Research - (2020) Volume 8, Issue 1
Comparison between Conventional Orthopantomograph and Three Dimensional Reconstructed OPG from Cone Beam Computed Tomography in Evaluation of Root Resorption during Orthodontic Treatment
Faisal Mohamed Faisal1* and Dheaa H Al-Groosh2
*Correspondence: Faisal Mohamed Faisal, Ministry of Orthodontics, College of Dentistry, University of Baghdad, Baghdad, Iraq, Email:
Abstract
Introduction: Radicular resorption is an unwanted side effect of orthodontic therapy.
Aim: The aim of this study was to compare between two radiographic methods in detection of root resorption induced by orthodontic treatment, by comparing panoramic radiographic images (OPG) with cone-beam computed tomography volumes (CBCT) in assessing radicular resorption encouraged by orthodontic treatments.
Methods: The sample of this study consisted of 469 teeth in 20 individuals after the completion of leveling and alignment phase of orthodontic therapy with fixed appliances. This study examined & tested the existence or nonexistence and the degree of radicular reabsorption on the OPG and the corresponding reconstructed 3D CBCT volumes. Radicular resorption was assessed as grade 0 (no resorption), grade 1 (mild resorption), grade 2 (moderate resorption), grade 3 (severe resorption) and grade 4 (extreme resorption).
Results: assessment of OPG radiographs showed that the evaluation of 12 teeth was not possible. There were statistically significant differences found between OPG and CBCT: 165 and 87 teeth revealed no radicular resorption by OPG and CBCT volumes, respectively; 237 and 292 teeth revealed mild root resorption, while 54 and 79 revealed moderate resorption by OPG and CBCT volumes, respectively. Furthermore, 3 teeth evaluated to have grade 3 radicular resorption (severe resorption) when evaluated by OPG, while 10 teeth were assessed to have severe resorption with CBCT.
Conclusion: Radicular resorption during and after orthodontic movement of teeth is underrated when assessed by OPG. CBCT may be a valuable complemental analytic technique to formal radiology, in order to be used when a choice on continuance or adjustment of the orthodontic therapy is needed due to root resorption induced by orthodontic treatment.
Keywords
CBCT, OPG, Orthodontic treatment, Panoramic radiographs, Dentistry
Introduction
Permanent demineralization of cementum (occasionally of dentine) of root surface of the tooth histologically can be defined as root resorption [1]. Diagnosis can be achieved by anamnestic data and thorough clinical reflexion, but only radiographic investigations are determinative, repeatedly exclusive, and regularly decisive. Factors lead to radicular reabsorption can be classified according to Alexander, et al. and Baumrind et al. in 1996 into local or general: Endocrine pathologies, significant oral dysfunctions, osteoporosis, traumas or external causes (orthodontic treatments), expanders, intrusion movements, aggressive or inappropriate orthodontic therapy, and therapy in patients with predisposition for root resorption (traumas, osteoporosis, or hypothyroidism) [2,3].
Different theories were created to explain mechanisms of root resorption: Becks, et al. in 1932 and Becks, et al. in 1936 wrote about “hereditary transmission of the individual predisposition for root resorption” [4,5]. Rygh, et al. in 1986 wrote about “predisposition not in different individuals only, but also in the same individual at dissimilar times, as hormone metabolical signals can change the osteoclastic/ osteoblastic activity” [6].
The individual`s age is essential: Root resorption induced by orthodontic treatment is mostly visible throughout adolescence after most of orthodontic treatments are completed and root apices are closed by this time. Sameshima, et al. stated that root reabsorption rises with age, particularly in the area of anterior teeth, corresponding to the incisor teeth [7]. Melsen, et al. declared that adult individuals don’t have similar cellular pool of young individuals thus, orthodontic forces directed to the teeth should be minimized, because the amount of bone to be resorbed relative to irregular movement of teeth is also minimized [8]. Most authors [9] found no relation between root resorption and gender, though Brezniak, et al. proclaimed that females were more susceptible to root resorption to the ratio of 3.7:1 [10,11].
