Review - (2022) Volume 10, Issue 8
Clinico-Epidemiological Characterization of Paediatric Ocular Trauma: A Systematic Review
Fahad Mohammed Albaqami1*, Muhanad Althbaiti1, Abdulrahman Albugami1, Abdulsalam Alshehri1, Ahmed Salah Saleh Alosaimi1, Majed Mohammed Albaqami2 and Abdulhamid Alghamdi3
*Correspondence: Fahad Mohammed Albaqami, Medical Student, College Of Medicine, Taif University, Taif, Saudi Arabia, Email:
Abstract
Background: Children's non-congenital monocular blindness is most commonly caused by ocular trauma. Seven percent of all injuries to them are the result of these accidents, and 10-15 percent of eye disorders are caused by these accidents. Evidence suggests that children account for 12.5 percent to 33.7 percent of all eye injury admissions. Aim: To give a systematic review of ocular trauma, focusing on the etiology and patient demographics as well as the type of injury. Methodology: Articles were chosen using a systematic search in the Medline (PubMed), Google Scholar, Science Direct, EMBASE, and CENTRAL (Cochrane Library) databases (2012 to 2022). The American Academy of Ophthalmology, Association for Research in Vision and Ophthalmology, and European Society of Ophthalmology annual meeting abstracts from 2012 onwards were also searched, in addition to online trial registers by index. Similar title and abstract search criteria were used for the EMBASE database. The data was gathered using an extraction form that was standardized. Hard-to-define papers were assessed by a second researcher. The selection of manuscripts followed the most recent 2020 PRISMA recommendations. Results: The systematic review included a total of 15 observational studies, 8 of which were prospective and 7 of which were retrospective. The patients' mean extracted age was determined to be 8.57 years. In every study, males suffered more ocular damage (extracted proportion being 73.24 percent). Studies revealed that the majority (60%) of injuries occurred outside the home, including on streets, in schools, on roads, in fields, and on playgrounds. Conclusion: It was concluded that men suffered more ocular trauma than women in the majority of studies, and that home was the most common site of trauma, followed by outside the home. Regarding the kind of trauma, the papers chosen for review most frequently reported blunt and projectile object trauma. The majority of paediatric trauma patients in the research chosen presented to the hospital within 12 hours, while in some studies they reported even beyond 24 hours.
Keywords
Ocular Trauma, Blunt trauma, Projectile trauma, Ocular injury
Introduction
Ocular injuries are the leading cause of non-congenital monocular blindness among children is ocular injury [1]. These injuries account for 7% of total injuries caused to them and 10-15% of the eye diseases [2]. Evidence suggests that of the total admissions of eye injury, 12.5% to 33.7% are constituted by children [3]. Children are more prone to injury than adults because of their immature motor system. Additionally, they are very curious to explore their environment without anticipating the danger. This makes them more prone to injury. Ocular injuries are not limited to physical impairment but also impact social, emotional, and psychological well-being with impending doom.
The mode of injury, causes of ocular injury, diagnosis, and management differ between adults and children. Children often do not report the injuries until substantial damage has occurred as they are unaware of the consequences. This leads to delays in reporting and seeking health care advice. Consequently, the ocular inflammation increases. Besides these, there are challenges in primary assessment due to young uncooperative patients. Delayed medical or surgical interventions affect the chances of recovery. The outcome of ocular trauma depends upon etiology, the severity of the trauma, and the duration between trauma and surgery. Thus, ocular trauma significantly affects the visual acuity among children. Also, the risk of developing amblyopia is more among them, which can affect their quality of life [4] Blindness due to trauma can be prevented in 90% of cases by taking preventive measures [5] Adopting relatively simple precautions like a safe environment by removing sharp or dangerous risks, education, and adult supervision [6]
The American Academy of Paediatrics (AAP) reports that 66% of ocular injuries are caused in children aged less than 16 years of age, and the children aged 9 to 11 years are most affected [7]. Previous literature suggests that male children are more prone to ocular injury than female children. A study conducted by Singh et al. reported that males had a 2.18 higher risk than females [8]. Children less than three years of age suffer ocular- injury caused to them by their handlers, while older children suffer self-inflicted injury. The injury is more commonly afflicted outdoors, either in schools or playgrounds, or on streets in developing countries, while the injuries were most commonly caused at home in developed countries [8,9] A few studies have reported no difference in injury on the basis of seasonality, while a few report that injury was more commonly reported in the summer and spring seasons. The injury was caused by a variety of things like wooden objects and vegetative matter or sports-related [10], which are usually play- objects of children. These include gully danda, pencil, wooden sticks, etc. Penetrating injuries were more commonly caused by sharp objects like knives, needles, etc. [11].
