Review - (2021) Volume 9, Issue 2
Comparative Evaluation of Incidence of Alveolar Osteitis with Bayonet Flap and Envelope Flap in Third Molar Surgery: A Systematic Review
Ramvihari Thota, Senthilnathan Periasamy* and Mahathi N
*Correspondence: Senthilnathan Periasamy, Department of Oral and Maxillofacial Surgery, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, India, Email:
Abstract
The purpose of this study was to compare two traditionally used surgical techniques to determine if a specific incision/flap design technique can predictably reduce the incidence of complications, particularly AO, in impacted mandibular third molar removal surgery. The aim of this systematic review is to assess the efficacy of Bayonet flap with Envelope flap on the Incidence of Alveolar Osteitis in impacted mandibular third molar surgery. The Databases of PubMed, Cochrane and Google Scholar were searched for the related topics along with a complimentary manual search of all oral surgery journals till December 2019. Articles were selected based on the inclusion criteria, which included all RCTs. Based on the study findings; the modified triangular flap may be superior to the envelope flap in terms of incidence in alveolar osteitis. The modified triangular flap design appears more advantageous than the envelope flap in terms of pain, trismus, and wound dehiscence in the first 3 days following surgical removal of impacted third molar and may have a better impact on QOL during this time. This may also indicate the clinical validity in terms of its ability to differentiate between the two flap groups and the excellent compatibility exhibited with clinically determined alveolar osteitis. Further comparative further studies involving larger populations are still required to determine the best flap technique for third molar surgery.
Keywords
Alveolar osteitis, Bayonet flap, Envelope flap, Molar surgery
Introduction
Surgical removal of impacted third molars is a common procedure in oral and maxillofacial surgery [1-4]. Since the third molar region contains loose connective tissue largely consisting of blood and lymph vessels [5,6], inflammatory complications such as pain, swelling, trismus, and alveolitis are generally seen in the immediate post‐operative period [5-8]. There are medical, legal, and economic implications of postoperative complications. These complications are still regarded as a major problem for both surgeons and patients [9]. Various surgical approaches have been employed and compared in the search for a solution. The flap design is an important factor affecting the frequency and severity of postoperative complications [10-12].
Alveolar osteitis (AO), also known as “dry socket,” is reported to be a relatively common complication following impacted mandibular third molar removal surgery, where the incidence has been reported to be as high as 45% [13]. Crawford first described the term in 1876, and since then the condition has been referred to as localized osteitis, alveolar osteitis, alveoalgia, alveolitis sicca Dolorosa, septic socket, necrotic socket, fibrinolytic alveolitis, as well as localized osteomyelitis [14]. Though the etiology of AO remains debatable, its cause has often been attributed to the partial or total disintegration of the blood clot in the alveolar socket, which leads to a loss of the reparative agents normally present in coagulated blood. AO typically presents with painful, unfilled sockets at the surgical site 2-5 days post-extraction, commonly accompanied by unpleasant taste, halitosis, and pain radiating to one or both ears [13]. To help reduce the incidence of AO as well as other complications, studies have investigated the effects of a wide variety of proposed etiologic factors such as antibiotics, chlorhexidine rinses, tobacco products, menstrual status, and the age of the patient, but few investigators have taken into account the potential differences in the efficacy of alternative surgical techniques in preventing the initiation of AO.
One such surgical alternative in consideration is the alteration of flap designs and primary closure. In most modern oral and maxillofacial surgery offices/clinics, the most common approaches when accessing impacted mandibular third molars utilize either the envelope flap (EF) with a distal relieving incision extended laterally to the ramus or the modified triangular flap (MTF) [15]. While both techniques provide adequate access as well as space to perform the necessary ostectomy to expose the dental crown for tooth removal, these designs do not allow for primary closure over the sound bone which has been thought to contribute to higher incidences of complications like AO [2].
The surgical removal of third molar teeth may result in a number of complications, including alveolar osteitis (AO). Third molar surgery has been associated with a variety of complications and side effects. The flap design is one of the factors influencing the severity of these complications and side effects.
The envelope flap with a distal relieving incision to the ramus4 and the triangular flap, which was first described by Szmyd are the most common approaches in impacted third molar surgery. Several studies have been conducted to compare the effect of those flaps on pain, swelling, trismus, and primary wound healing in the postoperative period. Although it has been reported that the influence of flap design is of importance on wound healing after third molar surgery, there is not an agreement. Whereas some authors reported that flap design had no clinical significance in point of postoperative pain and trismus, others stated that triangular flap is more advantageous for primary wound healing and wound dehiscence was less when a triangular.
From the existing literature, it is obvious that the type of incision is an important consideration in the surgical removal of the impacted teeth. Further, it is vital to note that the design of the flap is a critical parameter in the surgery of third molars. The design of the flap influences the visibility and accessibility to the impacted tooth and also has an impact on the subsequent healing process of the surgical defect created following surgery.
From this study it is concluded that incidence of alveolar osteitis with modified triangular flap is less compared to envelope flap in the patients who have undergone mandibular third molar surgery. With a rich case bank established over 3 decades we have been able to publish extensively in our domain [16-26]. Based on this inspiration we aim to do a systematic review on comparative evaluation of incidence of alveolar osteitis with bayonet flap and envelope flap in third molar surgery.
Aim
The aim of this systematic review was to analyze the existing literature to compare and evaluate envelope flap and bayonet flap in preventing the occurrence of alveolar osteitis following mandibular third molar surgery.
Structured Question
Is bayonet flap effective in lowering the postoperative incidence of alveolar osteitis compared to envelop flap following mandibular third molar surgery?.
PICO analysis
Population: Patients undergoing mandibular third molar surgery.
Intervention: Bayonet flap.
Comparison: Envelope flap.
Outcome: Alveolar Osteitis.
Materials and Methods
Search methodology
Following Figures 1A-R and 2 explains the search methodology.
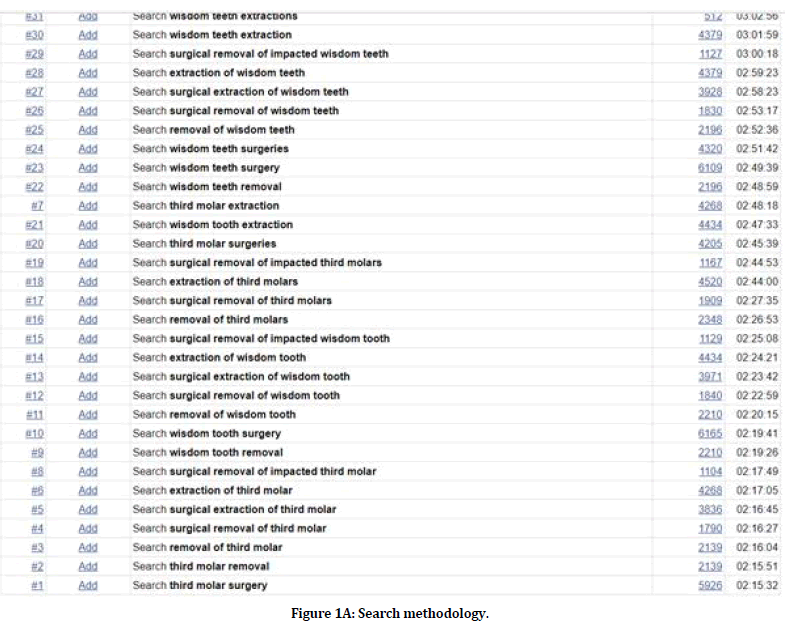
Figure 1a. Search methodology.