Certain radiographic examinations can be effective documentation particularly for orthodontists who, more than other specialists are frequently under medical-legal authority regarding a contentious radicular reabsorption. The radiographic investigations are in fact an independent enduring record which in the medicallegal field can be assessed by numerous examiners, further independently than other particular clinical examinations [12,13]. Radiographic analysis can expose an abnormal pathology earlier than the appearance of clinical signs and symptoms, which is essential, particularly if unsuitable orthodontic treatments can be prevented, if it could have deteriorated the situations of the dentition and their roots.
Teeth are enormously radiopaque and radiologically well defined, due to their high density; So radiological methods including those taken inside (periapical radiographs) and outside (Orthopantomograph or OPG) the patient`s mouth, based on digital and traditional ways, can give valuable information to the specialist [3,14,15]. Also the CBCT has become an extremely essential method in examinations, analysis and diagnostics.
Traditional method
Extra-oral Orthopantomographic Pethod (OPG): It pictures extensive surfaces (13 × 18/18 × 24/24 × 30 cm) and it is created by an orthopantomograph in which the X-ray origin and the film box rotate at the same time whereas the patient stand still with patient`s chin on the suitable support [16]. It is beneficial as a primary diagnostic orientation and gives an overall idea of dentition, dental arches, bones of maxilla, sinuses adjacent to nasal cavity and Temporomandibular joint however, due to its imprecise definition and dental overlapping; it doesn’t deliver similar structural specifics gained by endo-oral radiology.
Intra-oral method (periapical radiograph): It pictures smaller surfaces (2 × 3/3 × 4/4 × 5/5 × 7 cm) and gives radiological information more precisely and dental alveoli details more accurately. A precise copy of the inspected structure couldn’t be achieved, since the copy is distorted by the ray angles which originated from one point but conical origin. In order to minimize distortions, the film should be placed in a parallel way and adjacent to the structure to impress, therefore the beam`s central ray can hit the structure and film in a perpendicular way.
Digital method: This technique can be used for intra-oral (endo-oral RX) and extra-oral (OPG) methods. Digital radiography gives an arithmetical value to the dissimilar levels of X-ray immersion in the tissues and to distinguish the numerous tones of gray which comprise the radiological picture.
Digital radiography can be classified into inline digital radiography, when the numerical picture can be acquired from the patient directly, and into outline digital radiography, when the numerical picture is acquired via a diagram that was made previously. The radiation dose decrease in digital radiography, the quality of images, and post-processing optimisation and elaboration are essential portions of development in radiographic dentistry. This study intent to confirm the validness of the radiological image and the most efficient radiographic procedures to analyze, avoid, treat, and decrease harm or resorption of root.
Materials and Methods
The study`s sample comprised of CBCT volumes, preoperative and postoperative OPG images for patients who were attending the orthodontic department at the College of Dentistry/University of Baghdad was recruited. 20 patients (5 males and 15 females) were selected, those patients have just finished the alignment phase with NiTi wire gauge of 0.017” X 0.025” or 0.018” X 0.025”, and planned to have a stainless steel wire in the following appointment.
The inclusion criteria for selected patients was [17]
1. Patients with full set of permanent teeth (with the acceptance of one missing or extracted tooth per each quadrant).
2. Patients have preoperative panoramic radiographs.
3. Patients have just finished the leveling and alignment phase of orthodontic treatment.
4. Patients with or have high risk of root resorption such as thin roots.
5. Patients have no root abnormalities or impactions rather than wisdom teeth.
6. Patients who need extraction for their wisdom teeth after completion of orthodontic treatment.
CBCT volumes and OPG radiographs were established in the 3D radiographic section of Ghazy AL-Hariri hospital using KAVO OP 3D Pro system machine (Finland), then the CBCT volumes were imported to On Demand 3D Dental software, while OPG images were imported to AutoCAD 2018- English software package for analysis. Preparation and position of the patients were achieved as stated by the operator guide of the KAVO OP 3D Pro system radiographic machine. The scanning protocol of CBCT was selected which included:
A. KV: 66.
B. mA: 10.
C. Scanning time: 16 sec.
D. Voxel size: 300.
The scanning protocol of OPG was selected which included
A. KV: 66.
B. mA: 7.4.
C. Scanning time: 16.4 second.
D. Voxel size: 87.
CBCT and OPG measurements
The existence or nonexistence and severity of radicular resorption in the reconstructed OPGs and the conventional OPGs is determined via the scoring system of Levander, et al. [18] that categorizes it into five grades as seen in Figure 1 and Figure 2.