Birmingham Eye Trauma Terminology System (BETTS), developed by Kuhn et al., is an unambiguous system to categorize the ocular injury, and it depicts terminology (open and closed globe injury) [12]. Open globe injury is an emergency, and it requires immediate surgical intervention. This type of injury is most common in children younger than 2 years than closed-globe injury, which is more common among older children. Closed globe injury was more common than open-globe injury. Among closed globe, injuries include adnexal injury, subconjunctival hemorrhage, and corneal abrasion [13].
Although, the research conducted in developed countries is far more common than in developing countries. However, eye injuries are common in developing countries. The epidemiological profile of ocular injury varies from country to country, as well as the nature of the injury and visual outcome. These are influenced by socio-economic, cultural, and demographic factors of a region. There is a lack of reporting of representative data on the ocular injury of children in developing countries. This challenges the organized approach toward diagnosis and timely management. Thus, this systematic review aims to synthesize the demographic factors associated with ocular injury among children.
Aim
To provide a systematic review of ocular trauma with emphasis on the type of injury and patient demographics and to explore the causes associated.
Methods
Search strategy
We identified articles using a systematic search in MEDLINE (PubMed), Google Scholar, Science Direct, EMBASE, and CENTRAL (Cochrane Library) databases for studies using data from the last 10 years (2012 to 2022). We additionally searched online trial registers by index (http://ClinicalTrials.gov, http://www.controlledtrials. com) and proceedings of the American Academy of Ophthalmology, Association for Research in Vision and Ophthalmology, and European Society of Ophthalmology annual meeting abstracts from 2012 onwards. Search terms used were derivatives of “eye” AND “trauma” AND “children." The following search string was used for the MEDLINE search: (ocular [tiab] OR orbit*[tiab] OR eye [tiab] OR globe[tiab] OR adnexa*[tiab]) AND (trauma*[tiab] OR blast [tiab] OR explosi*[tiab] OR injury[tiab] OR damage*[tiab] OR thermal[tiab) AND (children [tiab] OR paediatrics[tiab] OR child[tiab] OR adolescents*[tiab]).
For the EMBASE database, similar search queries on title and abstract were employed. The Cochrane Library was searched on index. The references from related articles were searched manually. Reports on government and legislation were compiled from relevant sources and then hand-searched. Data on the most recent ocular firework trauma incidence rates were obtained from national trauma incidence records.
Eligibility criteria
Included articles had to supply information on trauma to the eye or its adnexa among pediatric populations less than 18 years of age. For general trauma publications to be considered, the ophthalmic component should be adequately described. Pediatric studies were included. To be eligible for inclusion, the extent of trauma and visual acuity had to be described, and the studies had to be having data not older than 2012 (Last 10 years). Excluded from analysis were non pediatric injuries, occupational injuries, wound classification studies, operation techniques, and case reports. English-only restriction was applied.
Data collection
A standardized extraction form was used to collect the data. A second investigator reviewed papers that were difficult to define. In the case of lacking data, we did not contact the authors of the original studies. We retrieved data on the author, publication year, region, study design, inclusion period, the total number of patients, type of ocular involvement, age, sex, and mode of damage for each included paper. Patient characteristics (such as gender and age) were taken from studies that provided enough detailed information. The weighted average by study size was used to obtain the mean. The study used a standardized trauma grading system, such as the Birmingham Eye Trauma Terminology System (BETTS) (Figure 1).
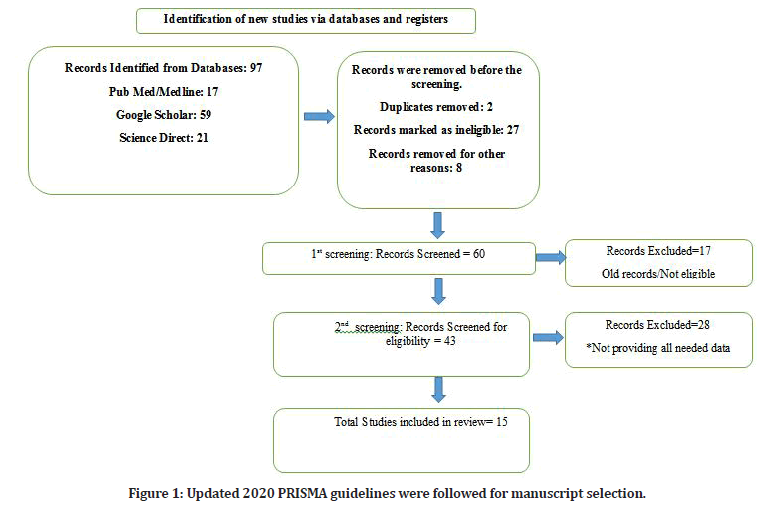
Figure 1: Updated 2020 PRISMA guidelines were followed for manuscript selection.