Figure 1b. Search methodology.
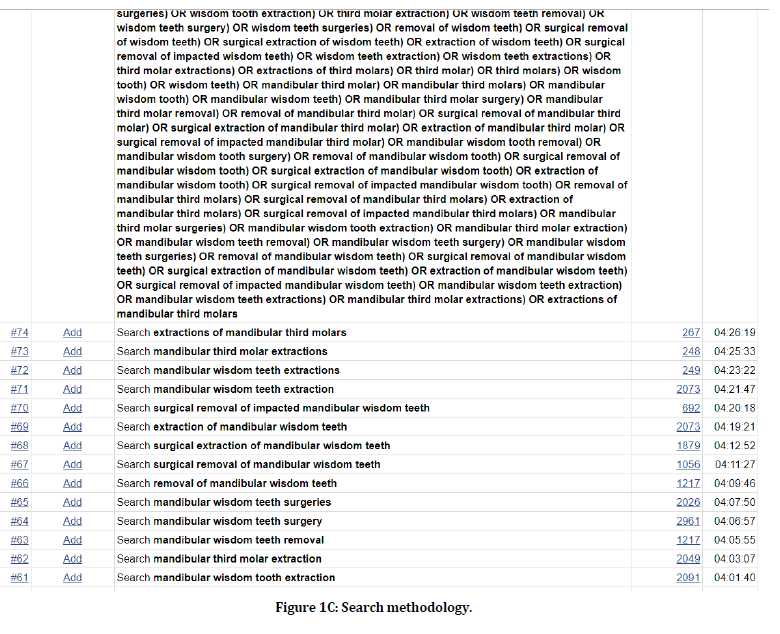
Figure 1c. Search methodology.
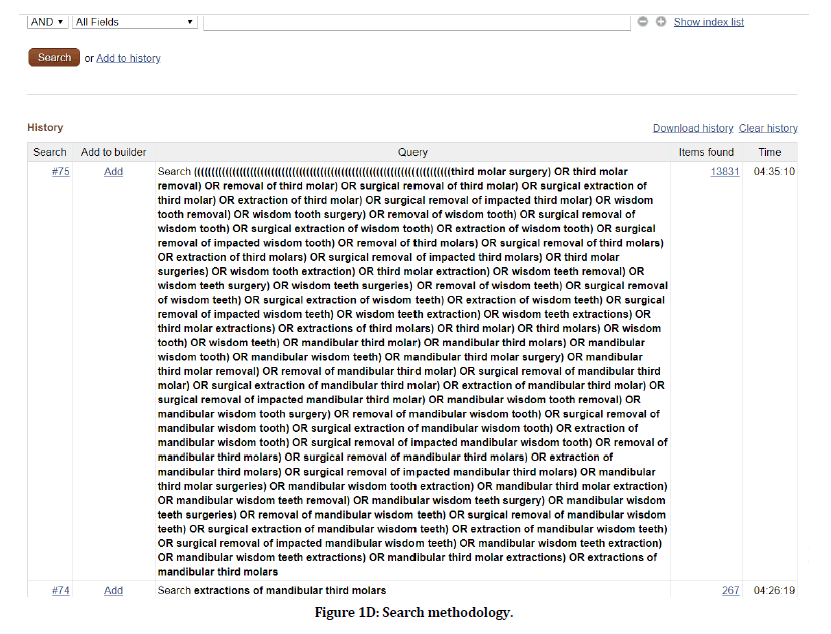
Figure 1d. Search methodology.
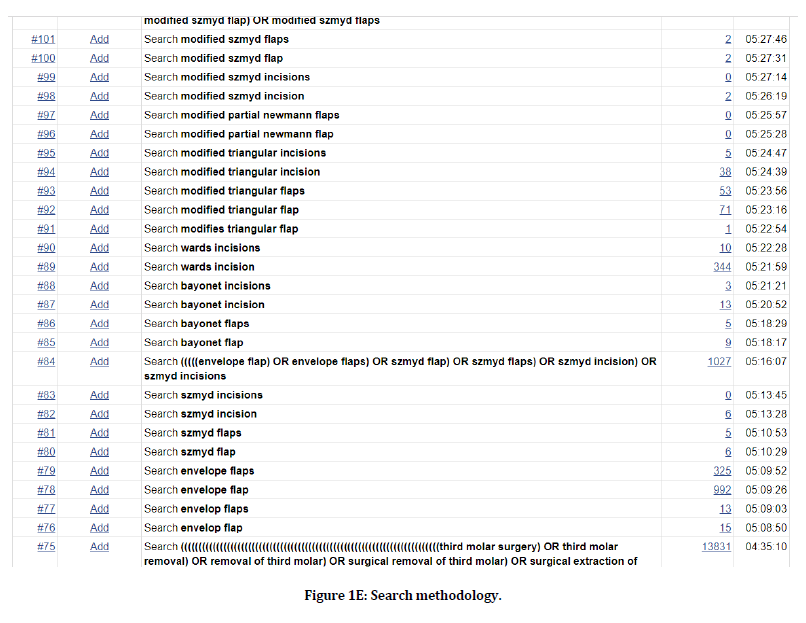
Figure 1e. Search methodology.
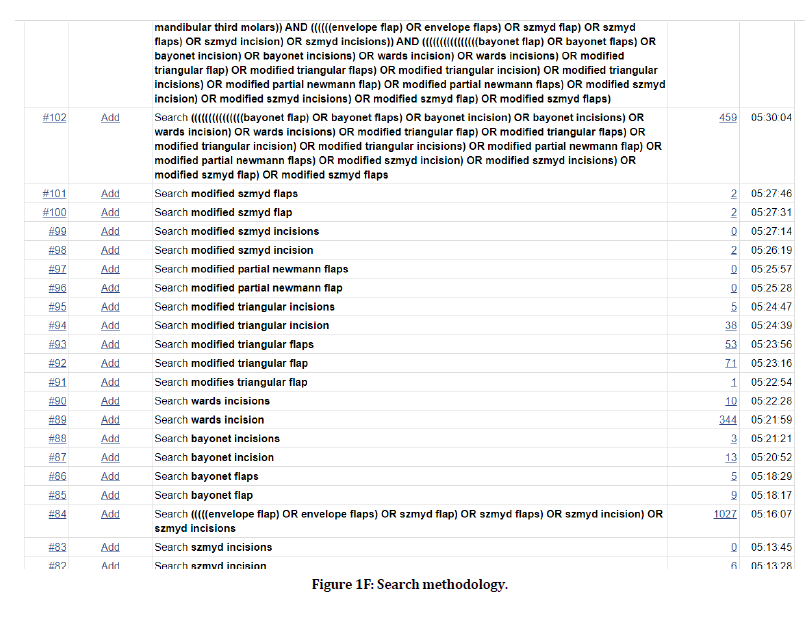
Figure 1f. Search methodology.
