Research - (2021) Volume 9, Issue 9
Comparison of Efficacy of Trypsin, Chymotrypsin and Bromelain with Dexamethasone and Serratiopeptidase in Postoperative Sequelae in Mandibular Third Molar Surgery-A Randomised Controlled Trial
Yandeti Srinivasulu*, Abdul Wahab and Dinesh Prabu
*Correspondence: Yandeti Srinivasulu, Department of Oral and Maxillofacial surgery, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences (SIMATS), Saveetha University Tamilnadu, India, Email:
Abstract
Aim: The aim of the study was assessing the efficacy of trypsin+chymotrypsin + bromelain with dexamethasone+serratiopeptidase tablets in postoperative wound healing in surgical removal of mandibular third molars impaction. Materials and Methods: A prospective randomized study conducted with 40 patients that required removal of mesio angularly impacted mandibular third molar. The systematic statistical analysis was performed after the data collection was done. Patients were categorized into two groups (Group 1: dexamethasone+serratiopeptidase , Group 2 : trypsin+chymotrypsin + bromelain ) in a crossover manner .Subjective and objective observations recorded that include age, gender, and pain score using visual analog scale . Each patient was evaluated using a visual analogue scale.trypsin+chymotrypsin + bromelain Results: Pain intensity at the postoperative 1st, 3rd, 5th, 7th day postoperative was less in dexamethasone+serratiopeptidase group than trypsin+chymotrypsin+bromelain group and there was significant difference seen statistically (p<0.001).Swelling and Trismus were not statistically significant, however there were significant reduction in Swelling and Trismus on 3rd day. Conclusion: No statistically significant difference was noted between two groups with respect to pain and swelling, however in case of trismus there was a statistically significant difference between the two groups. Clinically patients on dexamethasone had better relief with regards to pain, trismus and swelling when compared to the trypsin group. Use of Dexamethasone postoperatively following surgical removal of mandibular third molar provided better relief with regards to the above parameters.
Keywords
Anti-inflammatory, Trypsin, Chymotrypsin, Bromelain, Dexamethasone, Serratiopeptidase mandibular third molar
Introduction
Surgical removal of impacted third molars is one of the most common procedures performed by maxillofacial surgeons by elevating a flap which causes a significant amount of soft tissue injury releasing various chemical mediators of inflammation [1]. These mediators trigger physiological processes like vasodilatation, vasoconstriction, leukocyte migration, and chemotaxis. Inflammation kicks off the healing and regeneration process for wounded tissues. Even though inflammation is a healing process, it produces a great deal of discomfort owing to pain and swelling [2]. Trismus, which is caused by intramuscular inflammation, may be a source of anxiety for the patient. As a result, to reduce the negative effects of inflammation, it is necessary to control the inflammatory process [3].
Infections and dehiscence of the wound are common consequences following surgical operations, especially in hospitals with high patient volumes. As a result, better and faster wound healing is desirable to reduce inpatient duration. Wound healing is a continuum of complex interrelated biological processes at the molecular level [4]. During wound healing, the formation and remodeling of the extracellular matrix involves a series of events that occur in a highly sequential manner [5]. Following trauma to soft tissues or skeletal injury, fibrin exudates accumulate leading to edema, and hematoma thereby impair microcirculation. Plasmin, the body’s own fibrinolytic agent, breaks down the fibrin barrier and restores circulation, thereby facilitating the process of wound healing [6]. Proteolytic enzymes such as chymotrypsin and trypsin from the pancreas, bromelain (pineapple enzyme), papain (papaya enzyme), fungal proteases, and serratia peptidase (the ‘‘silkworm" enzyme) have all been shown to act in a similar manner. These enzymes are absorbed by circulating enzyme inhibitors, such as a1-antitrypsin and a2-macroglobulin, whose levels rise sharply in response to injury and tissue loss. This increase in inhibitor levels is what causes the operative fibrinolytic shutdown and the persistence of inflammatory edoema, which causes healing to be delayed. As a result, proteolytic enzymes aid the action of plasmin, which is required to clear up the blocked microcirculation and therefore resolve edoema and begin the healing process [7].
Study setting and data collection
A prospective randomized study conducted with 40 patients that required removal of mesio angularly impacted mandibular third molar. The systematic statistical analysis was performed after the data collection was done. Patients were categorized into two groups (Group1: dexamethasone+serratiopeptidase, Group 2: Trypsin+chymotrypsin+bromelain) in a crossover manner. Subjective and objective observations recorded that include age, gender, and pain score using visual analog scale . . Each patient was evaluated using a visual analogue scale.
