Research - (2021) Volume 9, Issue 4
Comparative High Resolution Computed Tomography and X-Ray Findings of Non-tuberculosis Lung Diseases and Pulmonary Tuberculosis in Patients with Acid Fast Bacilli Smear-Positive Sputum
Sharanya Ponni S and Prabakaran M*
*Correspondence: Prabakaran M, Department of Radio Diagnosis, Sree Balaji Medical College & Hospital, Bharath Institute of Higher Education and Research, India, Email:
Abstract
To compare the HRCT and X ray Chest imaging findings in tuberculosis and non-tuberculosis patients. To compare and contrast the imaging findings of tuberculosis and non-tuberculosis patients to assess the frequency and percentage of males and females involved. To identify the various imaging findings in eachstage of tuberculosis. The comparative study also helped in better visualisation of the pathologies with HRCT Chest.
Keywords
Tuberculosis, Communicable infections, Tomography
Introduction
Tuberculosis is one of the most common communicable infections encountered in India. It affects all ages and more towards the lower socioeconomic status. The presentation of the disease varies in each individual and age plays a role in certain types. As tuberculosis is a communicable disease, the bacterial load in each individual is responsible for the spread of the disease. The higher the bacterial load, more the chance of infection spread to the community. Tuberculosis has various presentations [1]. They are divided into subgroups based on their presentation and the onset of disease. The younger the individual, earlier the presentation of the disease[2].
Isolation of a high bacterial load patient is essential to prevent the bacterial spread. To prevent further deterioration of the patient’s symptoms, the anti-tuberculosis regimen is essential. Recently the resistance of antituberculosis drugs has increased the importance of treatment regimen. [3] In Radiology, the first modality to visualize a tuberculosiscaseis by X-ray technique. Chest postero-anterior views are taken, followed by High resolution computed tomography (HRCT) in required cases [4-6]. Though X ray is a primary modality, HRCT chest is considered superior in imaging techniques. X ray Chest can be used to initially asses and thereby very useful in follow ups after treatment as the risk of radiation is minimal compared to that of a CT scan. However HRCT technique is compared to be superior in the imaging of lung disease. [7] HRCT chest is performed using thin section CT images with a high spatial frequency reconstruction algorithm to detect and characterize to image the pulmonary diseases. With the availability of multidectector CT scanners, the scans are performed in a single breath hold. Two methods are used to assess, one axial HRCT images and volumetric reconstruction. These techniques provides better evaluation of cases[8,9]. A comparative study of the sputum positive tuberculosis and non-tuberculosis patients was done using HRCT chest and X ray imaging.
Methodology
Source of data
This is a comparative study done on a minimum of 50 patients with sputum positive tuberculosis and other chest symptoms who presented to the Department of Radio Diagnosis at Sree Balaji Medical College & Hospital. The study period was from December 2017– June 2019.
Methods of collection of data
✓ Duration of study: 19 months (December 2017 – June 2019)
✓ Sample size: 50 cases
✓ Inclusion criteria: All patients with sputum positive tuberculosis and chest symptoms who presented to the radiology department.
✓ Exclusion criteria: Asymptomatic individuals; pregnant women.
✓ Methods: All patients were subjected to X ray Chest and HRCT Chest.
Imaging protocols and procedure
Patients of the inclusion criteria who came to radiology department and referrals from pulmonology department who were subjected to X ray Chest and HRCT chest done using Siemens healthiness 16 slice scanner.
Scanning parameters
Patient preparation: Patient was briefed about the procedure and made to change the dress but to avoid clothing with metal such as zipper, snaps or jewellery, since metal objects may affect the CT images.
The HRCT protocol: The patient had to lieon the test table in a supine position with his arms raised over his head. Further scans with a patient in the prone position are obtained in a few situations, mostly high-resolution CT protocols of the lungs. To minimize artifacts produced by respiratory flexibility, the shortest possible scan time was used. In order to prevent misregistration caused by irregular patient breathing between scans, chest scans are obtained wherever possible to ones’ breath hold.
Technical protocol is as follows
✓ Slice thickness: 0.625-1.25 mm.
✓ Scan time: 0.5-1 second.
✓ kV: 120.
✓ mAs: 100-200.
✓ Collimation: 1.5-3 mm.
✓ Matrix size: 768 x 768/the largest available.
✓ FOV: 35 cm.
✓ Reconstruction algorithm: high spatial frequency.
Window: lung window.
Data collection: The data was collected by data collection sheet which was designed to include all variables (demography, HRCT findings and X ray findings). X Ray Chest was taken by CR (Computed Radiography) machine. Chest PA (postero-anterior views) were taken.