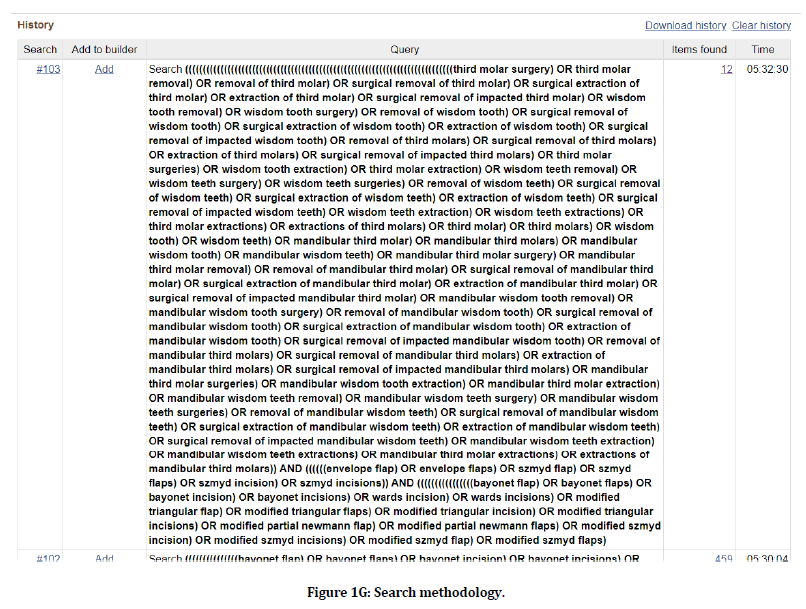
Figure 1g. Search methodology.
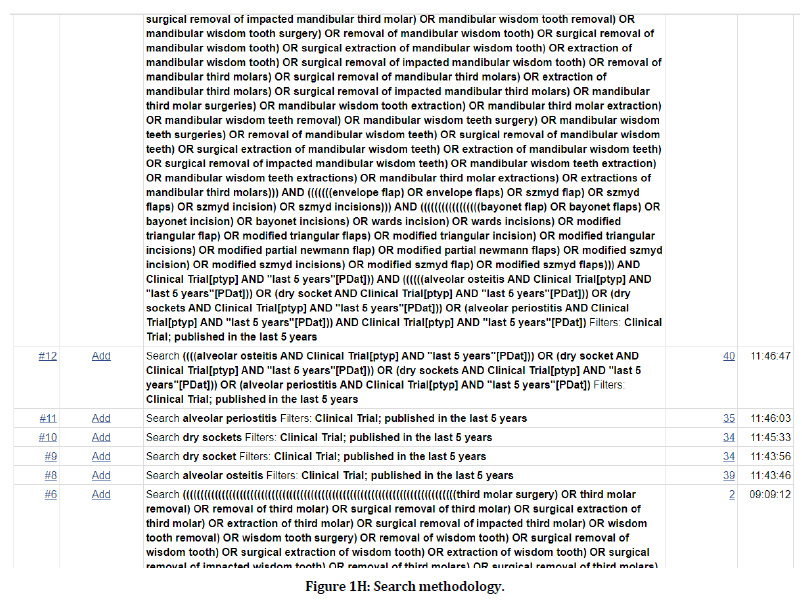
Figure 1h. Search methodology.
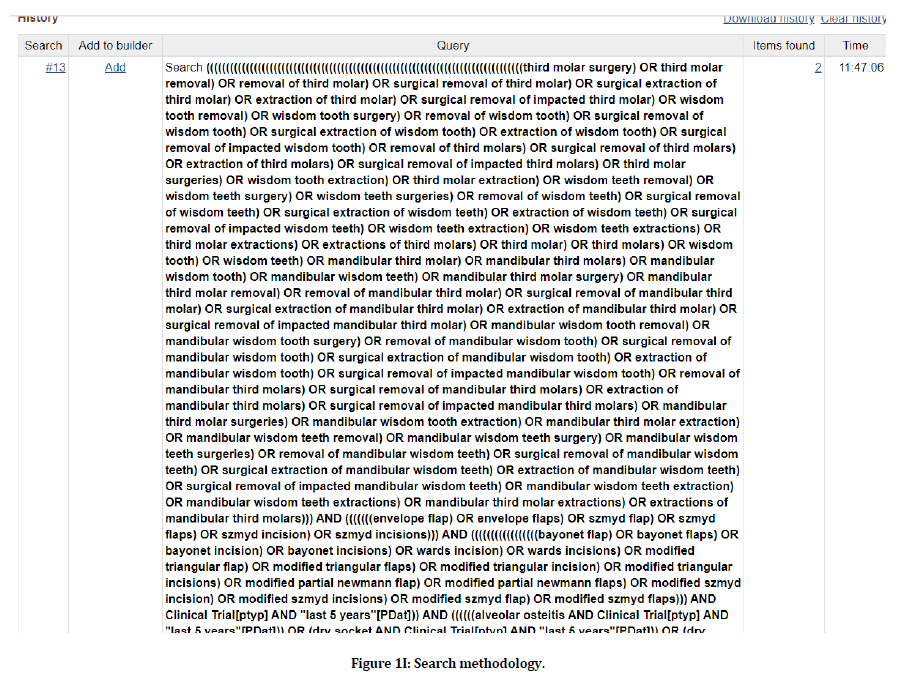
Figure 1i. Search methodology.
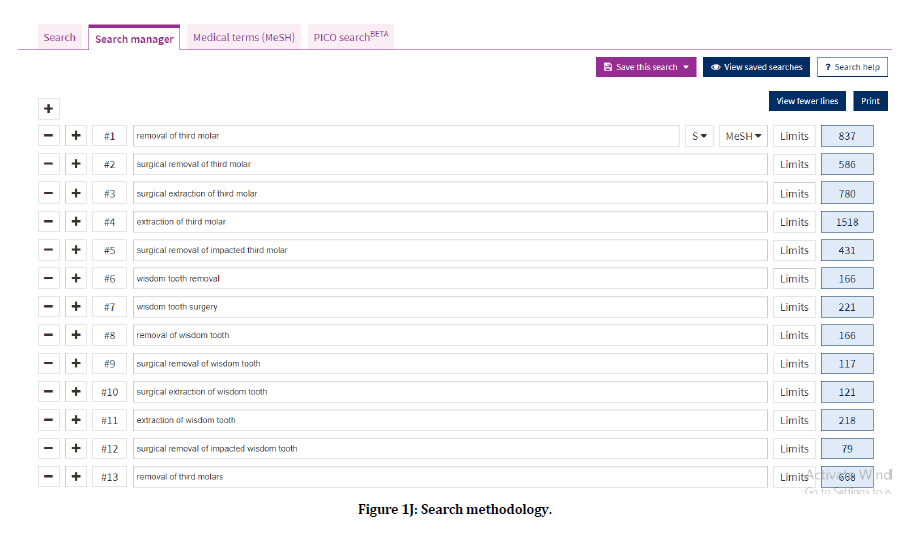
Figure 1j. Search methodology.