Patients were reported to Saveetha Dental College for pain treatments. The patients were reported to the Department of Oral and Maxillofacial Surgery for surgical removal of third molar impaction .
Ethical committee approval for this study was obtained from the Institutional Ethics Committee with the following ethical approval number. SDC/SIHEC/2020/ DIASDATA/0619-0320.
Sampling
Patients who underwent pericoronitis treatment at Saveetha Dental College were included in the study population by Systematic Sampling.
Inclusion criteria
Patients of all age groups and gender with impacted mandibular third molars with diagnosis of pericoronitis were included.
Exclusion criteria
Patients with impacted teeth other than third molars,and common dental problems were excluded from the study.
Duplicate patient records and incomplete data were excluded. Datas were reviewed by an external reviewer. A total of 40 patients were enrolled in the study. The patient's age, gender, and pericoronitis, as well as pericoronal abscess, were all reported.
Data analysis
The data obtained were tabulated in Microsoft Excel 2016 (Microsoft office 10) and later exported to SPSS (Statistical Package for Social Sciences) for Windows version 20.0, SPSS Inc, Chicago IU, USA) and subjected to statistical analysis. The Chi-square test was used, with a significance level of< 0.05.
Results
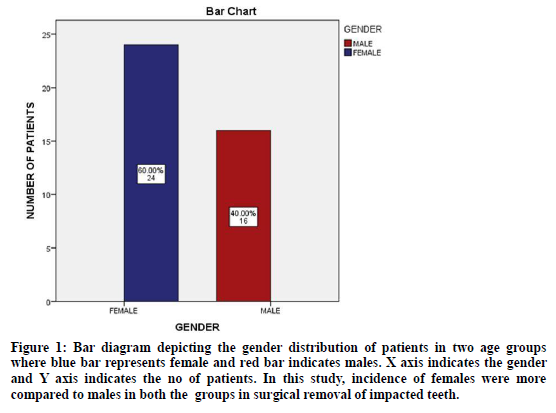
There were 26 female patients and 14 male patients, with an average age of 23 years. Statistical analysis was performed with the paired t-test and the independent ttest for comparison between the groups.
Comparison of post-operative swelling between Dexamethasone and Chymotrypsin groups with facial measurement values showed statistically significant less swelling with Dexamethasone group on 1st, 3rd, 5th post-operative days as compared to Chymotrypsin group. (Table 1). Patients taking Dexamethasone showed better mouth opening ability as compared against Chymotrypsin group patients on 1st, 3rd, 5th and 7th post-operative days. But none of the values compared, were statistically significant for mouth opening (Table 2). Comparison of post-operative pain between Dexamethasone and Chymotrypsin groups revealed a statistically significantly less pain with Dexamethasone group on 1st, 3rd, 5th, and 7th post-operative days compared to Chymotrypsin group (Table 3).
| Day | Group | Number of patients | Mean | Standard Deviation | P Value |
|---|---|---|---|---|---|
| 1st Day | Group 1 | 20 | 3.6 | 0.5 | <0.001 |
| Group 2 | 20 | 4.08 | 0.4 | ||
| 3rd Day | Group 1 | 20 | 5.48 | 0.51 | <0.001 |
| Group 2 | 20 | 6.2 | 0.5 | ||
| 5th Day | Group 1 | 20 | 3.2 | 0.707 | <0.001 |
| Group 2 | 20 | 4.8 | 0.408 | ||
| 7th Day | Group 1 | 20 | 1.4 | 0.645 | <0.001 |
| Group 2 | 20 | 1.44 | 0.507 |
Table 1: Swelling measurement.
| Day | Group | Number of patients | Mean | Standard deviation | P Value |
|---|---|---|---|---|---|
| 1st Day | Group 1 | 20 | -9.96 | 2.685 | <0.001 |
| Group 2 | 20 | -11.04 | 1.767 | ||
| 3rd Day | Group 1 | 20 | -7.6 | 2.125 | <0.001 |
| Group 2 | 20 | -8.92 | 1.654 | ||
| 5th Day | Group 1 | 20 | -5.82 | 1.624 | <0.001 |
| Group 2 | 20 | -5.74 | 1.234 | ||
| 7th Day | Group 1 | 20 | -3.04 | 1.107 | <0.001 |
| Group 2 | 20 | -3.56 | 1.051 |
Table 2: Maximal incisal mouth opening.
| Day | Group | Number of patients | Mean | Standard Deviation | P Value |
|---|---|---|---|---|---|
| 1st Day | Group 1 | 20 | 5.02 | 0.656 | <0.001 |
| Group 2 | 20 | 8.12 | 0.617 | ||
| 3rd Day | Group 1 | 20 | 2.14 | 0.435 | <0.001 |
| Group 2 | 20 | 4.56 | 0.551 | ||
| 5th Day | Group 1 | 20 | 1.02 | 0 | 0.001 |
| Group 2 | 20 | 1.4 | 0.5 | ||
| 7th Day | Group 1 | 20 | 0.5 | 0.5 | 0.001 |
| Group 2 | 20 | 1.01 | 0 |
Table 3: Pain measurement.