Protocol
✓ Exposure: 100-110 Kvp.
✓ Exposure: 4-8 mAs.
✓ Suspended inspiration.
Centring point at Thoracic 7th vertebra.
Research hypothesis
Compare the non-tuberculosis patients with tuberculosis sputum positive cases with the help of HRCT chest and Chest X ray, proving that TB is better delineated with HRCT Chest, though the chest X-ray is an initial investigation. Though subtle findings between TB and non TB are identified, TB manifests in 3 major forms, primary TB, post primary TB and Latent TB, where the findings are unique in each manifestation.
Data analysis
Comparative study.
Results
Results are explained in detail in form of tables (Tables 1-8) and Figures (Figures 1-6).
| Frequency | Percent | Valid Percent | Cumulative Percent | ||
|---|---|---|---|---|---|
| Valid | Female | 21 | 42 | 42 | 42 |
| Male | 29 | 58 | 58 | 100 | |
| Total | 50 | 100 | 100 |
Table 1: Frequency and percentage of people with TB andNon TB: SEX.
| Frequency | Percent | Valid Percent | Cumulative Percent | ||
|---|---|---|---|---|---|
| Valid | No TB | 25 | 50 | 50 | 50 |
| TB | 25 | 50 | 50 | 100 | |
| Total | 50 | 100 | 100 |
Table 2: Frequency and percentage of people with TBandNon TB non-valid.
| Frequency | Percent | Valid Percent | Cumulative Percent | ||
|---|---|---|---|---|---|
| Valid | No | 25 | 50 | 50 | 50 |
| Yes | 25 | 50 | 50 | 100 | |
| Total | 50 | 100 | 100 |
Table 3: Frequency and percentage of people with sputum AFP.
| Frequency | Percent | Valid Percent | Cumulative Percent | ||
|---|---|---|---|---|---|
| Valid | No | 35 | 70 | 70 | 70 |
| Yes | 15 | 30 | 30 | 100 | |
| Total | 50 | 100 | 100 |
Table 4: Frequency and percentage of people with cavity.
| Frequency | Percent | Valid Percent | Cumulative Percent | |
|---|---|---|---|---|
| Valid no | 50 | 100 | 100 | 100 |
Table 5: Frequency and percentage of people with ghon focus.
| Frequency | Percent | Valid Percent | Cumulative Percent | ||
|---|---|---|---|---|---|
| Valid | no nodule | 27 | 54 | 54 | 54 |
| solid calcified | 3 | 6 | 6 | 60 | |
| Partly solid | 4 | 8 | 8 | 68 | |
| ground glass | 16 | 32 | 32 | 100 | |
| Total | 50 | 100 | 100 | ||
Table 6: Frequency and percentage of people with Nmorp.
| Frequency | Percent | Valid Percent | Cumulative Percent | ||
|---|---|---|---|---|---|
| Valid | No | 46 | 92 | 92 | 92 |
| Yes | 4 | 8 | 8 | 100 | |
| Total | 50 | 100 | 100 | ||
Table 7: Frequency and percentage of people with mediastinal shift.
| Sex | Frequency | Percent | Valid Percent | Cumulative Percent | ||
|---|---|---|---|---|---|---|
| Female | Valid | No | 13 | 61.9 | 61.9 | 61.9 |
| Yes | 8 | 38.1 | 38.1 | 100 | ||
| Total | 21 | 100 | 100 | |||
| Male | Valid | No | 12 | 41.4 | 41.4 | 41.4 |
| Yes | 17 | 58.6 | 58.6 | 100 | ||
| Total | 29 | 100 | 100 |
Table 8: Frequency and percentage of people with ATT.
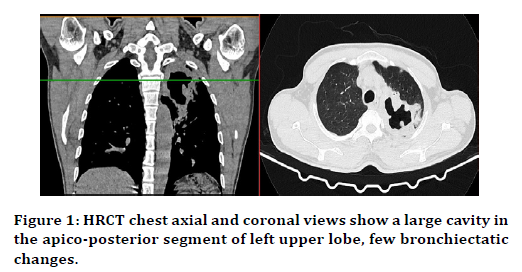
Figure 1. HRCT chest axial and coronal views show a large cavity in the apico-posterior segment of left upper lobe, few bronchiectatic changes.
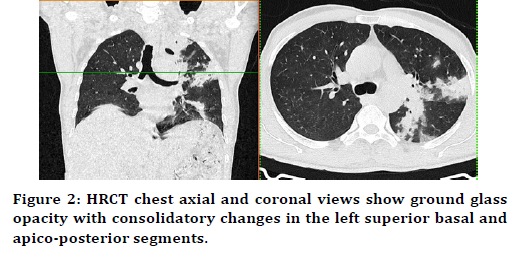
Figure 2. HRCT chest axial and coronal views show ground glass opacity with consolidatory changes in the left superior basal and apico-posterior segments.