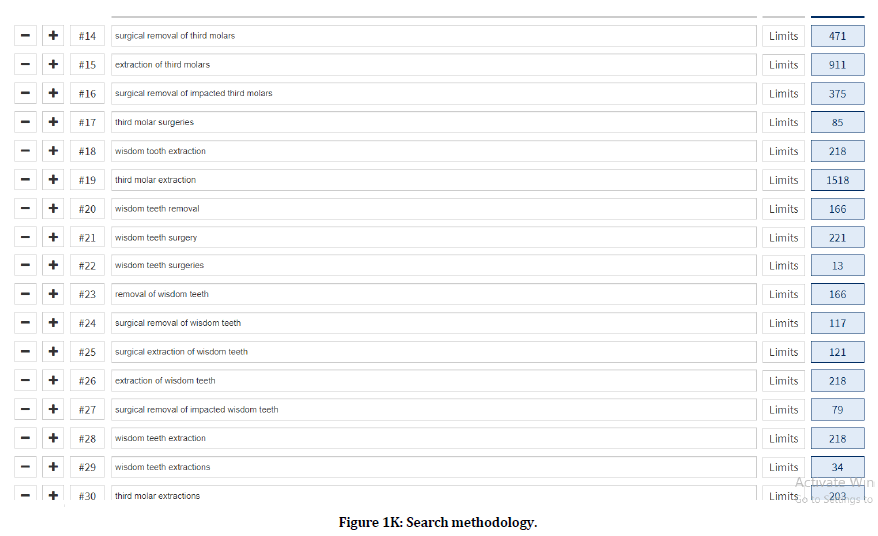
Figure 1k. Search methodology.
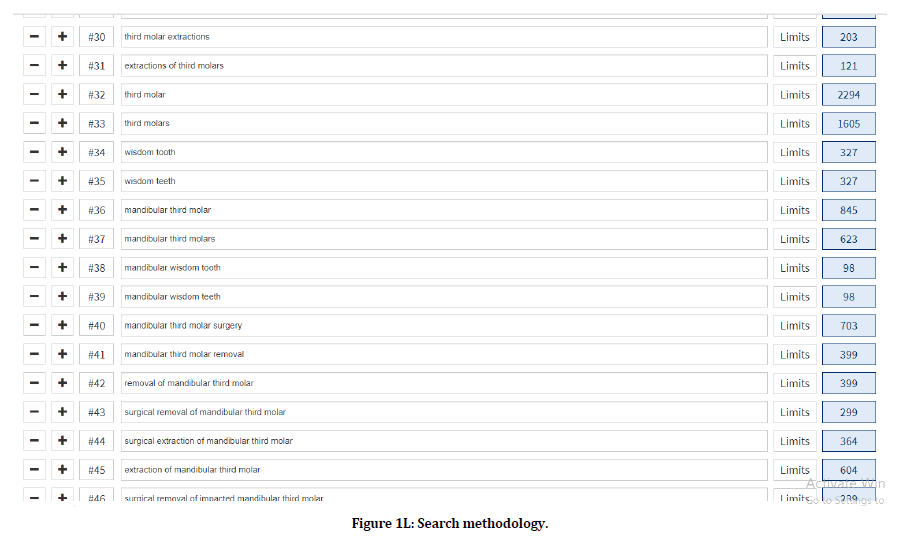
Figure 1l. Search methodology.
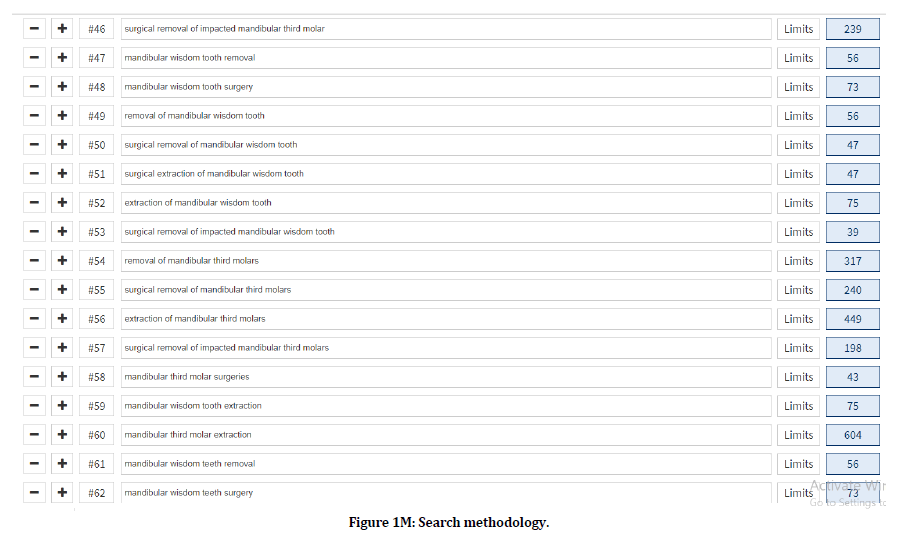
Figure 1m. Search methodology.
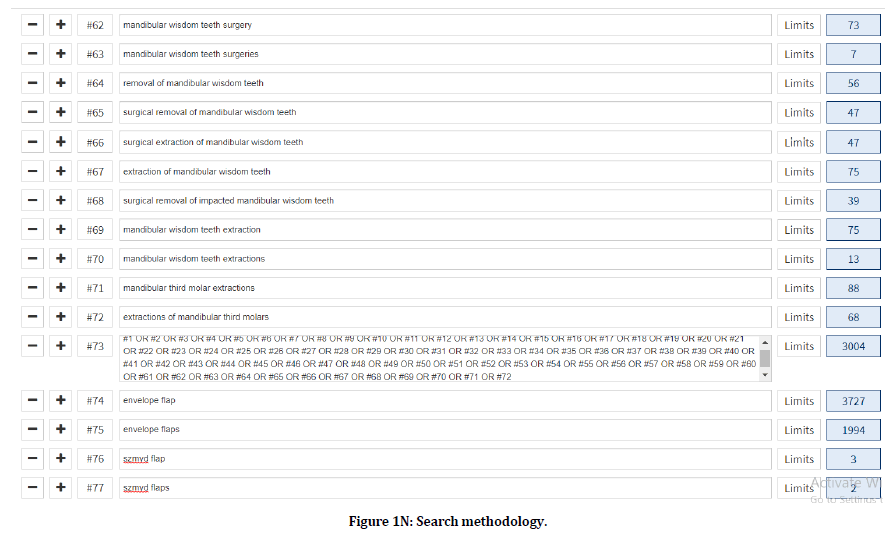
Figure 1n. Search methodology.