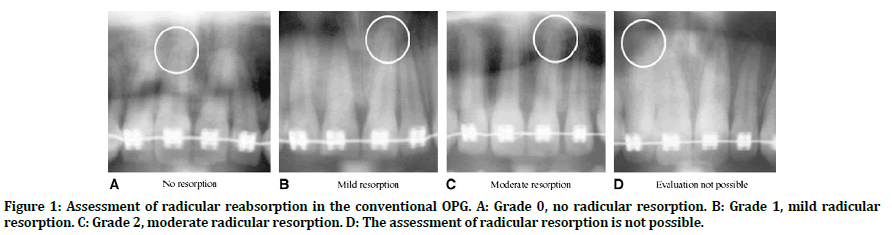
Figure 1. Assessment of radicular reabsorption in the conventional OPG. A: Grade 0, no radicular resorption. B: Grade 1, mild radicular resorption. C: Grade 2, moderate radicular resorption. D: The assessment of radicular resorption is not possible.
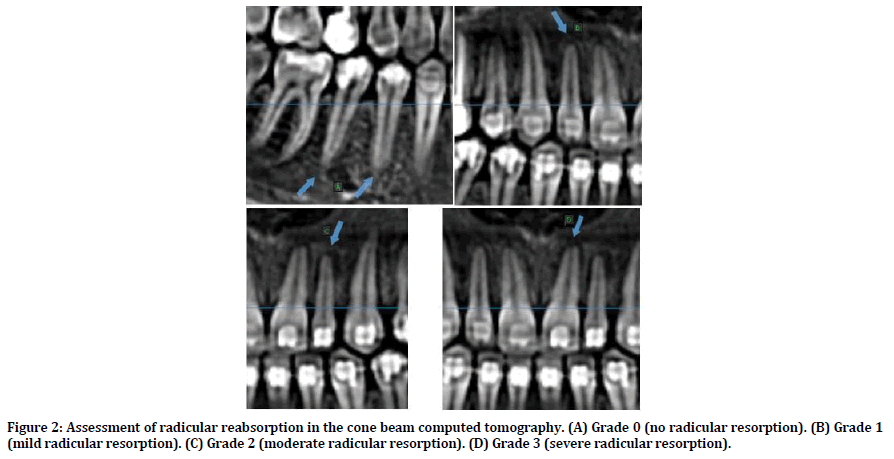
Figure 2. Assessment of radicular reabsorption in the cone beam computed tomography. (A) Grade 0 (no radicular resorption). (B) Grade 1 (mild radicular resorption). (C) Grade 2 (moderate radicular resorption). (D) Grade 3 (severe radicular resorption).
Grade 0: No root resorption.
Grade 1: Mild resorption, with the root of normal length and only an irregular contour.
Grade 2: Moderate resorption, with small areas of root loss and the apex having an almost straight contour.
Grade 3: Severe resorption, with loss of almost one third of root length.
Grade 4: Extreme resorption, with loss of more than one third of the root length.
