Original Article - (2019) Volume 7, Issue 2
Comparing the Effectiveness of the Unified Protocol Transdiagnostic and Mindfulness-based Stress Reduction Program on Anxiety and Depression in Infertile Women Receiving In Vitro Fertilisation
Elnaz Mousavi1, Sedighe Hosseini2, Maryam Bakhtiyari1, Abolfazl Mohammadi3, Mohesn Saberi Isfeedvajani4, Abbas Masjedi Arani1* and Seyed Hassan Sadaat5
*Correspondence: Abbas Masjedi Arani, Faculty of Medicine, Department of Clinical Psychology, Shahid Beheshti University of Medical Sciences, Iran, Email:
Abstract
Introduction: Our study aimed to preliminary evaluated outcomes on anxiety and depression symptoms among infertile women treated with unified protocol transdiagnostic (UP) in a group format and mindfulness-based stress reduction (MBSR).
Methods: A total of 45 subjects were randomly selected, of which 15 subjects were assigned to each of the experimental groups and 15 subjects in the control group. After referral by the reproductive endocrinologist, the subjects were evaluated by a clinical psychologist in terms of SCID structured; beck anxiety inventory and beck depression inventory-second edition then the subjects were randomly assigned into two groups.
Results: We found significant decline on general anxiety, and depression, while significant change over treatment in the UP and MBSR groups was observed as compared to control group. Our analysis revealed the larger effect sizes for changes in anxiety symptoms, followed by depressive. Furthermore, Treatment outcomes were demonstrated in UP and MBSR groups on general symptoms of anxiety, and depression after 3-months follow-up.
Conclusion: MBSR training declined mean anxiety and depression, and enhanced mindfulness, which can be applied as a useful approach for managing and decreasing anxiety and depression in infertile women receiving In vitro fertilisation (IVF).
Keywords
Anxiety and depression, Infertile women, Mindfulness-based stress reduction, Treatment
Introduction
Emotional disorders (depressive and anxiety disorders) are the most common psychiatric disorders worldwide [1], which lifetime prevalence for anxiety and depressive disorders have been estimated to be up to 29% and 19% [2,3].
The mentioned disorders with common comorbidity are often led to disability, functional impairment, occupational impairment, less productivity and high economic burden [3-8]. The consequences of emotional disorders highlight the crucial importance of psychological therapy for providing efficacious treatment for the condition. Therefore, mental health treatment programs (MHS) for these disorders should be applied more appropriately. Psychological therapies are considered based on the tow approach including disorder-specific (cognitive behavior therapy, CBT) and transdiagnostic when address symptoms of one disorder (i.e., depression), or symptoms of co-occurring condition by targeting common processes [3,9-13]. A variety of psychological interventions have been provided over the past decades, and their efficacies have been previously revealed [14-17].
Although effective therapeutic modalities are currently available for treatment of anxiety and depressive disorders by some approaches such as CBT, however most people do not have access to these features due a variety of barriers for dissemination and accessibility, e.g., costs, long distances, mobility restraints, privacy concerns, social stigma [18-20]. On the other hand, some draw backs are mentioned herein for disorder-specific treatment approach, i) a remarkable discrepancy of disorder-specific therapy with understanding of anxiety and depressive disorders has been highlighted; ii) a relatively limited attention has been regarded to comorbidity in disorder-specific treatments, whereas remarkable comorbidity rates (up to 40%–80%) have been documented in this regard [5,12,21].
The transdiagnostic approaches have been provided to solve the pitfalls of disorder-specific intervention via simultaneous addressing either principal and comorbidity by evaluating common symptoms, and overall course, as well as response to therapy, suggesting a promising therapy. The transdiagnostic approaches are capable of detecting processes for underpinning an integrated array of diagnosis such as, interpersonal, cognitive-behavioral, emotional, psychological processes, etc. [3,22-24]. Transdiagnostic treatment is potentially capable of targeting a variety of common risk factors that may be helpful in enhancing the efficacy of psychological prevention programs [25,26].
The Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders (UP) has been used via focusing on CBT protocol for targeting emotion regulation processes involved in progression of emotional disorders [27]. On the other hand, mindfulness-based programs are commonly applied in healthcare, and educational settings such as mindfulness-based stress reduction [28]. Beneficial effect of MBSR has been previously indicated for many outcomes e.g., stress, psychological disorders and dealing with the disease and pain (e.g. high blood pressure, AIDS, chronic pain, cancer, depressive and anxiety disorders and sleep disorders, etc.) [28-35]. Favorable efficacy of MBSR has been reported for stress reduction, while its moderate effectiveness has been previously indicated for anxiety and depression [30]. A growing body of evidence supports effectiveness of MBSR for anxiety disorders [36,37]. Therefore, the current study was aimed to compare the effectiveness of unified protocol transdiagnostic treatment in group format and mindfulness-based stress reduction program on anxiety and depression in infertile women receiving IVF.
Materials and Methods
Sample methods
Participants included 45 women with infertility at the age of 20-45 years who were referred to Tehran Taleghani hospital with symptoms of anxiety and depression in 2018.
Subjects were entered into treatment groups and control group via SCID Structured, Beck Anxiety Inventory and Beck Depression and convenience sampling. A total of 45 subjects were randomly selected, of which 15 subjects were assigned to each of the experimental groups and 15 subjects in the control group.
Inclusion criteria included 1) Spending at least one year of marriage and having a definite diagnosis of infertility, 2) Elementary and higher education, 3) Women aged 20-45 years, 4) No previous treatment history of IVF/ ICSI, 5) Participation agreement.
Exclusion criteria included 1) Having hormonal and genital diseases, 2) Having a separation and remarriage history, 3) Having adopted child, 4) History of acute psychiatric disorder, 5) Absence of more than two sessions of treatment in the experimental group, 6) History of receiving MBSR and UP.
Procedure and instruments
Questionnaires
Structured clinical interview for Axis I, DSM-IV, (SCIDI): A comprehensive standardized tool for assessing the underlying psychiatric disorder in I axis based on the definitions and criteria of DSM-IV.
Structured clinical interview for Axis II, DSM-IV (SCID-II): This tool is a semi-structured diagnostic interview.
Beck anxiety inventory (BAI): This questionnaire specifically evaluates the severity of symptoms of clinical anxiety.
Beck depression inventory (BDI-II): This questionnaire is one of the most recognized tests of depression that was developed by Beck's Psychiatrist (1961).
After referral by the reproductive endocrinologist, the subjects were evaluated by a clinical psychologist in terms of SCID structured, beck anxiety inventory and beck depression inventory-second edition then the subjects were randomly assigned into two groups of intervention based on the criteria of inclusion and exclusion criteria (UP group, and MBSR group) and control group.
After completing letter of commitment and diagnosis of the disease, beck anxiety inventory, beck depression inventory, difficulties in emotion regulation scale (DERS), the Intolerance of Uncertainty Scale-Short Form (IUS-12, and Short List of Coping Strategies.
It should be noted that individuals were matched according to age in all three groups. Patients present in UP group (15 patients) for 10 sessions per week (each session for 2 hours). In the MBSR group, patients (15 patients) received training for reduction of mindfulness-based stress for 8 sessions per week (each session for 2 hours).
In order to comply with the principles of professional ethics, the control group received effective treatment at the end of the study. Diagnostic evaluation tools were used and severity of each disorder in the patients was performed in four stages of pre-intervention, in the midst of intervention (sixth session), post-intervention, and 3 months’ follow-up. After the end of the treatment sessions, the information was analyzed using multivariate statistical methods.
Statistical analysis
To quantitatively describes or summarizes the data, descriptive statistics were first used. T-test was used to test the hypotheses Covariance, and two-way analysis of variance (ANOVA) was also used for independent groups. Furthermore, the Kolmogorov–Smirnov test was employed to assess the normal distribution in dependent variables and the Levene's Test for assessing the equality of variances. A significant level was p<0.05. All analyses were conducted using in SPSS version 25.0 for Windows (SPSS, Inc., Chicago, IL).
Results
The results show that the age classification of the UP and MBSR treatment groups is similar in age. 47% (25) were 34 and 53% were between 35 and 44 years old. In the control group, one-third of the subjects were 25 to 34 years of age, and two-thirds of them were 35 to 44 years of age.