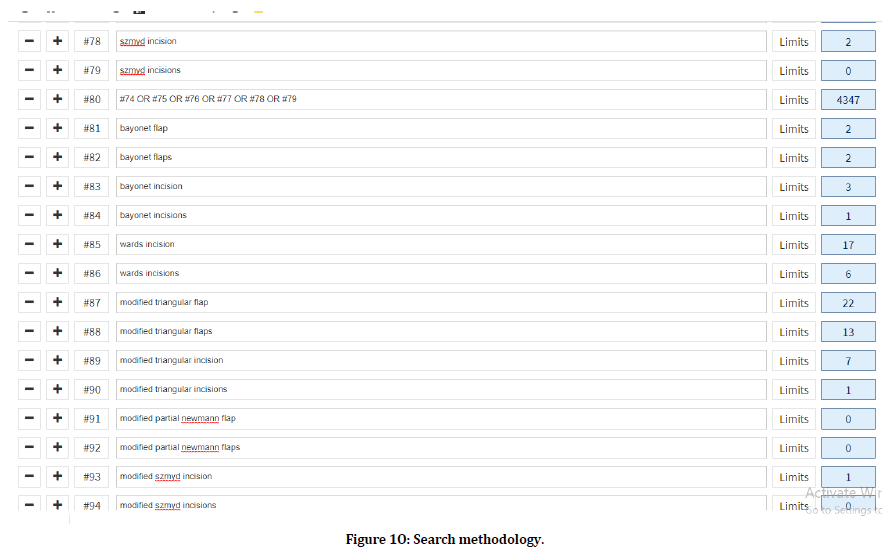
Figure 1o. Search methodology.
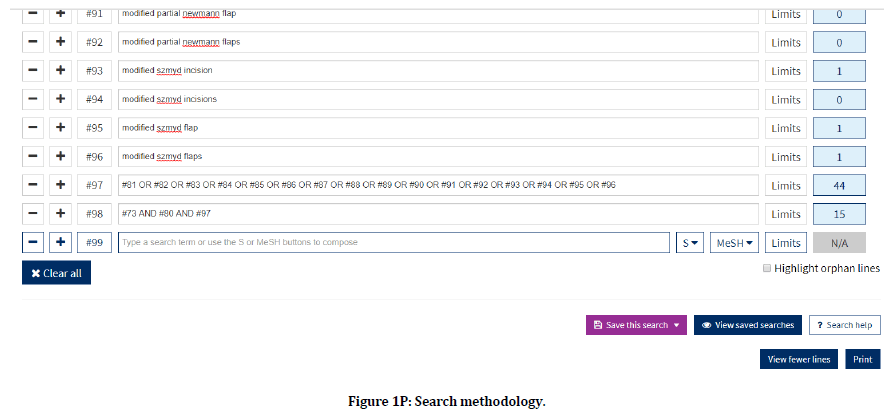
Figure 1p. Search methodology.
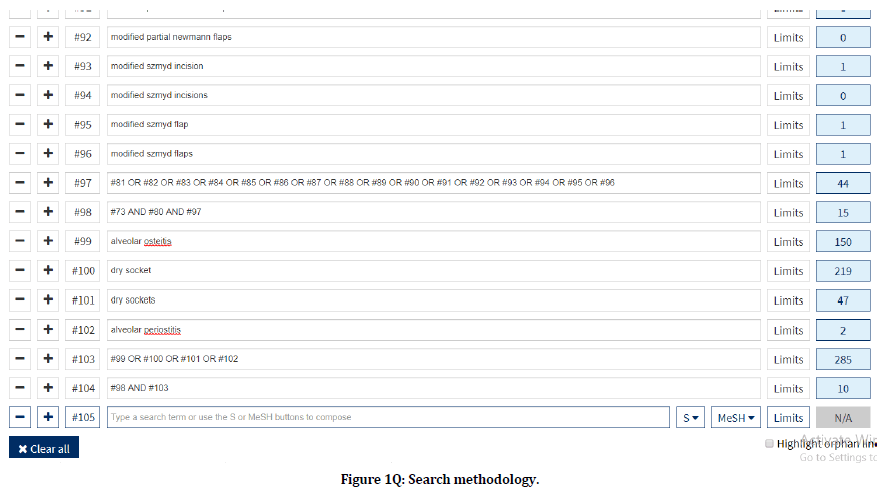
Figure 1q. Search methodology.
Figure 1r. Search methodology.
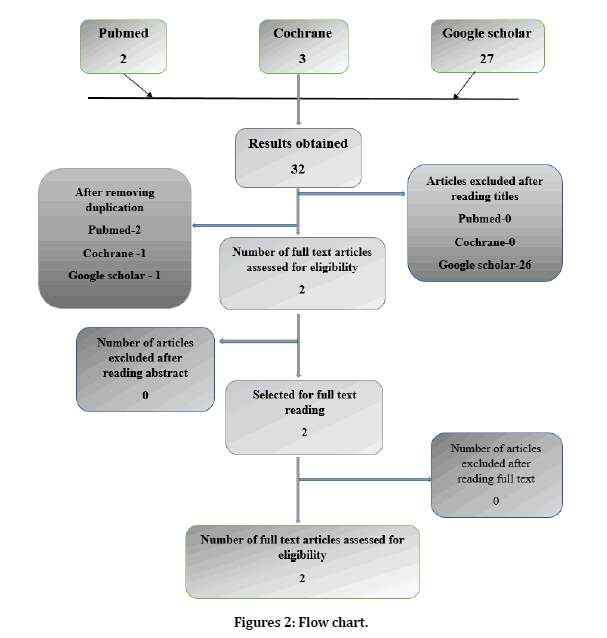
Figure 2. Flow chart.
Inclusion criteria
Criteria for considering studies for the Review
Types of studies
Randomized controlled trials
Clinical trials
Types of participants
Patients undergoing mandibular third molar surgery.
Types of intervention
Postoperative incidence of alveolar osteitis is evaluated using bayonet flap for the patients undergoing mandibular third molar surgery.
Types of comparison
Postoperative incidence of alveolar osteitis is evaluated using envelope flap for the patient undergoing mandibular third molar surgery.
Types of outcome measures
Post-operative incidence of alveolar osteitis for the patient undergoing mandibular third molar surgery.
Exclusion criteria
The following studies were excluded
Review articles.
Animal studies.
Invitro studies.
Studies not meeting inclusion criteria.
Languages other than English.
Sources used
The data bases of PubMed, cochrane and google scholar were searched for the related topics.
We used free-text terms to search the following journals.
British Journal of Oral and Maxillofacial Surgery.
International Journal of Oral and Maxillofacial Surgery.
Journal of Oral and Maxillofacial Surgery.
Journal of Cranio Maxillofacial Surgery.
Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.
Only articles in English and human species were applied during the electronic search to include all the possible clinical trials that are relevant for the search phase of the systematic review. A reference list of the identified randomized trials was also checked for possible additional studies.
Search flow chart (Figure 2)
Data collection and analysis
Screening and selection
An electronic search was carried out using the keywords in the Search engines- PubMed, Cochrane, and Google Scholar which yielded a total of 32 articles. Based on pre-set inclusion and exclusion criteria, the titles of the studies identified from the search were assessed independently by two review authors. Conflicts concerning the inclusion of the studies were resolved by discussion. Twenty-six articles were excluded after reading titles. Two titles were identified from the search after excluding four duplications. Abstracts of selected articles were reviewed independently. No articles were excluded after reading the abstract. Full-text articles were retrieved for two relevant studies.