A modification from scoring system of Levander, et al. [18] was created, this modification includes gathering the means of all teeth that were evaluated to have grade 0 (no resorption), and grade 1 (mild resorption) together as one category called least resorptive category, and also by gathering the means of all teeth that were evaluated to have grade 2 (moderate resorption) and grade 3 (severe resorption) as one category called most resorptive category, this can be achieved in both categories by the same way, for example: in least resorptive category a mean value for each tooth in the maxillary (or mandibular arch) in each method OPG (or CBCT) was obtained by summation of mean values for the tooth in the right and left side of maxillary (or mandibular) arch that was evaluated to have grade 0, then another mean value was obtained for each tooth that was evaluated to have grade 1 by the same way mentioned previously, at last a mean value was calculated from the extracted two mean values by the following equation:
Mean=(grade 0 mean+grade 1 mean)/2
This modification was created in order to simplify the understanding and comparison of the grades of radicular reabsorption by creating 2 categories: least resorptive category and most resorptive category.
Results
An overall of 469 dentitions were assessed by OPG and CBCT for radicular resorption: 235 teeth in the maxilla and 234 teeth in the mandible (157 incisors, 80 canines,152 premolars, and 80 molars). Assessment was not possible in 12 teeth including 1 incisor, 3 canines, and 8 premolars with the OPG method as these teeth were not clear enough to be evaluated properly. The comparability between both techniques was evaluated in dentitions evaluated by both techniques, 457 dentitions were evaluated for statistical analysis. The no. and percentages of dentitions with various grades of radicular reabsorption as assessed via OPG and CBCT are seen in Tables 1-4. According to these Tables; 165 dentitions were assessed by OPG showing grade 0 resorption (no resorption), while, with CBCT, just 87 dentitions showed grade 0 resorption (no resorption). 237 dentitions had grade 1 root resorption (mild radicular resorption) by OPG and 292 dentitions by CBCT. 54 teeth showed grade 2 root resorption (moderate root resorption) by OPG, however 79 dentitions showed grade 2 resorption by CBCT.
| Tooth No | Grades of Root Resorption N/% | P Value | ||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |||
| 1 | CBCT | 4/20% | 11/55% | 4/20% | 1/5% | 0.552 (NS) |
| OPG | 6/30% | 9/45% | 5/25% | 0 | ||
| 2 | CBCT | 0 | 14/70% | 6/30% | 0 | 0.402 (NS) |
| OPG | 1/5% | 15/75% | 4/20% | 0 | ||
| 3 | CBCT | 3/15% | 16/80% | 0 | 1/5% | 0.024 (NS) |
| OPG | 4/20% | 10/50% | 3/15% | 0 | ||
| 4 | CBCT | 1/5% | 7/35% | 10/50% | 0 | 0.230 (NS) |
| OPG | 4/20% | 7/35% | 5/25% | 0 | ||
| 5 | CBCT | 5/25% | 14/70% | 1/5% | 0 | 0.027 (NS) |
| OPG | 8/40% | 6/30% | 3/15% | 0 | ||
| 6 | CBCT | 1/5% | 12/60% | 4/20% | 3/15% | 0.019 (NS) |
| OPG | 7/35% | 11/55% | 2/10% | 0 | ||
Table 1: Grades of root resorption for maxillary right teeth.
| Tooth No | Grades of Root Resorption N/% | P Value | ||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |||
| 1 | CBCT | 1/5% | 13/65% | 5/25% | 1/5% | 0.110 (NS) |
| OPG | 6/30% | 10/50% | 2/10% | 2/10% | ||
| 2 | CBCT | 0 | 11/55% | 5/25% | 3/15% | 0.205 (NS) |
| OPG | 1/5% | 12/60% | 5/25% | 0 | ||
| 3 | CBCT | 2/10% | 15/75% | 3/15% | 0 | 0.889 (NS) |
| OPG | 3/15% | 14/70% | 3/15% | 0 | ||
| 4 | CBCT | 4/20% | 12/60% | 2/10% | 0 | 0.190 (NS) |
| OPG | 8/40% | 9/45% | 0 | 0 | ||
| 5 | CBCT | 5/25% | 14/70% | 1/5% | 0 | 0.008 (HS) |
| OPG | 14/70% | 4/20% | 1/5% | 0 | ||
| 6 | CBCT | 2/10% | 12/60% | 6/30% | 0 | 0.047 (S) |
| OPG | 8/40% | 10/50% | 2/10% | 0 | ||
Table 2: Grades of root resorption for maxillary left teeth.