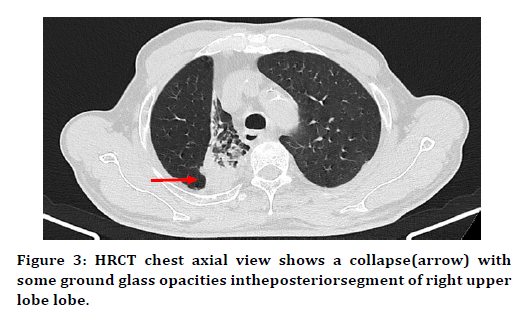
Figure 3. HRCT chest axial view shows a collapse(arrow) with some ground glass opacities intheposteriorsegment of right upper lobe lobe.
Figure 4. Pleural thicknong.
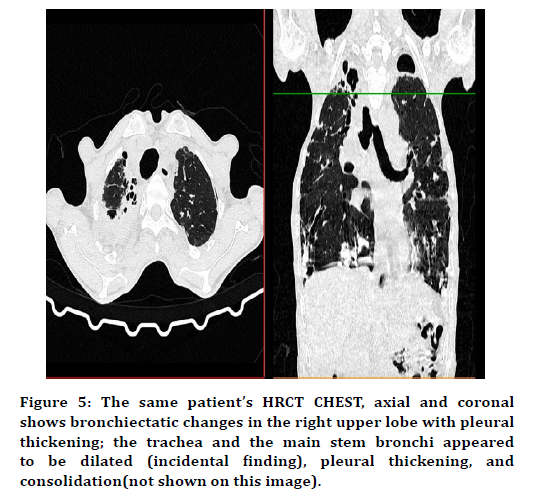
Figure 5. The same patient’s HRCT CHEST, axial and coronal shows bronchiectatic changes in the right upper lobe with pleural thickening; the trachea and the main stem bronchi appeared to be dilated (incidental finding), pleural thickening, and consolidation(not shown on this image).
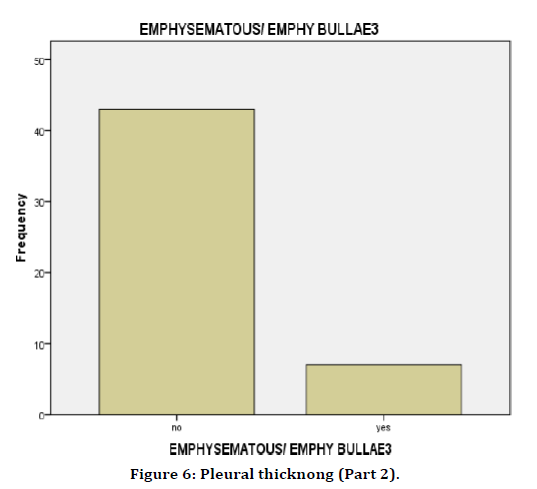
Figure 6. Pleural thicknong (Part 2).
Discussion
There have been human remains with TB traces dating back thousands of years. In recent decades, a concerted international effort to eradicate mycobacterium tuberculosis has been made to reduce the survival potential of the human pathogen with no existing reservoir for the ecosystem. This has been particularly successful since 2000, when the World Health Organization (WHO 2017) estimates that global incidence of tuberculosis has dropped by 1.5% each year. In addition, death from tuberculosis has been dramatically and steadily reduced. The WHO has reported that the global TB mortality rate has fallen by 22% from 2000 to 2015[10].
NTM-LD and pulmonary tuberculosis (PTB) have major medical complications if not diagnosed and treated at the earliest. This research aimed at contrasting and classifying the characteristics of chest CT that help distinguish NTM lung disease from PTB in patients with acid fast bacillus smear-positive (AFB) sputum [11-13]. All sputum positives for tuberculosis cases were included in the study and they underwent routine Chest X ray followed by HRCT chest [14]. In relation to the age, males between the ages 60 – 70 had higher correlation to the disease and females between the ages 50 to 70 had higher correlation to the disease. According to the study done there is significant association between collapse 38%ofstudy,(P 0.041, p value=<0.05), cavity 30% (P 0.001, p value<0.05), morphology of the nodules(ground glass and partly solid, 30% and 10%) (P 0.023, p value < 0.05) and nodule distribution (random and tree in bud, 18% and 30%) (P 0.037, p value<0.05) in primary TB [15-17].