The reference list of the full-text articles were reviewed for identifying additional studies. Titles of articles relevant to the review were selected by discussion. Quality Assessment criteria to evaluate the studies were decided by two review authors in accordance with CONSORT guidelines. The risk of bias for each study was independently assessed by the review authors and conflicts concerning the risk of bias were sorted by discussion.
Data extraction
Data extraction for general characteristics of studies and variables of outcome was done.
For each trial the following data were recorded
Author and journal.
Study design.
Sample size.
Participants and group.
Methodology.
Outcome measures.
Results.
Conclusion.
Variable of interest
It is given in table 1.
| S.No | Variables Of Interest |
|---|---|
| 1 | Alveolar osteitis |
Table 1: Variable interest.
Quality assessment
The quality assessment of included trials was undertaken independently as a part of data extraction process. Four main quality criteria were examined.
1. Method of Randomization, recorded as
a) YES- Adequate as described in the text.
b) NO- Inadequate as described in the text.
c) Unclear in the text.
2. Allocation Concealment, recorded as
a) YES- Adequate as described in the text.
b) NO- Inadequate as described in the text.
c) Unclear in the text.
3. Outcome assessors Blinded to intervention, recorded as
a) YES- Adequate as described in the text.
b) NO- Inadequate as described in the text.
c) Unclear in the text.
4. Completeness of Follow up (was there a clear explanation for withdrawals and dropouts in each treatment group) assessed as
a )YES- Dropouts were explained.
b) NO- Dropouts were not explained.
c) None- No Dropouts or withdrawals.
Other methodological criteria examined included:
1. Presence or Absence of sample size calculation.
2. Comparability of Groups at the start.
3. Clear Inclusion or Exclusion criteria.
4. Presence or Absence of estimate of measurement error.
Risk of bias in included studies
The study was assessed to have a “High risk” of bias if it did not record a “Yes” in three or more of the four main categories, "Moderate Risk "if two out of four categories did not record a "Yes", and “Low Risk” if all the four categories recorded if randomization assessor, Blinding and Completeness of follow up were considered Adequate. In case of non-randomized and clinical trials without control group, it is recorded as not applicable.
Results and Discussion
Table 2 shows the general characteristics of the studies.
| S.No | Author | Year | Study design | Sample size | Age | Technique Used | Method of Evaluation |
|---|---|---|---|---|---|---|---|
| 1 | Jeffrey A Elo et al | 2016 | Randomized single-blinded clinical study | N=196 | No age limit | One group Bayonet flap and another group Envelope flap Two groups got novel incision design | Post-operative incidence of alveolar osteitis using clinical assessment |
| 2 | Goksel Simsek Kaya | 2019 | Randomized clinical study | N=60 | 18-31yrs | One group Bayonet flap and another group Envelope flap | Post-operative incidence of alveolar osteitis using clinical assessment |
Table 2: General characteristics of the studies.
Table 3 explains the data extraction.
| S.No. | Author and year | Technique used | Method of evaluation | Incidence values | Outcomes |
|---|---|---|---|---|---|
| 1 | Jeffrey A Elo et al 2016 | One group Bayonet flap and another group Envelope flap. Two groups got novel incision design | Post-operative incidence of alveolar osteitis using clinical assessment | Post-operative alveolar osteitis | Post-operative incidence of alveolar osteitis was significantly less with bayonet flap |
| Bayonet flap group=0.10 | |||||
| Envelope flap group=0.13 | |||||
| 2 | Goksel Simsek Kaya et al 2019 | One group Bayonet flap and another group Envelope flap | Post-operative incidence of alveolar osteitis using clinical assessment | Post-operative alveolar osteitis | Post-operative incidence of alveolar osteitis was significantly less with bayonet flap |
| Bayonet flap group=0 | |||||
| Envelope flap group=0.14 |
Table 3: Data extraction.
Table 4 shows the evidence level of selected articles.
| S.No | Author and year | Study design | Level of Evidence |
|---|---|---|---|
| 1 | Jeffrey A Elo et al 2016 | Randomized single-blinded study | 1 |
| 2 | Goksel Simsek Kaya et al 2019 | Randomized clinical study | 1 |
Table 4: Evidence level of selected articles.
Table 5 shows the risk of bias- major criteria.
| S.No. | Study | Randomization | Allocation concealment | Assessor Blinded | Dropouts described | Risk of Bias |
|---|---|---|---|---|---|---|
| 1 | Jeffrey A Elo et al 2016 | Yes | Yes | Yes | None | Moderate |
| 2 | Goksel Simsek Kaya et al | Yes | Yes | Yes | None | Moderate |
Table 5: Risk of bias- major criteria.
Table 6 determines risk of bias-minor criteria.
| S.No. | Study | Sample Justified | Baseline Comparison | I/E Criteria | Method of error |
|---|---|---|---|---|---|
| 1 | Jeffrey A Elo et al 2016 | Yes | Yes | Yes | No |
| 2 | Goksel Simsek Kaya et al 2019 | Yes | Yes | Yes | No |
Table 6: Risk of bias-minor criteria.
Table 7 shows the summation for individual parameter.
| S.No | Author | Year | Evaluation period | Outcome |
|---|---|---|---|---|
| 1 | Jeffrey A Elo et al 2016 | 2016 | POD 4th day | There wasn’t much significant difference between the two groups, but results are in favor of Bayonet flap |
| 2 | Goksel Simsek Kaya et al 2019 | 2019 | POD 4th day | There was a significant difference between two groups, results are in favor of Bayonet group |
Table 7: Summation table for individual parameter.
Figure 3 illustrates the comparison of incidence ofalveolar Osteitis.
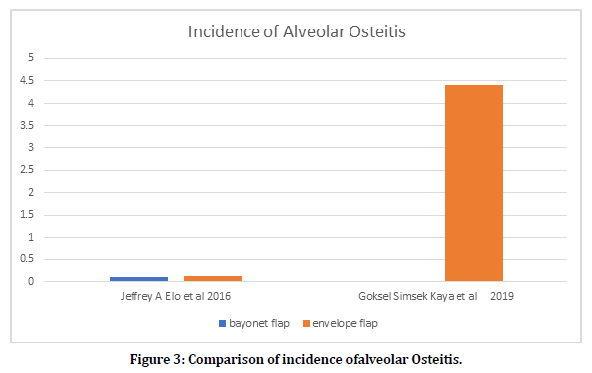
Figure 3. Comparison of incidence ofalveolar Osteitis.
Impacted third molar surgery is a very common procedure. A variety of factors, such as the duration of the operation, difficulty of the surgery, magnitude of the ostectomy, lack of oral hygiene, or the surgeon’s experience, affect the severity of postoperative complications and morbidity. It has also been proposed that the flap design is effective in the postoperative course and, therefore, results of different flaps have been evaluated.