| Tooth No | Grades of Root Resorption N/% | P Value | ||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |||
| 1 | CBCT | 1/5% | 16/80% | 3/15% | 0 | 0.045 (S) |
| OPG | 7/35% | 11/55% | 2/10% | 0 | ||
| 2 | CBCT | 1/5% | 15/75% | 4/20% | 0 | 0.042 (S) |
| OPG | 7/35% | 11/55% | 2/10% | 0 | ||
| 3 | CBCT | 3/15% | 15/75% | 2/10% | 0 | 0.915 (NS) |
| OPG | 4/20% | 14/70% | 2/10% | 0 | ||
| 4 | CBCT | 11/55% | 7/35% | 1/5% | 0 | 0.785 (NS) |
| OPG | 8/40% | 9/45% | 2/10% | 0 | ||
| 5 | CBCT | 8/40% | 11/55% | 1/5% | 0 | 0.948 (NS) |
| OPG | 9/45% | 10/50% | 1/5% | 0 | ||
| 6 | CBCT | 2/10% | 11/55% | 7/35% | 0 | 0.002 (HS) |
| OPG | 11/55% | 8/40% | 1/5% | 0 | ||
Table 3: Grades of root resorption for mandibular right teeth.
| Tooth No | Grades of Root Resorption N/% | P Value | ||||
|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | |||
| 1 | CBCT | 1/5% | 14/70% | 3/15% | 0 | 0.307 (NS) |
| OPG | 5/25% | 11/55% | 3/15% | 0 | ||
| 2 | CBCT | 4/20% | 13/65% | 3/15% | 0 | 0.855 (NS) |
| OPG | 5/25% | 13/65% | 3/15% | 0 | ||
| 3 | CBCT | 4/20% | 12/60% | `3/15% | 0 | 0.589 (NS) |
| OPG | 7/35% | 11/55% | 1/5% | 1/5% | ||
| 4 | CBCT | 10/50% | 8/40% | 0 | 1/5% | 0.522 (NS) |
| OPG | 8/40% | 10/50% | 1/5% | 0 | ||
| 5 | CBCT | 8/40% | 10/50% | 0 | 0 | 0.274 (NS) |
| OPG | 12/60% | 5/25% | 1/5% | 0 | ||
| 6 | CBCT | 6/30% | 9/45% | 5/25% | 0 | 0.074 (NS) |
| OPG | 12/60% | 7/35% | 1/5% | 0 | ||
Table 4: Grades of root resorption for mandibular left teeth.
Additionally, 3 dentitions showed grade 3 root resorption (severe resorption) when evaluated by OPG, while 10 teeth were assessed to have severe resorption by CBCT. In general, the differences between OPG imaged and CBCT volumes in assessing radicular resorption were significant for maxillary right and left first molars, maxillary right second premolars, maxillary right canines, mandibular right lateral incisors, and mandibular right central incisors. The differences between the 2 methods were highly significant for maxillary left second premolars, and mandibular right first molars. However, the differences between OPG and CBCT in evaluation of radicular resorption were not significant for maxillary right and left first premolars, maxillary right and left lateral incisors, maxillary right and left central incisors, maxillary left canines, mandibular right and left second premolars, mandibular right and left first premolars, mandibular right and left canines, mandibular left lateral incisors, mandibular left central incisors, and mandibular left first molars.