Table 1 describes the main variables, by separating the groups and intervention stages. The findings were reported using mean and standard deviation (SD).
| Variable | Stage | Groups | ||
|---|---|---|---|---|
| UP | MBSR | Control | ||
| Anxiety | Pre-test | 29/13 ± 7/60 | 34/07 ± 5/90 | 32/93 ± 8/20 |
| Post-test | 20/33 ± 4/06 | 25/33 ± 5/51 | 35/60 ± 8/08 | |
| Follow up | 19/80 ± 3/82 | 24/47 ± 5/78 | 37/00 ± 10/45 | |
| Depression | Pre-test | 26/93 ± 6/78 | 27/60 ± 6/10 | 28/67 ± 6/55 |
| Post-test | 20/40 ± 6/41 | 24/07 ± 5/34 | 30/89 ± 7/38 | |
| Follow up | 20/20 ± 6/80 | 23/93 ± 4/27 | 31/80 ± 6/52 | |
Table 1: The main variables by separating the groups and the test steps
The test defaults were measured by repeated measurements. Finally, using repeated measures test as well as post-test and paired comparisons; the effect of interventions was investigated.
Examining the values of Skewness and kurtosis shows that the Skewness values of all variables are obtained in the range 2+ to 2 and the kurtosis values for all variables ranged from 2+ to 2. According to this statistic, distribution of all variables can be considered normal. Shapiro-Wilk test showed that the significance level for all variables is greater than 0.05 and the distribution of variables is normal.
As shown in Table 2. The effect of time factor on anxiety level is found to be significant (p<0.05 and F=25.19). This means that mean of anxiety has decreased significantly in different stages of pre-intervention, post-intervention and follow-up. The Eta-square (η2) was determined as 0.375. The interaction of time and group was also found to be significant (p<0.05), indicating a time-varying effect in different groups (UP, MBSR, and control).
| Impact source | Sum of squares | Degrees of freedom | Average squares | The amount of F | p-value | Effect size |
|---|---|---|---|---|---|---|
| Group | 3444/13 | 2 | 1722/07 | 30/73 | <0/001 | 0/600 |
| Time | 736/73 | 24-Jan | 592/13 | 25/19 | <0/001 | 0/375 |
| Group and Time | 1061/41 | Feb-49 | 426/55 | 18/14 | <0/001 | 0/464 |
Table 2: Analysis of variance with repeated measurements to compare the effects of time and group
The results show that the effect of the groups (interventions) on anxiety (p<0.05 and F=30.73). This means that the treatments performed on anxiety have been effective and intervention has caused a significant change in the mean of anxiety in post-test and follow-up. The effect size index was equal to 0. 600. Regarding the Table 2, it can be concluded that the level of anxiety has a significant change in two intervention groups.
Figure 1 depicts the linear graph of the mean of anxiety. Charts have been reported by groups, and show a decreasing trend of anxiety levels in the two treatment groups. The reduction in anxiety slope in the two groups is approximately equal. Scores in the control group exhibits a slight increase in the post-test and follow-up stages.
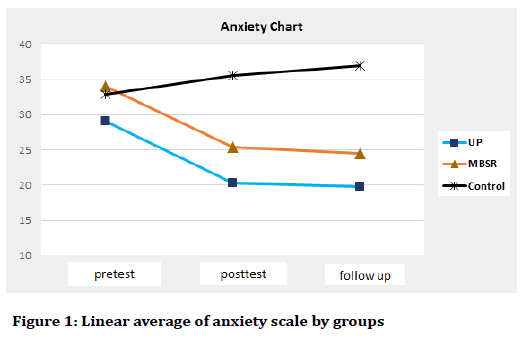
Figure 1. Linear average of anxiety scale by groups
In Table 3, the result of multivariate effects (group and time effects) on depression was measured. The variance analysis tests applied to evaluate whether the mean of depression in different stages (pre-test, post-test, and follow-up) was generally different or not. The findings presented herein, indicate that the effect of time factor on depression is significant (p<0.05 and F=18.83), indicating significant change of depression in different stages of pre-test, post-test and follow-up. The Eta-square (η2) was calculated as 0.310. In addition, the interaction of time and group was also found to be significant (p<0.05), indicating that time variation in various groups (UP, MBSR, and control) was different.