The two flap designs used in this study are both frequently used and have acceptance among oral surgeons. The envelope flap has a broad base and, consequently, a good blood supply. The surgical site can be adequately exposed, and the sulcular incision can be extended if needed. It has some disadvantages, however. A larger flap also means more osteoclastic activity and more bone loss. Wound dehiscence distal to the second molar is said to be another shortcoming of envelope flap design. These gaps are generally located adjacent to the second molar, serve as a trap for foods, and maybe a good environment for bacteria, which may lead to alveolar osteitis and soft tissue abscesses. Because less tissue is elevated and the buccal aspect of the second molar is protected, the modified triangular flap has been asserted to be a more conservative technique.
Alveolar osteitis (AO) is often a significant cause of pain and discomfort following mandibular third molar removal surgery. There is still no consensus concerning whether or not the flap design applied in third molar surgery affects the post‐operative period [27,28]. Although some authors have reported that post‐operative comfort and wound healing are directly correlated with the flap design applied [27]. The degree of swelling and the severity of pain are the principal indicators of post‐operative patient comfort following surgical removal of third molar [29]. There is no consensus in the literature on the effect of flap design on post‐operative pain, although flap design had no direct effect on pain, the incidence of alveolar osteitis was higher in patients receiving envelope flaps, who therefore had higher VAS scores [30].
Mucoperiosteal flap preparation results in increasing osteoclast activity at the alveolar process, thus triggering the loss of alveolar bone [7,31]. Soft tissue tensions due to hematoma and masticatory muscle movements in the surgical field may induce wound dehiscence in the first few days post‐operatively. Dehiscence creates a potential trap for food particles and a good environment for bacteria, hence leading to post‐ operative alveolar osteitis, soft tissue abscesses and long‐term discomfort and additional treatment requirements [3,7,31,32]. From the patient’s perspective, dehiscence may prolong discomfort and cause continuous pain [31]. Our results support those of previous studies reporting frequent wound dehiscence in the first stage of wound healing in patients receiving envelope flaps [31,32,33].
The purpose of this study was to compare the bayonet flap against the envelope flap in reducing the incidence of AO. Though its exact etiology is unknown, many potential risk factors for AO have been identified. Several preventative techniques have been proposed to address this issue with varying degrees of success. There are reports that regular irrigation with a 0.12% chlorhexidine solution both pre-operatively and up to 7 days postoperatively can lead to a better prognosis [15,34]. In addition, topical as well as systemic antibiotics (such as tetracycline and metronidazole) may help reduce the prevalence of pathologic states [35,36].
Envelope flap
The envelope flap was performed with a sulcular incision extending from the first molar to the second and a distal relieving incision to the mandibular ramus. The incision was made from a point immediately medial to the external oblique ridge as far as the center of the distal line angle of the second molar. A sulcular buccal incision was then made from that point made to the center of the first molar. The mucoperiosteal flap was elevated completely as far as the buccal surface of the mandible. The lingual tissues were only retracted superficially (Figure 4).
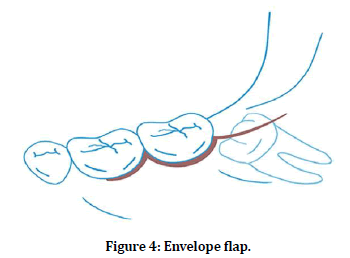
Figure 4. Envelope flap.
Modified triangular flap
The modified triangular flap was implemented as described by Szmyd [37] and as subsequently modified by Jakse. The first part of the incision was similar to that described in the envelope flap technique. The incision extended from the mandibular ramus as far as the distobuccal crown edge of the second molar. An oblique perpendicular incision of approximately 10 mm was then made to the mandibular vestibulum. The periodontium of the second molar was only disturbed at the distofacial edge. A lingual mucoperiosteal flap similar to that used with the envelope flap was also raised (Figure 5).
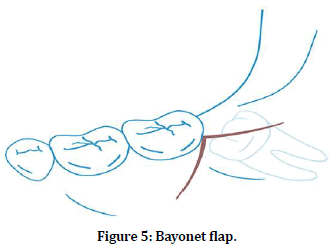
Figure 5. Bayonet flap.
Interpretation of results
In a study conducted by other authors in 2016, a total sample size of 196 with one group consisting of 61 patients and others with 65 patients. One group was given an envelope flap and one group was given bayonet flap. In the envelope flap group, after undergoing mandibular third molar surgery, the occurrence of AO was 8 out of 61 and was 7 out of 65 with bayonet flap. The incidence was 0.13 in the envelope flap group and 0.10 in the bayonet flap group. In the study conducted by other authors in 2019, a total number of 30 patients having bilateral impacted mandibular third molar with each group consisting of 30 patients, one group was given envelope flap and another group received bayonet flap. There was a significant reduction in the occurrence of AO in the bayonet flap group with 0 out of 30 compared to envelope flap group where the occurrence of AO was 4 out of 30.
Summary
The aim of this systematic review is to assess the efficacy of Bayonet flap with Envelope flap on the Incidence of Alveolar Osteitis in impacted mandibular third molar surgery. There were 2 randomized controlled trials included in this systematic review. Both of the studies have used envelope flap and bayonet flap to compare the incidence of postoperative alveolar osteitis occurrence. In these studies, only less number of patients was evaluated. So more studies to be done in the future. Thus in this systematic review, we conclude that modified triangular flap (bayonet flap) had a lesser incidence of alveolar osteitis when compared to envelope flap in mandibular third molar surgery.
Conclusion
In this systematic review we have concluded that, on average, modified triangular flap (bayonet flap) had a lesser incidence of alveolar osteitis when compared to envelope flap in mandibular third molar surgery. More studies have to be done to evaluate the efficacy of the flaps.
Acknowledgments
The authors would like to acknowledge the help and support rendered by the department of oral and maxillofacial surgery and information technology of Saveetha Dental College and Hospitals for their constant assistance with the research.
Conflict of Interest
The authors declare no conflicts of interest.
References
- Laureano Filho JR, de Maurette MA, Cotinho M, et al. Clinical comparative study of the effectiveness of two dosages of dexamethasone to control postoperative swelling, trismus and pain after the surgical extraction of mandibular impacted third molars. Med Oral Patol Oral Cir Bucal 2008; 13:129–132.
- Goldsmith SM, De Silva RK, Tong DC, et al. Influence of a pedicle flap design on acute postoperative sequelae after lower third molar removal. Int J Oral Maxillofac Surg 2012; 41:371-375.
- Koyuncu BÖ, Çetingül E. Short-term clinical outcomes of two different flap techniques in impacted mandibular third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116:e179-84.
- Rabi A, Haris PM, Panickal DM, et al. Comparative evaluation of two different flap designs and postoperative outcome in the surgical removal of impacted mandibular third molar. J Contemporary Dent Practice 2017; 18:807-811.
- Majid OW, Al-Mashhadani BA. Perioperative bromelain reduces pain and swelling and improves quality of life measures after mandibular third molar surgery: A randomized, double-blind, placebo-controlled clinical trial. J Oral Maxillofac Surg 2014; 72:1043-1048.