Results
A final total of 15 observational studies were included in the Systematic review, out of which 8 were prospective, and 7 were retrospective. The mean extracted age of the patients was found to be 8.57 years. In all the studies, males were more affected by ocular injuries (extracted proportion being 73.24%). Around 60 % of the studies showed that the place of getting the injury was outside the home, which included streets, schools, roads, fields, and playgrounds(Table 1).
| Sl. No. | Study | Design | Sample Size | Mean Age | Gender | Place of Injury | Object/Mode of Injury |
|---|---|---|---|---|---|---|---|
| 1. | Shah et al | Prospective | 12687 | 10.2 ± 5.1 years | Males (68.3%) | Home (62.2%) | Wooden Object (49.3%) |
| Females (31.7%) | Stone (16.4%) | ||||||
| 2. | Ebrahim A et al | Prospective | 75 (80 Eyes) | 5 years | Males (66 %) | Outside Home (54.67%) | Blunt (44%) |
| Observational | Females (33 %) | Sharp (39%) | |||||
| 3. | Gladiola et al | Prospective | 86 | 8.5 years | Males (76%) | Home (72.09%) | Blunt trauma (54.65%) |
| Observational | Females (26%) | Penetrating injuries (20.93%) | |||||
| 4. | Singh et al | Prospective | 220 | 8.74 ± 3.93 years | Males (68.63 %) Females (31.36 %) |
NA | Blunt trauma (29.54 %) |
| Interventional | Metallic/Sharp (14.09 %) | ||||||
| 5. | Martina M et al | Prospective | 96 | 7.3 years | Males (73%) | *Home (≈20 %) | Blunt trauma (34.1 %) |
| Observational | Females (27%) | Others (≈80%) | Metallic/Sharp (22.8 %) | ||||
| 6. | Madan et al | Prospective | 61 | 8.33 ± 4.03 years. | Males (62.3%) | NA | Sports related (29.5%) |
| Observational | Females (37.7%) | Wooden stick (22.9%) | |||||
| Firecracker (18%) | |||||||
| 7. | Pardhi et al | Prospective | 79 (94 Eyes) | NA | Males (57%) | NA | Projectile objects (20%) |
| Interventional | Females (43%) | Sports (16%) | |||||
| Accidental falls (15%) | |||||||
| Blunt objects (14%) | |||||||
| 8. | Aldous et al | Prospective | 160 | 9.59 ± 4.92 years | Males (100 %) | Home (5 %) | Toy Gun/ Blunt (86.9%) |
| Observational | Females (00 %) | Outside Home (95%) | Fireworks (11.2%) | ||||
| 9. | Puodziuviene et al. | Retrospective | 268 | 10.7 ± 4.6 years | Males (79.4 %) | Home (60.4 %) | Blunt trauma (40.3 %) |
| Observational | Females (20.6 %) | Outside Home (39.6 %) | Metallic/Sharp (29.9 %) | ||||
| 10. | S. Qayum et al | Retrospective | 357 | 8.36 years | Males (74.8 %) | Home (48 %) | Blunt trauma (max in CGI) |
| Observational | Females (25.2 %) | Outside Home (52 %) | Metallic/Sharp (max in OGI) | ||||
| 11. | Bucan et al | Retrospective | 353 | 10.5 years | Males (82 %) | Home (17 %) | NA |
| Observational | Females (18 %) | Outside Home (83 %) | |||||
| 12. | Y Liu et al | Retrospective | 295 (295 Eyes) | 7.8 ±4.6 years | Males (72 %) | NA | Projectile (36.8%) |
| Observational | Females (28 %) | Struck (20.4%) | |||||
| 13. | Katiyar et al | Retrospective | 191 | 7.6 ± 3.3 years | Males (79.1 %) | Home (21.5 %) | NA |
| Observational | Females (20.9 %) | Outside Home (78.5 %) | |||||
| 14. | C Boret et al | Retrospective | 337 | 8.4 ± 4.1 years | Males (73 %) | Home (51 %) | Blunt trauma (22 %) |
| Observational | Females (27 %) | Outside Home (49 %) | Fall (16%) | ||||
| Projectile (14%) | |||||||
| Metallic/Sharp (7 %) | |||||||
| 15. | V Antonio et al | Retrospective | 61 | 9 years (median) | Males (67.21 %) | Home (26.23 %) | Blows (63.93%) |
| Observational | Females (57.37 %) | Outside Home (32.79 %) | Foreign Body (19.67%) | ||||
| * Calculated on the basis of objects causing injury | |||||||
Table 1: Sociodemographic factors comparison of the selected studies.