| Group | Comparison | Difference in averages | Standard error | p-value |
|---|---|---|---|---|
| UP | Pre-test with post-test | 8/80 | 1/55 | <0/001 |
| Pre-test with follow-up | 9/93 | 1/80 | <0/000 | |
| Post-test and follow-up | 0/533 | 0/486 | 0/292 | |
| MBSR | Pre-test with post-test testestest | 8/73 | 1/21 | <0/001 |
| Pre-test with follow-up | 9/60 | 1/19 | <0/001 | |
| Post-test and follow-up | 0/867 | 0/506 | 0/109 | |
| Control | Pre-test with post-test | -2/67 | 1/52 | 0/101 |
| Pre-test with follow-up | -4/07 | 2/30 | 0/098 | |
| Post-test and follow-up | -1/40 | 0/979 | 0/175 |
Table 3: Comparison of the mean of anxiety in different stages by groups
The effect of the group (interventions) on depression was found to be significantly considerable (p<0.05 and F=32.61). In fact, treatments have been effective in depression, which interventions have caused a significant change in the mean of depression in post-test and followup. The effect size was presented as 0.0614. According to the Table 4, it can be concluded that the degrees of depression in different stages had significant changes among at least two groups.
| Impact source | Sum of squares | Degrees of freedom | Average squares | The amount of F | p-value | Effect size |
|---|---|---|---|---|---|---|
| Group | 1433/03 | 2 | 716/51 | 32/61 | <0/001 | 0/614 |
| Time | 191/75 | 1/38 | 138/43 | 18/83 | <0/001 | 0/310 |
| Time and group | 455/94 | 2/77 | 164/58 | 22/39 | <0/001 | 0/516 |
Table 4: Analysis of variance with repeated measurements to compare time and group effects
Table 5 indicates the average results of interventions in different stages (pre-test, post-test and follow-up). The ttest was used to compare the different stages.
| Group | Comparison | Averages difference | Standard error | p-value |
|---|---|---|---|---|
| UP | Pre-test with post-test | 6/53 | 0/810 | <0/001 |
| Pre-test with follow-up | 6/73 | 0/973 | 0/001 | |
| Post-test and follow-up | 0/20 | 0/380 | 0/607 | |
| MBSR | Pre-test with post-test | 3/53 | 0/608 | <0/001 |
| Pre-test with follow-up | 3/67 | 0/882 | 0/001 | |
| Post-test and follow-up | 0/133 | 0/413 | 0/751 | |
| Control | Pre-test with post-test | -2/20 | 0/987 | 0/043 |
| Pre-test with follow-up | -3/13 | 1/276 | 0/028 | |
| Post-test and follow-up | -0/93 | 0/665 | 0/182 |
Table 5: Comparison of depression in different stages by groups
The results revealed a significant difference between intervention groups (UP group and the MBSR group) and the control group (p<0.05). In fact, the mean of depression in the treatment groups was reduced, but an increasing trend was found in control group. Additionally, in both treatment and control groups, there was a significant difference between pre-test and follow-up (p<0.05). Moreover, there was an increasing trend in the control group and a decreasing trend in the treatment groups. Furthermore, post-test and follow-up score was not found to be different in both treatment and control groups (p>0.05).
Figure 2 demonstrates the decreasing trend of depression in the two treatment groups. The decrease in depression is approximately equal in the two groups. Scores in the control group show a slight increase in the post-test and follow-up stages.
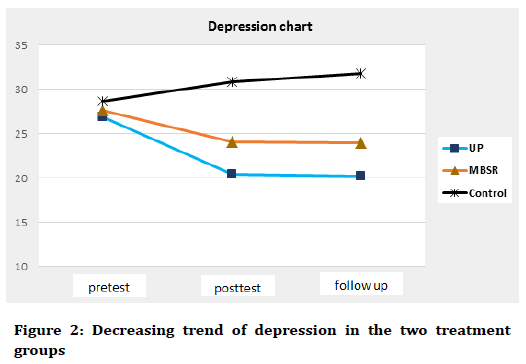
Figure 2. Decreasing trend of depression in the two treatment groups
Discussion
This current study was performed to evaluate the UP in a group format for subjects suffering from comorbid anxiety and depression symptoms among infertile women receiving IVF.