The following Figures 3 and 4 represent a modification from scoring system of Levander, et al. [18] this modification includes gathering the means of all teeth that were evaluated to have grade 0 (no resorption), and grade 1 (mild resorption) together as one category called least resorptive- category, and also by gathering the means of all teeth that were evaluated to have grade 2 (moderate resorption) and grade 3 (severe resorption) as one category called most resorptive category, this can be achieved in both categories by the same way, for example: in least resorptive category a mean value for each tooth in the maxillary (or mandibular arch) in each method OPG (or CBCT) was obtained by summation of mean values for the tooth in the right and left side of maxillary ( or mandibular) arch that was evaluated to have grade 0, then another mean value was obtained for each tooth that was evaluated to have grade 1 by the same way mentioned previously, at last a mean value was calculated from the extracted two mean values by the following equation:
Mean=(grade 0 mean + grade 1 mean)/2
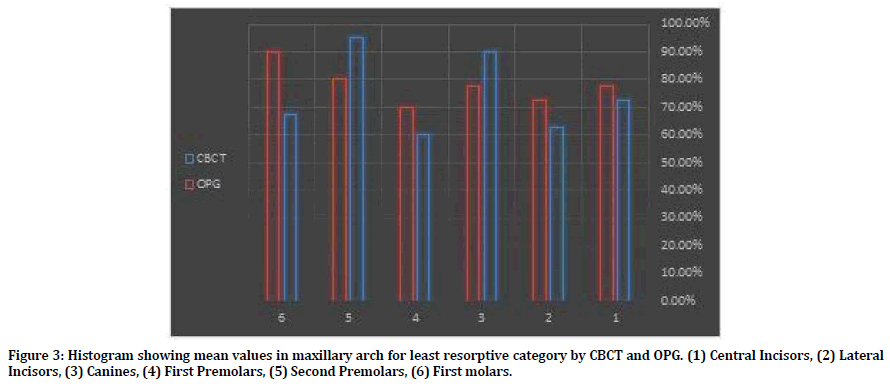
Figure 3. Histogram showing mean values in maxillary arch for least resorptive category by CBCT and OPG. (1) Central Incisors, (2) Lateral Incisors, (3) Canines, (4) First Premolars, (5) Second Premolars, (6) First molars.
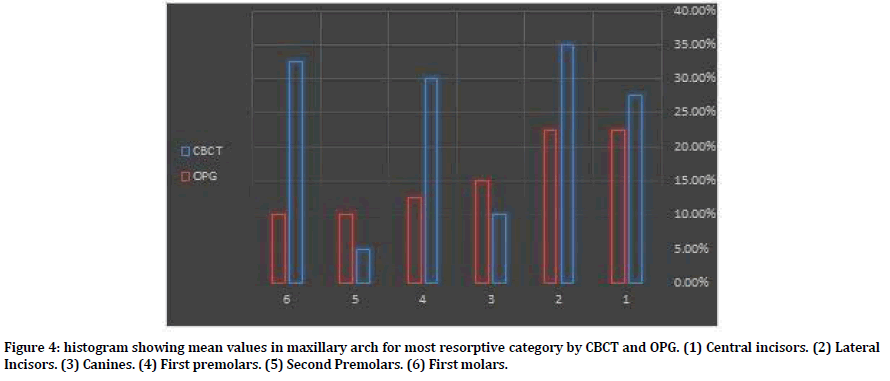
Figure 4. histogram showing mean values in maxillary arch for most resorptive category by CBCT and OPG. (1) Central incisors. (2) Lateral Incisors. (3) Canines. (4) First premolars. (5) Second Premolars. (6) First molars.
Discussion
A golden standard for the recognition of root resorption induced by orthodontic treatment remains unknown. Though, this was outside the aim of study. The aim of this study was to find out the accurateness of OPG in the diagnosis of radicular reabsorption in comparison with CBCT after finishing the leveling and alignment phase of orthodontic treatment.
A comparison of the OPG readings with those gained by CBCT: while 83.3% of dentition was identified to have radicular reabsorption with CBCT, just 64.3% exhibited radicular reabsorption by OPG. Additionally, the assessment of 12 dentitions was not possible with OPG. In general, the results recommended that radicular reabsorption may be underrated with OPG.
Radicular reabsorption is a three dimensional process, and its degree should be measured accurately. So far, radiological techniques, even though they have significant limitations, are the only techniques to assess radicular reabsorption. Nevertheless, careful interpretation and thorough understanding of the results are necessary.