Data collected by means of the Visual Analogue Scale. The difference in postoperative pain scores between the groups was statistically significant at any of the time points studied although patients in Group 1 had a lower pain score at all time points. Data collected by means of the 0–4 Scale are Group 1 had a lower pain score at all time points. At 6 h after surgery, the difference between the groups was statistically significant. The comparison of mean pain scores at 1st day after surgery revealed a statistically significant difference between the groups, both according to VAS and by the 0–4 scale (Figure 1).
Figure 1: Bar diagram depicting the gender distribution of patients in two age groups where blue bar represents female and red bar indicates males. X axis indicates the gender and Y axis indicates the no of patients. In this study, incidence of females were more compared to males in both the groups in surgical removal of impacted teeth.
Discussion
An impacted third molar tooth can cause significant discomfort, swelling, and dysfunction if it is surgically removed. It is said that the inflammatory process is necessary for healing to occur but inflammation also causes edema, pain, and trismus [8,9]. Swelling usually reaches its maximum within 48-72 hours of the surgical procedure. The vasoactive amines cause vasodilatation, thereby increasing blood flow to the inflamed area. Even meticulous surgical technique can minimize the sequelae of inflammation but will not prevent it completely [2,10,11].
In several physiological processes, including tissue morphogenesis, tissue repair, angiogenesis, and tissue modulation, enzymes play a significant role in proteolytic modulation at the cellular matrix, reducing bruising, swelling, discomfort, and healing time. Oral enzyme therapy consists of enzymes that are taken orally, absorbed in the intestine, and function systemically. Endogenous enzymes that regulate immunological function, cell signalling, oxidative stress, and blood flow are supported and maintained by systemically absorbed enzymes [12].
They appear to minimise the body's physiological overshooting reaction to diseases and injuries, allowing the body to utilise its natural repair process more efficiently, swiftly repairing damaged structures [13]. Wound healing can be impaired by one or more phases of the inflammatory processes. Local impacts such as oxygenation, infection, foreign bodies, and venous insufficiencies affect the wound's characteristics directly, while systemic factors such as age, gender, hormones, stress, ischemia, nutrition, and metabolic disorders affect the body's ability to heal the wound [8,14].
Proteolytic enzyme preparations have been used since Mayan civilization, when wrapping papaya leaves around wounds was thought to help them heal faster. Pineapple has been used as a medicinal plant by several tropical native cultures and its enzyme bromelain has been chemically known since 1876 [15]. Following that, their use as an anti-inflammatory and anti-edematous agent became apparent. In addition to this, these enzymes also express fibrinolytic, immune normalizing, and primary and secondary analgesic effects [10,16]. When several clinical and experimental studies showed that oral administration of these systemically acting enzymes resulted in high bioavailability without a loss of functional activity, interest in these enzymes skyrocketed, and they were hailed as a promising treatment for acute (e.g., sports) injuries, post-surgery, and degenerative joint conditions [17–19].
On the first, third, fifth, and seventh postoperative days, we found that the dexamethasone group had statistically significantly less swelling than the chymotrypsin group. Similar results were found showing Dexamethasone has better anti-inflammatory effects [3,20]. Statistically significant less cheek swelling was noted with Dexamethasone group on 1st, 3rd, 5th, 7th postoperative days as compared to Chymotrypsin group [12]. In our study patients taking Dexamethasone showed better mouth opening ability as compared against Chymotrypsin group patients on 1st, 3rd, 5th and 7th post-operative days. Dexamethasone may function by blocking the release of arachidonic acid from membrane lipids (by promoting the development of proteins called Amnexins or Lipocortins that inhibit phospholipase A2), so indirectly lowering the generation of all eicosanoid PGs, TXs, and LTs. Furthermore, they prevent cytokines from inducing COX-2 at the site of inflammation. Eicosanoid modulation, fibrinolytic action, stimulation of endogenous proteases, and necrotic tissue clearance are all effects of chymotrypsin [8].
Conclusion
Wound treatment with trypsin and chymotrypsin provides a better resolution of symptoms of inflammation such as the improvement of erythema, local irritation, discharge, edema, induration, and tenderness. There was no statistically significant difference between the two groups in terms of discomfort and edoema, but there was a statistically significant difference in terms of trismus. Clinically patients on dexamethasone had better relief with regards to pain, trismus and swelling when compared to the trypsin group. Use of Dexamethasone postoperatively following surgical removal of mandibular third molar provided better relief with regards to the above parameters.