Our findings indicated significant decrease of depression and general anxiety symptoms in different stages of pretest, post-test and follow-up, whereas an increasing trend was found in control group. Treatment gains was observed at 3-month follow-up by UP in group setting on general symptoms of anxiety, depression and severity. These findings are more or less in agreement with previous studies in group settings [38,39].
The UP protocol in group format has been previously indicated to be useful with some advantages as compared to CBT. The UP is capable of facilitating the same therapeutic approach for many psychological disorders [38,40-42]. Furthermore, this protocol is capable of decreasing waiting lists by simultaneous addressing either therapeutic principles common to psychological treatments and comorbidity via evaluating common symptoms, and overall course, as well as response to therapy in anxiety and depressive disorders, which can potentially be useful in decreasing the duration of suffering in unattended subjects [24,42].
The efficacy of the UP has been previously evaluated [41,43]. Findings revealed UP was remarkably capable of decreasing symptom severity, negative affect, symptom interference, in anxiety disorders and/or depression comorbid state, but not all, where long-term effect has been reported to be up to 6 months post-intervention [44].
Previously, a preliminary intervention indicated the durability of broad intervention gains for the long-term outcome of UP [45].
A study by de-Ornelas et al. emphasized on efficacy of UP in group format, where this approach was capable of improving symptoms of depression and anxiety in patients suffering from unipolar depression and/ or comorbid anxiety disorders [46]. Laposa et al. reported a favorable decrease in general anxiety symptoms using UP protocol in Group format for comorbid anxiety symptoms, however further investigation of this intervention is warranted by researchers [39]. Bullis et al. demonstrated preliminary description of efficacy for UP in group format in patients with anxiety disorder and additional comorbid diagnoses, but its effectiveness for depression was found to be moderate [38].
However long-term duration of this intervention can be of great importance. Therefore, it cannot be guaranteed that that finding is the same with the results of UP protocols. On the other hand, variability in the types of anxiety symptoms should be taken in to consideration, because Up is not capable of addressing negative selfimage and focus of attention (FOA) as compared to cognitive-behavioral models of social anxiety disorder (SAD) [39].
It should be taken into account that it is very difficult to distinguish between specific treatments and transdiagnostic (e.g., UP, UP in group format). Further studies are required to compared the UP with cognitivebehavioural therapy (CBT) for clarifying effectiveness of the UP in patients with anxiety disorders; because it will show if it is equal to or better than CBT [39,47,48].
Our findings indicated that significant decreases were observed in depressive symptoms using MBSR protocol; MBSR training declined mean anxiety and depression, and enhanced mindfulness. But, there was no significant difference between the UP and the MBSR.
MBSR program has been revealed to be capable of decreasing symptoms of psychological disorders (e.g., anxiety and depression) [49-51].
As a matter of fact, MBSR programs has been reported to play its important role as effective protocol in improving psychological functions, resulting in reduction of suffering. MBSR programs have been shown to be effective on many physical and psychological complains such as anxiety symptoms, depression, stress systolic bold pressure [49,50,52]. MBSR program has been appeared to result in significantly greater decreases in stress, while its moderate effectiveness has been previously revealed for anxiety and depression [53]. Nevertheless, accumulating evidence suggests the effectiveness of MBSR for anxiety disorders [36,37]. The current results of MBSR's effectiveness are consistent with the previous studies [3,36,37] when patients improved their mindfulness. Therefore, MBSR may be considered as a useful approach for managing and decreasing anxiety and depression in infertile women. The findings presented herein appeared that MBSR program may be positively applicable for infertile women, when concerns are raised about anxiety and depression. Further studies are needed to clinically assess subjects representing the population of infertile women by MBSR program, where determination of efficacy is warranted. Limitations of our study were small sample size and short time follow-up (3 months followup). Therefore, revealing and depth understanding of predictors of long-term outcome are of crucial important in interoperating effectiveness of interventions, as studies reported predictors of short-term treatment outcomes (e.g., favorable effects at post-intervention).
Conclusion
The current study compared the changes in the UP group with changes in the MBSR and control groups.