Object/Mechanism causing the injury
10 studies out of 15 observed that the most common mode of injury was blunt trauma; meanwhile, Sharp objects were the second most common objects causing injury. Projectiles and stones were also the common modes of injury.
Time of presentation to the hospital
In 4 studies out of 7 which had recorded the data of the time of presentation to the hospital, it was observed that the majority of patients reached within 24 hours, while in 3 studies, it was shown that the major fraction of patients reached after initial 24 hours.
Type of Injury
Closed Globe injury was more in 7 studies out of 14 with an extracted proportion of 45.1 %. While Open Globe Injury's extracted proportion was 39.42 %, it was more encountered (in 8 studies). When it came to the Area involved, the Zone 1 injuries involving Cornea, Hyphema, and Contusion were the most common injuries found in the maximum studies, followed by globe rupture or penetrating injuries (Table 2).
| Sl. No. | Study | Time of Presentation | Type of Injury | Tissue/Area Involved |
|---|---|---|---|---|
| 1. | Shah et al | NA | CGI (41.9%) | Closed globe contusion (68.5%) |
| OGI (59.5%) | Lamellar laceration (31.5%) | |||
| 2. | Ebrahim A et al | Within 24 hours (56%) | CGI (13.75%), | Ruptured globes (30%) |
| After 24 Hours (37.33%) | OGI (83.75%) | Lacerated globes (53.75%) | ||
| 3. | Gladiola et al | NA | NA | NA |
| 4. | Singh et al | Upto 12 Hours (30%) | CGI (32.72%), | Ant. Segment (77.27%) |
| More than 12 Hours (70%) | OGI (67.28%) | Post. Segment (22.73%) | ||
| 5. | Martina M et al | Within 24 Hours (61.6%) | CGI (83.2 %), | NA |
| Within first 12 Hours (40.6%) | OGI (9.6%) | |||
| 6. | Madan et al | Within 6 h (11.5%) | CGI (24.6 %), | Zone 1 (78.7%) |
| Between 6 and 24 h (32.8%) | OGI (63.9%) | Zone 2 (6.6%) | ||
| 24 h after injury (55.7%) | Zone 3 (14.8%) | |||
| 7. | Pardhi et al | Within 1 hour (25%) | CGI (41 %) | Eyelid (51 %) |
| Between 1–24 hours (61%) | OGI (59 %) | Conjunctival (16%) | ||
| After 24 hours (14%) | Cornea (15%) | |||
| 8. | Aldous et al | NA | OGI ( maximum) | Hyphema (78.75 %) |
| Ruptured globe (10.00 %) | ||||
| Corneal abrasion (3.13 %) | ||||
| Limbal ischemia (1.88 %) | ||||
| 9. | Puodziuviene et al. | During the first 24 hours (64.9%) | CGI (53.4 %), | Zone I (73.7%), |
| In the first 45 hours (22.8%) | OGI (28.7 %) | Zone II (15.8%) | ||
| Zone III (10.5%) | ||||
| 10. | S. Qayum et al | NA | CGI (67.8 %) | Adnexal (25.5%) |
| OGI (32.2 %) | Sub Conj.Haem.(24.9%) | |||
| Corneal perforation (18.5) | ||||
| Corneal abrasion (17.3%) | ||||
| 11. | Bucan et al | NA | CGI (84.7 %), | Contusion (79 %) |
| OGI (15.3 %) | Penetration (13.6%) | |||
| 12. | Y Liu et al | NA | CGI (22.7 %), | Zone I (46.1 %), |
| OGI (26.4 %) | Zone II (31.7 %) | |||
| Zone III (22.03 %) | ||||
| 13. | Katiyar et al | 27.6 ± 37.9 hours | CGI (30.9 %), | Corneoscleral laceration (48.2%) |
| OGI (69.1 %) | Globe rupture (12.6%) | |||
| 14. | C Boret et al | NA | CGI (77.5 %), | Hyphema (22%) |
| OGI (22.5 %) | Not specified (24%) | |||
| 15. | V Antono et al | NA | CGI (57.37 %), | Contusion (36.06%) |
| OGI (14.75 %) | Lamellar laceration (21.31%) | |||
| Eyelid (16.39%) |
Table 2: Comparison of ocular injury characteristics and features.