Conflict of Interest
No conflict of interest.
Funding for the Study
Nil.
References
- James R, Hupp DMDJM, Myron R, et al. Contemporary oral and maxillofacial surgery, 7E: South Asia Edition E-Book. Elsevier Health Sciences 2019; 740.
- Hargreaves KM, Troullos ES, Dionne RA, et al. Bradykinin is increased during acute and chronic inflammation: Therapeutic implications. Clin Pharmacol Ther 1988; 44:613–21.
- Elhag M, Coghlan K, Christmas P, et al. The anti-inflammatory effects of dexamethasone and therapeutic ultrasound in oral surgery. Br J Oral Maxillofac Surg 1985; 23:17–23.
- Marchegiani C, Lucci S. Tissue therapy: Clinical experiments in some surgical affections. Int J Tissue React 1982; 4:155–158.
- Grinnell F. Fibronectin and wound healing. J Cell Biochem 1984; 26:107–116.
- Latha B, Ramakrishnan KM, Jayaraman V, et al. Action of trypsin: Chymotrypsin (Chymoral forte DS) preparation on acute-phase proteins following burn injury in humans. Burns 1997; 23:3–7.
- Alexander CM, Werb Z. Proteinases and extracellular matrix remodeling. Curr Opin Cell Biol 1989; 1:974–82.
- Sisk AL, Hammer WB, Shelton DW, et al. Complications following removal of impacted third molars: The role of the experience of the surgeon. J Oral Maxillofac Surg 1986; 44:855–859.
- Juodzbalys G, Daugela P. Mandibular third molar impaction: Review of literature and a proposal of a classification. J Oral Maxillofac Res 2013; 4:e1.
- Malamed SF. Handbook of local anesthesia. Mosby 2004; 399.
- Peterson LJ. Peterson’s principles of oral and maxillofacial surgery. PMPH-USA 2012; 2000.
- Chopra D, Rehan HS, Mehra P, et al. A randomized, double-blind, placebo-controlled study comparing the efficacy and safety of paracetamol, serratiopeptidase, ibuprofen and betamethasone using the dental impaction pain model. Int J Oral Maxillofac Surg 2009; 38:350–355.
- Kerkhoffs GMMJ, Struijs PAA, de Wit C, et al. A double blind, randomised, parallel group study on the efficacy and safety of treating acute lateral ankle sprain with oral hydrolytic enzymes. Br J Sports Med 2004; 38:431–435.
- Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res 2010; 89:219–29.
- Taussig SJ, Batkin S. Bromelain, the enzyme complex of pineapple (Ananas comosus) and its clinical application. An update. J Ethnopharmacol 1988; 22:191–203.
- Gupta MK, Khanna JN, Khera SS. Evaluation of trypsin & chymotrypsin in the management of post-operative oedema. J Indian Dent Assoc 1985; 57:101–105.
- Bucci LR. Nutrition applied to injury rehabilitation and sports medicine. CRC Press 1994; 304.
- Al-Sandook TA, Tawfik NO, Qassim DA. Clinical evaluation of the efficacy of orthal-forte (prolytic enzymes, trypsin and chymotrypsin) on postoperative sequel following the removal of lower impacted third molar. Int J Enhanc Res Sci Technol Eng 2014; 3:169–73.
- Tamimi Z, Al Habashneh R, Hamad I, et al. Efficacy of serratiopeptidase after impacted third molar surgery: A randomized controlled clinical trial. BMC Oral Health 2021; 21:91.
- Weber CR, Griffin JM. Evaluation of dexamethasone for reducing postoperative edema and inflammatory response after orthognathic surgery. J Oral Maxillofac Surg 1994; 52:35–39.
Author Info
Yandeti Srinivasulu*, Abdul Wahab and Dinesh Prabu
Department of Oral and Maxillofacial surgery, Saveetha Dental College and Hospital, Saveetha Institute of Medical and Technical Sciences (SIMATS), Saveetha University Tamilnadu, Tamil Nadu, IndiaCitation: Yandeti Srinivasulu, Abdul Wahab, Dinesh Prabu, Comparison of Efficacy of Trypsin, Chymotrypsin and Bromelain with Dexamethasone and Serratiopeptidase in Postoperative Sequelae in Mandibular Third Molar Surgery-A Randomised Controlled Trial , J Res Med Dent Sci, 2021, 9(9): 140-144
Received: 10-Aug-2021 Accepted: 13-Sep-2021