The results reveal that anxiety and depression declined during the implementation of treatment by both UP and MBSR and continued to decrease during 3 month followup. Based on the findings, UP and MBSR were effectively capable of decreasing measures of depression, anxiety, when they were applied with infertile women. Our study suggests that mindfulness training may be associated with change in emotional processes and provide data on the efficacy of both interventions. It should be taken in to consideration that our findings have preliminary supported a clinically relevant effects of the UP and MBSR protocols.
Ethical Approval
This study was approved by Shahid Beheshti University of Medical Sciences Ethics Committee. The code of ethics issued by the ethics committee of Shahid Beheshti University of Medical Sciences was: IR.SBMU.MSP.REC. 96233.
Acknowledgments
All staff of Infertility Division of Taleghani hospital and patients who participated in this study is appreciated.
Conflict of Interest
The authors declare that there is no conflict of interest regarding the publication of this manuscript.
References
- Brown TA, Barlow DH. A proposal for a dimensional classification system based on the shared features of the DSM-IV anxiety and mood disorders: implications for assessment and treatment. Psychol Assess 2009; 21:256-71.
- Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 2005; 62:593-602.
- Khodyakov D, Zulfacar SM, Jones F, et al. Whole person care in under-resourced communities: Stakeholder Priorities at long-term follow-up in community partners in care. Ethn Dis 2018; 28:371-80.
- Goldberg DP, Krueger RF, Andrews G, et al. Emotional disorders: Cluster 4 of the proposed meta-structure for DSM-V and ICD-11. Psychol Med 2009; 39:2043-59.
- Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the national comorbidity survey replication. Arch Gen Psychiatry 2005; 62:617-27.
- Vos T, Barber RM, Bell B, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the global burden of disease study 2013. Lancet 2015; 386:743-800.
- Birnbaum HG, Kessler RC, Kelley D, et al. Greenberg employer burden of mild, moderate, and severe major depressive disorder: Mental health services utilization and costs, and work performance. Depress Anxiety 2010; 27:78-89.
- Mathers C, Fat DM, Boerma JT. The global burden of disease: 2004 Update. World Health Organization, Geneva 2008.
- Sauer-Zavala S, Barlow DH. The case for borderline personality disorder as an emotional disorder: Implications for treatment. Clin Psychol Sci Pract 2014; 21:118-38.
- Steele SJ, Farchione TJ, Cassiello-Robbins C, et al. Efficacy of the unified protocol for transdiagnostic treatment of comorbid psychopathology accompanying emotional disorders compared to treatments targeting single disorders. J Psychiatr Res 2018; 104:211-6.
- Kazdin AE. Evidence-based psychotherapies II: Changes in models of treatment and treatment delivery. S Afr J Psychol 2014; 45:3-21.
- Newby JM, McKinnon A, Kuyken W, et al. Systematic review and meta-analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clin Psychol Rev 2015; 40:91-110.
- Queen AH, Barlow DH, Ehrenreich-May J. The trajectories of adolescent anxiety and depressive symptoms over the course of a transdiagnostic treatment. J Anxiety Disord 2014; 28:511-21.
- Kennedy SM, Tonarely NA, Sherman JA, et al. Predictors of treatment outcome for the unified protocol for transdiagnostic treatment of emotional disorders in children (UP-C). J Anxiety Disord 2018; 57:66-75.
- Kennedy SM, Bilek EL, Ehrenreich-May J. A randomized controlled pilot trial of the Unified Protocol for the Treatment of Emotional Disorders in Children (UP-C). Behav Modif 2018:145445517753940.
- Cuijpers P, Sijbrandij M, Koole SL, et al. Adding psychotherapy to antidepressant medication in depression and anxiety disorders: A meta-analysis. World Psychiatry 2014; 13:56-67.
- Hofmann SG, Smits JAJ. Cognitive-behavioral therapy for adult anxiety disorders: A meta-analysis of randomized placebo-controlled trials. J Clin Psychiatry 2008; 69:621-32.
- WHO-AIMS WH. Mental health systems in selected low-and middle income countries: a WHO-AIMS Cross-national analysis. Geneva: World Health Organization 2009.
- Stjerneklar S, Hougaard E, Nielsen AD, et al. Internet-based cognitive behavioral therapy for adolescents with anxiety disorders: A feasibility study. Internet Interv 2018; 11:30-40.