Only scanning electron microscopy or histologic studies can provide precise results, on the other hand these studies are carried out on experimentally moved and then on extracted premolars[19, 20]. By using the OPG technique, mandibular incisors images proclined throughout the orthodontic therapy can be foreshortened or the radicular apices may lie exterior to the focal plane, hence leading to "shorter" dentition after orthodontic therapy [21]. Additionally, throughout orthodontic treatment, the incisors angles may change which may affect the length of the radiological image of the dentition; in consequence, the extent of radicular reabsorption is not assessed accurately [22]. Lastly, the absence of duplicability is also an essential factor which restricts the diagnostic precision of the OPG [23].
CBCT offers extremely detailed three dimensional imaging with single exposure of nearly eighteen seconds. CBCT imaging may be acquired at any angulation, consequently giving optimal views and excluding overlaps. Cone beam computed tomography volumes have delivered dependable information about radicular angulation [24] and the management of unerupted canines [25,26]. The investigative capability of cone beam computed tomography to identify imitated exterior radicular reabsorption was studied by Silveira, et al. [27].
Holes of various diameters and depths were created on the cervical, mid, and apical portions of the buccal surfaces. Assessment of the CBCT’s diagnostic capability revealed high sensitivity and exceptional precision; only tiny holes in the apical portion were harder to discover in comparison with the remaining holes. Currently, it is obvious that CBCT can’t substitute OPG that stills the main radiographic method. Nevertheless, in definite complicated situations, the three dimensional information collections may be more appropriate than ordinary radiological methods. In this way, if symptoms of moderate radicular resorption are noticeable by OPG through the beginning or mid stage of orthodontic therapy, cone beam computed tomography can be valuable in assessing the severity of the condition to aid making the choice on continuance and potential adjustment of orthodontic therapy. This study showed that, in comparison with OPG, CBCT has the upper hand in identifying radicular reabsorption during orthodontic therapy; on the other hand it has a bigger therapeutic hazard. Thus, cone beam computed tomography should be used for two chief causes: in research, it may raise the understanding of radicular reabsorption, and, in clinical field, cone beam computed tomography volumes might aid in monitoring individuals (with syndromes, agenesis, unusual root forms) at the hazard of development of severe radicular reabsorption throughout orthodontic treatment.
Conclusion
CBCT is a potent technique to display radicular reabsorption through orthodontic treatment, while OPG undervalues it. Cone beam computed tomography may be a valuable complementary diagnostic technique to ordinary radiology, which can be used in making the decision whether to carry on or adjust orthodontic treatment because of root resorption encouraged by orthodontic treatment.
References
- Bishara SE, Vonwald L, Jakobsen JR. Changes in root length from early to mid-adulthood: Resorption or apposition? Am J Orthod Dentofacial Orthop 1999; 115:563-568.
- Alexander SA. Levels of root resorption associated with continuous arch and sectional arch mechanics. Am J Orthod Dentofacial Orthop 1996; 110:321-324.
- Baumrind S, Korn EL, Boyd RL. Apical root resorption in orthodontically treated adults. Am J Orthod Dentofacial Orthop 1996; 110:311-320.
- Becks H, Marshall JS. Resorption or absorption? J Am Dent Assoc 1932; 19:1528-1537.
- Becks H. Root resorption and their relation to pathologic bone formation: Part I: Statistical data and roentgenographic aspect. Int J Orthodont Oral Surg 1936; 22:445-482.
- Rygh P, Bowling K, Hovlandsdal L, et al. Activation of the vascular system: A main mediator of periodontal fiber remodeling in orthodontic tooth movement. Am J Orthod 1986; 89:453-468.
- Sameshima GT, Sinclair PM. Predicting and preventing root resorption: Part I. Diagnostic factors. Am J Orthod Dentofacial Orthop 2001; 119:505-510.
- Melsen B, Agerbaek N, Eriksen J, et al. New attachment through periodontal treatment and orthodontic intrusion. Am J Orthod Dentofacial Orthop 1988; 94:104-116.
- Brudvik P, Rygh P. Transition and determinants of orthodontic root resorption: Repair sequence. Eur J Orthod 1995; 17:177-188.
