. J Surg Oncol 2003; 83:167-172.
- Donegan WL. Tumor-related prognostic factors for breast cancer. Cancer J Clin 1997; 47:28-51.
- Valencak J, Heere-Ress E, Kopp T, et al. Selective immunohistochemical staining shows significant prognostic influence of lymphatic and blood vessels in patients with malignant melanoma. Eur J Cancer 2004; 40:358-364.
- Braun M, Flucke U, Debald M, et al. Detection of lymphovascular invasion in early breast cancer by D2-40 (podoplanin): A clinically useful predictor for axillary lymph node metastases. Breast Cancer Res Treat 2008; 112:503-511.
- Wong JS, O’Neill A, Recht A, et al. The relationship between lymphatic vessell invasion, tumor size, and pathologic nodal status: Can we predict who can avoid a third field in the absence of axillary dissection? Int J Radiat Oncol Biol Phys 2000; 48:133-137.
- Engers R, Gabbert HE. Mechanisms of tumor metastasis: Cell biological aspects and clinical implications. J Cancer Res Clin Oncol 2000; 126:682-692.
Author Info
Department of Pathology, Sree Balaji Medical College and Hospital, Bharath Institute of Higher Education and Research, Chennai, IndiaCitation: Moumita Dam, Hemalatha Ganapathy, Comparison of Lympho-Vascular Invasion and Blood Vessel Invasion as a Prognostic Predictor in Carcinomas of the Breast, J Res Med Dent Sci, 2021, 9 (1): 328-332.
Received: 09-Dec-2020 Accepted: 04-Jan-2021