In post primary TB, the patients had the treatment for tuberculosis once prior to the second episode of TB. The distribution of the nodules were statistically significant (P 0.037, p value < 0.05), implying that the nodules of certain distribution, centrilobular tree in bud 30%, random pulmonary nodules 16%, have an association with TB. Similarly, the morphology being ground glass 30% showed correlation with TB (P 0.023, p value < 0.05) [18].
Latent TB has a significant association with the pattern of nodule distribution, random nodules- 16% being predominant (P 0.037, p value < 0.05). In accordance to the male vs female statistics, there are 29 males and 21 females in this study. A total of 61.9% were affected of tuberculosis and 38.1% had other lung pathologies [19]. There were 58.6% of total males who were affected by TB and 41.4% who had other lung pathologies. There was no statistical significance and correlation between the individual disease/ pathology and the sex of the patient. However, females had more predilection to tuberculosis than male patients (61.9% vs. 58.6%). The X-ray Chest imaging showed similar statistics [20]. On comparing HRCT and X-ray, though HRCT Chestis a higher imaging modality, X ray chest is the first modality to visualize the significant imaging features. However certain imaging findings are better visualised in HRCT chest -segmental collapse, nodules in different size, morphology and distribution, fibro nodules, cavities, ground glass pattern, etc. The non-tuberculosis patients had higher incidence of consolidations and fewer random pulmonary nodules compared to the patients with typical tuberculosis imaging findings.
Conclusion
The patients with positive AFB smears and other lung pathologies had overlap of the clinical characteristics though certain imaging features pertaining to each stage of presentation in tuberculosis aided in the imaging of PTB and differentiating it from other lung pathologies. The comparative study also helped in better visualization of the pathologies with HRCT Chest.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgments
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- http://www.sprawls.org/resources/
- Engeler C. Christensen's physics of diagnostic radiology. 4th Edn. 1991; 180.
- Huda W. Review of radiologic physics. 4th Edn Philadelphia: Lippincott Williams.
- https://aapm.onlinelibrary.wiley.com/doi/full/10.1002/mp.13473
- Goldman LW. Principles of CT: Multislice CT. J Nucl Med Technol 2008; 36:57–68.
- Saunders J, Ohlerth S. CT Physics and instrumentation: Mechanical Design. In: Vet Comput Tomogr 2013; 1–8.
- Bushberg JT, Seibert JA, Leidholdt EM, et al. The essential physics of medical imaging. Schittny JC. Development of the lung. Cell Tissue Res 2017; 367:427–444.
- Hegazi AS. Evaluation of the lung diseases among smokers using conventional chest x- ray computerized tomography. Sudan University of Science and Technology, College of Graduate Studies and Scientific Research 2011.
- Schoepf UJ. Multi detector row CT of the Thorax. Springer 1984.
- Schwarz MI, King TE. Interstitial lung disease. Interstitial Lung Dis 2011; 106.
- Schittny JC. Development of the lung. Cell Tissue Res 2017; 367:427–444.
- https://www.ncbi.nlm.nih.gov/books/NBK470197/
- Leslie KO, Wick MR. Practical pulmonary pathology: A diagnostic approach. 3rd Edn 2018.
- Nakajima Y. Quick dissection of the segmental bronchi. Anat Sci Educ 2010; 213-215.
- https://www.ncbi.nlm.nih.gov/books/NBK441916/
- Sandhu GK. Tuberculosis: Current situation, challenges and overview of its control programs in India. J Glob Infect Dis 2011; 3:143–150.
- Prasad H, Singhal A, Mishra A, et al. Bovine tuberculosis in India: Potential basis for zoonosis. Tuberculosis 2005; 85:421–428.
- Srivastava K, Chauhan DS, Gupta P, et al. Isolation of Mycobacterium bovis and M. Tuberculosis from cattle of some farms in north India-possible relevance in human health. Indian J Med Res 2008; 128:26–31.
- https://www.ncbi.nlm.nih.gov/books/NBK513246/
- Nachiappan AC, Rahbar K, Shi X, et al. Pulmonary tuberculosis: Role of radiology in diagnosis and management. Radiographics 2017; 37:52-72.
Author Info
Sharanya Ponni S and Prabakaran M*
Department of Radio Diagnosis, Sree Balaji Medical College & Hospital, Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: Sharanya Ponni S, Prabakaran M, CT Comparative High Resolution Computed Tomography and X-Ray Findings of Non-tuberculosis Lung Diseases and Pulmonary Tuberculosis in Patients with Acid Fast Bacilli Smear-Positive Sputum, J Res Med Dent Sci, 2021, 9 (4): 343-347.
Received: 20-Mar-2021 Accepted: 08-Apr-2021