- Mah J, Prasad N. Dentine phosphoproteins in gingival crevicular fluid during root resorption. Eur J Orthod 2004; 26:25-30.
- Brezniak N, Wasserstein A. Root resorption after orthodontic treatment: Part 2. Literature review. Am J Orthod Dentofacial Orthop 1993; 103:138-146.
- Rivera M, De Luca S, Aguilar L, et al. Measurement of open apices in tooth roots in Colombian children as a tool for human identification in asylum and criminal proceedings. J Forensic Leg Med 2017; 48:9-14.
- Cameriere R, Pacifici A, Pacifici L, et al. Age estimation in children by measurement of open apices in teeth with Bayesian calibration approach. Forensic Sci Int 2016; 258:50-54.
- Thomson B, Saklatvala J, Chambers Y. Osteoblasts mediate interleukin 1 stimulation of bone resorption by rat osteoclasts. J Exp Med 1986; 164:104-112.
- Tronstad L. Root resorption-a multidisciplinary problem in dentistry. Biological mechanisms of tooth eruption and root resorption 1988;293-301.
- Cattaneo PM, Dalstra M, Melsen B. The finite element method: A tool to study orthodontic tooth movement. J Dent Res 2005; 84:428-433.
- Abbas SA, Alhuwaizi AF. Buccal cortical bone thickness in iraqi arab adults by cone beam computed tomography for orthodontic mini-implants. Journal of Baghdad College Dent 2017; 29:183-187.
- Levander E, Malmgren O. Evaluation of the risk of root resorption during orthodontic treatment: A study of upper incisors. Eur J Orthod 1988; 10:30-38.
- Owman-Moll P, Kurol J, Lundgren D. Continuous versus interrupted continuous orthodontic force related to early tooth movement and root resorption. Angle Orthod 1995; 65:395-401.
- Kaur G, Sidhu MS, Grover S, et al. Evaluation of tooth surface characteristics after application of intrusive orthodontic forces using scanning electron microscope: An in vivo study. J Indian Orthod Society 2019; 53:27-37.
- Armstrong D. Root resorption after orthodontic treatment. Australian Orthod J 2006; 22:153-159.
- Schwartz JP, Raveli TB, Barnabe D, et al. Cone beam computed tomography study of apical root resorption induced by Herbst appliance. J Applied Oral Sci 2015; 23:479-485.
- Tammisalo T, Luostarinen T, Vähätalo K, et al. Comparison of periapical and detailed narrow-beam radiography for diagnosis of periapical bone lesions. Dentomaxillofac Radiol 1993; 22:183-187.
- Peck JL, Sameshima GT, Miller A, et al. Mesiodistal root angulation using panoramic and cone beam CT. Angle Orthod 2007; 77:206-213.
- Liu DG, Zhang WL, Zhang ZY, et al. Localization of impacted maxillary canines and observation of adjacent incisor resorption with cone-beam computed tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2008; 105:91-98.
- Walker L, Enciso R, Mah J. Three-dimensional localization of maxillary canines with cone-beam computed tomography. Am J Orthod Dentofacial Orthop 2005; 128:418-423.
- da Silveira HL, Silveira HE, Liedke GS, et al. Diagnostic ability of computed tomography to evaluate external root resorption in vitro. Dentomaxillofac Radiol 2007; 36:393-396.
Author Info
Faisal Mohamed Faisal1* and Dheaa H Al-Groosh2
1Ministry of Orthodontics, College of Dentistry, University of Baghdad, Baghdad, Iraq2Department of Orthodontics, Baghdad University, Iraq
Citation: Faisal Mohamed Faisal, Dheaa H Al-Groosh, Comparison between Conventional Orthopantomograph and Three Dimensional Reconstructed OPG from Cone Beam Computed Tomography in Evaluation of Root Resorption during Orthodontic Treatment, J Res Med Dent Sci, 2020, 8(1): 167-174.
Received: 16-Jan-2020 Accepted: 03-Feb-2020