Conclusion
It was concluded that men suffered more ocular trauma than women in the majority of studies, and that home was the most common site of trauma, followed by outside the home. Regarding the kind of trauma, the papers chosen for review most frequently reported blunt and projectile object trauma. The majority of paediatric trauma patients in the research chosen presented to the hospital within 12 hours, while in some studies they reported even beyond 24 hours.
References
- El-Sebaity DM, Soliman W, Soliman AM, et al. Pediatric eye injuries in upper Egypt. Clin Ophthalmol 2011; 5:1417–1423.
- Acar U, Tok OY, Acar DE, et al. A new ocular trauma score in pediatric penetrating eye injuries. Eye 2011; 25:370–374.
- Poon AS, Ng JS, Lam DS, et al. Epidemiology of severe childhood eye injuries that required hospitalization. Hong Kong Med J 1998; 4:371–374.
- MacEwen C, Baines P, Desai P. Eye injuries in children: The current picture. Br J Ophthalmol 1999; 83:933–936.
- Pizzarello LD. Ocular trauma: Time for action. Ophthalmic Epidemiol 1998; 5:115.
- Ervin-Mulvey LD, Nelson LB, Freeley DA. Pediatric eye trauma. Pediatr Clin North Am 1983; 30:1167–1183.
- Coody D, Banks JM, Yetman RJ, et al. Eye trauma in children: Epidemiology, management, and prevention. J Pediatr Health Care 1997; 11:182–188.
- Singh S, Sharma B, Kumar K, et al. Epidemiology, clinical profile, and factors, predicting the final visual outcome of pediatric ocular trauma in a tertiary eye care center of Central India. Indian J Ophthalmol 2017; 65:1192–1197.
- Qayum S, Anjum R, Rather S. Epidemiological profile of pediatric ocular trauma in a tertiary hospital of northern India. Chinese J Traumatol 2018; 21:100–103.
- Madan AH, Joshi RS, Wadekar PD. Ocular trauma in pediatric age group at a tertiary eye care center in central Maharashtra, India. Clin Ophthalmol 2020;1 4:1003–1009.
- Li C, Lin Y, Xiao H, et al. Epidemiology of pediatric eye injuries requiring hospitalization in rural areas of Wenzhou and Changsha, China: A 10-year retrospective study. BMC Ophthalmol 2020; 20:100.
- Kuhn F, Morris R, Witherspoon CD. Birmingham eye trauma terminology (BETT): Terminology and classification of mechanical eye injuries. Ophthalmol Clin North Am 2002; 15:139–43.
- Bućan K, Matas A, Lovrić JM, et al. Epidemiology of ocular trauma in children requiring hospital admission: A 16–year retrospective cohort study. J Glob Health 2017; 7:010415.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Fahad Mohammed Albaqami1*, Muhanad Althbaiti1, Abdulrahman Albugami1, Abdulsalam Alshehri1, Ahmed Salah Saleh Alosaimi1, Majed Mohammed Albaqami2 and Abdulhamid Alghamdi3
1Medical Student, College Of Medicine, Taif University, Taif, Saudi Arabia2General Physician, Ministry of Defence, Taif, Saudi Arabia
3Department of Ophthalmology, College of Medicine, Taif University, Taif, Saudi Arabia
Citation: Fahad Mohammed Albaqami, Muhanad Althbaiti, Abdulrahman Albugami, Abdulsalam Alshehri, Majed Mohammed Albaqami, Ahmed Salah Saleh Alosaimi, Abdulhamid Alghamdi, Muath Alotaibi, Waleed Khalid Alrabie, Majed Mohammed Albaqami, Bader Saleh Almutairi, Hamoud Abdulmohsen Alobaylan, Faisal Alharthi, Talal Althomali, Clinico-Epidemiological Characterization of Paediatric Ocular Trauma: A Systematic Review, J Res Med Dent Sci, 2022, 10 (8):05-09.
Received: 27-Jul-2022, Manuscript No. JRMDS-22-70453; , Pre QC No. JRMDS-22-70453 (PQ); Editor assigned: 29-Jul-2022, Pre QC No. JRMDS-22-70453 (PQ); Reviewed: 12-Aug-2022, QC No. JRMDS-22-70453; Revised: 18-Aug-2022, Manuscript No. JRMDS-22-70453 (R); Published: 25-Aug-2022