- Collins KA, Westra HA, Dozois DJA, et al. Gaps in accessing treatment for anxiety and depression: Challenges for the delivery of care. Clin Psychol Rev 2004; 24:583-616.
- Brown TA, Campbell LA, Lehman CL, et al. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. J Abnorm Psychol 2001; 110:585-99.
- Wilamowska ZA, Thompson-Hollands J, Fairholme CP, et al. Barlow Conceptual background, development, and preliminary data from the unified protocol for transdiagnostic treatment of emotional disorders. Depress Anxiety 2010; 27:882-90.
- Mansell W, Harvey A, Watkins E, et al. Conceptual foundations of the transdiagnostic approach to CBT. J Cogn Psycho 2009; 23:6-19.
- Titov N, Dear BF, Staples LG, et al. Disorder-specific versus transdiagnostic and clinician-guided versus self-guided treatment for major depressive disorder and comorbid anxiety disorders: A randomized controlled trial. J Anxiety Disord 2015; 35:88-102.
- Titov N, Dear BF, Schwencke G, et al. Transdiagnostic internet treatment for anxiety and depression: A randomised controlled trial. Behav Res Ther 2011; 49:441-52.
- Weisel KK, Zarski AC, Berger T, et al. Efficacy and cost-effectiveness of guided and unguided internet- and mobile-based indicated transdiagnostic prevention of depression and anxiety (ICare Prevent): A three-armed randomized controlled trial in four European countries. Internet Interv 2018; 16:52-64.
- Mohajerin B, Bakhtiyar M, Olesnycky OS, et al. Application of a transdiagnostic treatment for emotional disorders to body dysmorphic disorder: A randomized controlled trial. J Affect Disord 2019; 245:637-44.
- Kabat-Zinn J. Bringing mindfulness to medicine: An interview with Jon Kabat-Zinn, PhD. Interview by Karolyn Gazella. Adv Mind Body Med 2005; 21:22-7.
- Gotink RA, Chu P, Busschbach JJ, et al. Standardized mindfulness-based interventions in healthcare: An overview of systematic reviews and meta-analyses of RCTs. PLoS One 2015; 10:e0124344.
- Khoury B, Lecomte T, Fortin G, et al. Mindfulness-based therapy: A comprehensive meta-analysis. Clin Psychol Rev 2013; 33:763-71.
- Baer R, Crane C, Miller E, et al. Doing no harm in mindfulness-based programs: Conceptual issues and empirical findings. Clin Psychol Rev 2019; 1-14.
- Rosenzweig S, Greeson JM, Reibel DK, et al. Mindfulness-based stress reduction for chronic pain conditions: Variation in treatment outcomes and role of home meditation practice. J Psychosom Res 2010; 68:29-36.
- Geary C, Rosenthal SL. Sustained impact of MBSR on stress, well-being, and daily spiritual experiences for 1 year in academic health care employees. J Altern Complement Med 2011; 17:939-44.
- Martin-Asuero A, Garcia-Banda G. The Mindfulness-based Stress Reduction program (MBSR) reduces stress-related psychological distress in healthcare professionals. Span J Psychol 2010; 13:897-905.
- Burschka JM, Keune PM, Oy UH, et al. Mindfulness-based interventions in multiple sclerosis: Beneficial effects of Tai Chi on balance, coordination, fatigue and depression. BMC Neurol 2014; 14:165.
- Vøllestad J, Nielsen MB, Nielsen GH. Mindfulness- and acceptance-based interventions for anxiety disorders: A systematic review and meta-analysis. Br J Clin Psychol 2012; 51:239-260.
- Regehr C, Glancy D, Pitts A. Interventions to reduce stress in university students: A review and meta-analysis. J Affect Disord 2013; 148:1-11.
- Bullis JR, Sauer-Zavala S, Bentley KH, et al. The unified protocol for transdiagnostic treatment of emotional disorders: Preliminary exploration of effectiveness for group delivery. Behav Modif 2015; 39:295-321.
- Laposa JM, Mancuso E, Abraham G, et al. Unified protocol transdiagnostic treatment in group format: A preliminary investigation with anxious individuals. Behav Modif 2017; 41: 253-68.
- Barlow DH, Farchione TJ, Fairholme CP, et al. The unified protocol for transdiagnostic treatment of emotional disorders: Therapist guide. New York: Oxford University Press 2011.