- Ibikunle AA, Adeyemo WL, Ladeinde AL. Oral health-related quality of life following third molar surgery with either oral administration or submucosal injection of prednisolone. Oral Maxillofac Surg 2016; 20:343-352.
- Dolanmaz D, Esen A, Isik K, et al. Effect of 2 flap designs on postoperative pain and swelling after impacted third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol 2013; 116:e244-246.
- Suarez-Cunqueiro MM, Gutwald R, Reichman J, et al. Marginal flap versus paramarginal flap in impacted third molar surgery: A prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont 2003; 95:403-408.
- Baqain ZH, Al-Shafii A, Hamdan AA, et al. Flap design and mandibular third molar surgery: a split mouth randomized clinical study. Int J Oral Maxillofac Surg 2012; 41:1020-1024.
- Yolcu ÜM, Acar AH. Comparison of a new flap design with the routinely used triangular flap design in third molar surgery. Int J Oral Maxillofac Surg 2015; 44:1390-1397.
- Kumar S, Sarumathi T, Veerabahu M, et al. To compare standard incision and comma shaped incision and its influence on post–operative complications in surgical removal of impacted third molars. J Clin Diagnost Res 2013; 7:1514.
- Sanchis Bielsa JM, Hernández-Bazán S, Peñarrocha Diago M. Flap repositioning versus conventional suturing in third molar surgery. Med Oral Patol Oral Cir Bucal 2008; 13:138–142.
- Kolokythas A, Olech E, Miloro M. Alveolar osteitis: A comprehensive review of concepts and controversies. Int J Dent 2010; 249073.
- Cardoso CL, Rodrigues MT, Júnior OF, et al. Clinical concepts of dry socket. J Oral Maxillofac Surg 2010; 68:1922-1932.
- Piecuch JF. What strategies are helpful in the operative management of third molars? J Oral Maxillofac Surg 2012; 70:S25–S32.
- Wahab PA, Nathan PS, Madhulaxmi M, et al. Risk factors for post-operative infection following single piece osteotomy. J Maxillofac Oral Surg 2017; 16:328-332.
- Eapen BV, Baig MF, Avinash S. An Assessment of the incidence of prolonged postoperative bleeding after dental extraction among patients on uninterrupted low dose aspirin therapy and to evaluate the need to stop such medication prior to dental extractions. J Maxillofac Oral Surg 2017; 16:48–52.
- Patil SB, Durairaj D, Kumar GS, et al. Comparison of extended nasolabial flap versus buccal fat pad graft in the surgical management of oral submucous fibrosis: A prospective pilot study. J Maxillofac Oral Surg 2017; 16:312-321.
- Jain M, Nazar N. Comparative evaluation of the efficacy of intraligamentary and supraperiosteal injections in the extraction of maxillary teeth: A randomized controlled clinical trial. J Contemporary Dent Practice 2018; 19:1117–1121.
- PC J, Marimuthu T, Devadoss P, et al. Prevalence and measurement of anterior loop of the mandibular canal using CBCT: A cross sectional study. Clin Implant Dent Related Res 2018; 20:531-534.
- Marimuthu M, Andiappan M, Wahab A, et al. Canonical Wnt pathway gene expression and their clinical correlation in oral squamous cell carcinoma. Indian J Dent Res 2018; 29:291.
- Wahab PA, Madhulaxmi M, Senthilnathan P, et al. Scalpel versus diathermy in wound healing after mucosal incisions: A split-mouth study. J Oral Maxillofac Surg 2018; 76:1160-1164.
- Abhinav RP, Selvarasu K, Maheswari GU, et al. The patterns and etiology of maxillofacial trauma in South India. Annals Maxillofac Surg 2019; 9:114.
- Ramadorai A, Ravi P, Narayanan V. Rhinocerebral mucormycosis: A prospective analysis of an effective treatment protocol. Annals Maxillofac Surg 2019; 9:192-196.
- Senthil Kumar MS, Ramani P, Rajendran V, et al. Inflammatory pseudotumour of the maxillary sinus: Clinicopathological report. Oral Surg 2019; 12:255-259.
- Sweta VR, Abhinav RP, Ramesh A. Role of virtual reality in pain perception of patients following the administration of local anesthesia. Annals Maxillofac Surg 2019; 9:110–113.
- Korkmaz YT, Mollaoglu N, Ozmeriç N. Does laterally rotated flap design influence the short-term periodontal status of second molars and postoperative discomfort after partially impacted third molar surgery?. J Oral Maxillofac Surg 2015; 73:1031-1041.
- Chen YW, Lee CT, Hum L, et al. Effect of flap design on periodontal healing after impacted third molar extraction: A systematic review and meta-analysis. Int J Oral Maxillofac Surg 2017; 46:363-372.
- Chaudhary M, Singh M, Singh S, et al. Primary and secondary closure technique following removal of impacted mandibular third molars: A comparative study. National J Maxillofac Surg 2012; 3:10.
- Kirk DG, Liston PN, Tong DC, et al. Influence of two different flap designs on incidence of pain, swelling, trismus, and alveolar osteitis in the week following third molar surgery. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontol 2007; 104:1-6.
- Jakse N, Bankaoglu V, Wimmer G, et al. Primary wound healing after lower third molar surgery: evaluation of 2 different flap designs. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont 2002; 93:7-12.
- Sandhu A, Sandhu S, Kaur T. Comparison of two different flap designs in the surgical removal of bilateral impacted mandibular third molars. Int J Oral Maxillofac Surg 2010; 39:1091-1096.
- Alqahtani NA, Khaleelahmed S, Desai F. Evaluation of two flap designs on the mandibular second molar after third molar extractions. J Oral Maxillofac Pathol 2017; 21:317.
- Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: postoperative complications and their risk factors. J Canadian Dent Assoc 2007; 73.
- Lee JY, Do HS, Lim JH, et al. Correlation of antibiotic prophylaxis and difficulty of extraction with postoperative inflammatory complications in the lower third molar surgery. Br J Oral Maxillofac Surg 2014; 52:54-57.
- Almendros-Marqués N, Berini-Aytés L, Gay-Escoda C. Influence of lower third molar position on the incidence of preoperative complications. Oral Surg Oral Med Oral Pathol Oral Radiol Endodont 2006; 102:725-732.
- Szmyd L. Impacted teeth. Dent Clin North Am 1971; 15:299–318.
Author Info
Ramvihari Thota, Senthilnathan Periasamy* and Mahathi N
Department of Oral and Maxillofacial Surgery, Saveetha Dental College and Hospitals, Saveetha Institute of Medical and Technical Sciences, Saveetha University Tamilnadu, Chennai, IndiaCitation: Ramvihari Thota, Senthilnathan Periasamy, Mahathi N, Comparative Evaluation of Incidence of Alveolar Osteitis with Bayonet Flap and Envelope Flap in Third Molar Surgery: A Systematic Review, J Res Med Dent Sci, 2021, 9 (2): 156-172.
Received: 29-Sep-2020 Accepted: 02-Feb-2021