- Barlow DH, Ellard KK, Fairholme CP, et al. The unified protocol for transdiagnostic treatment of emotional disorders: Client workbook. New York, NY: Oxford University Press; 2011.
- Osma J, Suso-Ribera C, García-Palacios A, et al. Efficacy of the unified protocol for the treatment of emotional disorders in the Spanish public mental health system using a group format: Study protocol for a multicenter, randomized, non-inferiority controlled trial. Health Qual Life Outcomes 2018; 16:46.
- Ellard KK, Fairholme CP, Boisseau CL, et al. Unified protocol for the transdiagnostic treatment of emotional disorders: Protocol development and initial outcome data. Cogn Behav Pract 2010; 17:88-101.
- Farchione TJ, Fairholme CF, Ellard KK, et al. The unified protocol for the transdiagnostic treatment of emotional disorders: A randomized controlled trial. Behav Ther 2012; 43:666-78.
- Bullis JR, Fortune MR, Farchione TJ, et al. A preliminary investigation of the long-term outcome of the unified protocol for transdiagnostic treatment of emotional disorders. Compr Psychiatry 2014; 55:1920-7.
- de-Ornelas MAC, Soares-Filho G, Pereira V, et al. Psychiatric disorders and quality of life in patients with implantable cardioverter defibrillators: A systematic review. Prim Care Companion CNS Disord 2013; 15.
- Mohammadi A, Birashk B, Gharaie B. Comparison of the effect of group transdiagnostic therapy and group cognitive therapy on anxiety and depressive symptoms. Iran J Public Health 2013; 42:48-55.
- Clark DA, Taylor S. The transdiagnostic perspective on cognitive-behavioral therapy for anxiety and depression: New wine for old wineskins? J Cog Psychotherapy 2009; 23:60-6.
- Carlson LE, Garland SN. Impact of mindfulness-based stress reduction (MBSR) on sleep, mood, stress and fatigue symptoms in cancer outpatients. Int J Behav Med 2005; 12:278-85.
- Carter BS, Buckley D, Ferraro R, et al. Factors associated with reintegration to normal living after subarachnoid hemorrhage. Neurosurgery 2000; 46:1326-33.
- Katati MJ, Santiago-Ramajo S, Pérez-García M, et al. Description of quality of life and its predictors in patients with aneurysmal subarachnoid hemorrhage. Cerebrovasc Dis 2007; 24:66-73.
- Song Y, Lindquist R. Effects of mindfulness-based stress reduction on depression, anxiety, stress and mindfulness in Korean nursing students. Nurse Educ Today 2015; 35:86-90.
- Khoury B, Sharma M, Rush SE, et al. Mindfulness-based stress reduction for healthy individuals: A meta-analysis. J Psychosom Res 2015; 78:519-28.
Author Info
Elnaz Mousavi1, Sedighe Hosseini2, Maryam Bakhtiyari1, Abolfazl Mohammadi3, Mohesn Saberi Isfeedvajani4, Abbas Masjedi Arani1* and Seyed Hassan Sadaat5
1Faculty of Medicine, Department of Clinical Psychology, Shahid Beheshti University of Medical Sciences, Tehran, Iran2IVF Center, Taleghani Hospital, Shahid Beheshti University of Medical Sciences, Tehran, Iran
3Department of Psychiatry, Tehran, Iran
4Faculty of Medicine, Quran and Hadith Reasearch Center and Department of Community Medicine, Baqiyatallah University of Medical Sciences, Tehran, Iran
5Behavioral Sciences Research Center, Lifestyle Institute, Baqiyatallah University of Medical Sciences, Tehran, Iran
Citation: Elnaz Mousavi, Sedighe Hosseini, Maryam Bakhtiyari, Abolfazl Mohammadi, Mohesn Saberi Isfeedvajani, Abbas Masjedi Arani, Seyed Hassan Sadaat, Comparing the effectiveness of the unified protocol transdiagnostic and mindfulness-based stress reduction program on anxiety and depression in infertile women receiving in vitro fertilisation, J Res Med Dent Sci, 2019, 7(2): 44-51
Received: 08-Mar-2019 Accepted: 14-Mar-2019
