Case Report - (2025) Volume 13, Issue 1
Clinical Management of Condensing Osteitis: A Case Report
*Correspondence: Reema A Sharaf, Department of Restorative Dentistry, Prince Sultan Medical Military City, Riyadh, Saudi Arabia, Email:
Abstract
An area of increased bone density characterizes condensing osteitis, also known as focal sclerosing osteomyelitis, a condition most commonly involving the mandible and typically resulting from chronic inflammation or infection. This lesion appears as a localized radiopaque area on radiographic images, typically in the periapical region (around the root of a tooth). In the present case report, we are reporting a case of condensing osteitis in a 57-year-old female who came to our dental clinic with sudden pain and bony swelling in the lower right side of the mandible. We have discussed the management and follow-up of the case.
Keywords
Osteitis, Osteomyelitis, Inflammation, Endodontic, Case report
Introduction
Chronic focal sclerosing osteitis is a localized, asymptomatic, radiopaque lesion of the jaw [1]. The condition is characterized by bone growth, which is caused by a mild infection of the pulp tissues. Condensing osteitis and sclerosing osteitis are synonyms for chronic focal sclerosing osteitis [2]. Low-virulence microorganisms in the residual necrotic pulp induce a bone response, causing chronic and mild irritation to the root canal and condensing osteitis [3]. They are more common in the jaw area and are typically discovered during regular dental radiograph examinations. The prevalence of condensing osteitis is about 4-7%. The mandibular region has a 91% prevalence of condensing osteitis, while the maxillary region has a 9% prevalence [4]. Condensing osteitis most commonly occurs in the mandibular first molar region, and it is more common in females.
The radiographic feature of condensing osteitis consists of a well-defined, localized, radio opaque area near the root of the tooth. The lesion is usually not associated with bone expansion or destruction but rather shows a dense sclerotic, hard bony appearance. Unlike more destructive forms of osteomyelitis, condensing osteitis is not characterized by bone loss but by bone formation in response to inflammation [5]. The lamina dura is lost and the periodontal ligament space widens [3]. These lesions generally are seen at the apex of a tooth with deep caries or large restorations, a crown or bridge, periodontal disease, and root canal therapy [1].
Histologically, in condensed osteitis, the bone's ability to remodel is slowed down because normal bone marrow is replaced with fibrous connective tissue. In some cases, inflammatory cells may also be present [4]. People with high tissue resistance are more likely to have condensed osteitis, which is when dense trabeculae form in the bone marrow spaces. These trabeculae look like compact bone [1]. Condensing osteitis occurs as a result of the defense mechanisms of the bone tissues against chronic pulpal inflammation or periapical infection. There are a few radiopaque jaw lesions where there is increased deposition of jaw bone, which can get confused with condensing osteitis. Differential diagnosis for condensing osteitis includes idiopathic osteosclerosis and cementoblastomas [1,5].
The diagnosis of condensing osteitis is primarily based on radiographic findings along with clinical correlation. Dentists typically identify it on periapical X-rays during routine exams. The lesion’s dense, localized sclerotic appearance differentiates it from other conditions, like periapical abscesses, which usually show radiolucency (dark areas indicating bone loss) [5].
Usually the involved tooth is non-vital or with reduced vitality, and there may also be a history of chronic dental infection or dental inflammation [5].
If pulpitis or tooth infection is the cause of condensing osteitis and the tooth is restorable, endodontic treatment is necessary to eliminate the source of inflammation. In severe cases, or when the tooth is non-restorable, extraction would be the treatment of choice [5]. Monitoring in some cases of condensing osteitis would be another choice of treatment, and the sclerotic area may remain stable over time without the need for any intervention. Regular radiographic monitoring is important to track changes in the lesion.
Condensing osteitis typically has a good prognosis, especially when the underlying cause, such as a dental infection, receives prompt treatment. Even after the infection resolves, the sclerotic bone may persist, but it typically poses no further health risks [5].
Case Report
A 57-year-old Saudi female came to our clinic at the department of restorative dentistry. She presented with complaints of pain and hard swelling in the lower right side of the mandible, specifically in tooth number 46. The patient has been diagnosed with lichen planus erosive type, and she is currently not taking any medications. Symptoms started two months ago; pain rises with biting and chewing. The swelling of the hard buccal bones is associated with the symptoms. No medications have been taken. A clinical examination was conducted, which revealed hard swelling both extra-orally and intra-orally, as well as desquamative gingivitis near areas 44 and 45. The buccal mucosa exhibits bilateral white reticulation without any associated ulcers or erosions. There is a Porcelain Fused to Metal crown (PFM), which is in good condition. The tender on percussion was positive for case number 46, but it was negative for cases numbers 45 and 47.
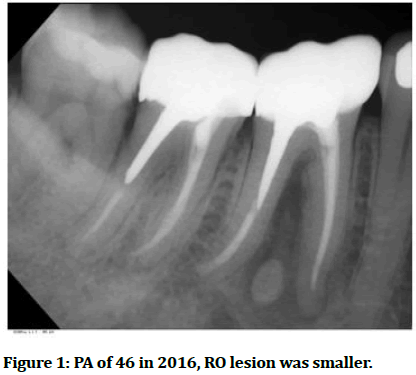
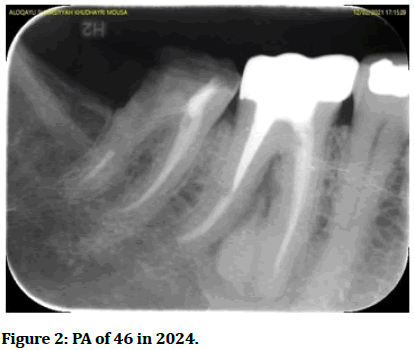
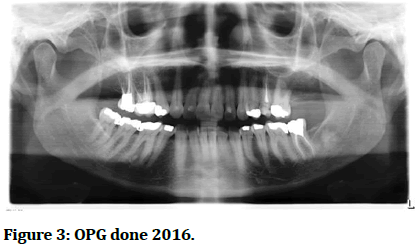
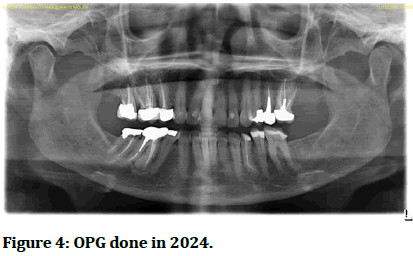
Investigations, including OPG and PA radiographs, reveal adequate root canal filling material, along with a post in the distal canal. There is a well-defined radio opaque lesion near the mesial root of 46 with radio-lucent rimming. The results of the CBCT were similar to those of the OPG, indicating a mild buccal expansion associated with 46 (Figures 1-4).
Consultations have been done and it has been explained that no treatment can be done at this moment, but we need to do closer follow-up in the clinic regularly with associated radiographs. It has been explained to her.
Figure 1: PA of 46 in 2016, RO lesion was smaller.
Figure 2: PA of 46 in 2024.
Figure 3: OPG done 2016.
Figure 4: OPG done in 2024.
Discussion
Chronic focal sclerosing osteitis is a localized, asymptomatic, radio-opaque lesion of the jaw [1]. It is characterized by bone growth, which is due to a mild infection of the pulp. Condensing osteitis and sclerosing osteitis are synonyms for chronic focal sclerosing osteitis [2]. Low-virulence microorganisms in the residual necrotic pulp cause chronic and mild irritation to the root canal, which in turn induces a bone response [3]. They are more common in the jaw area and are typically discovered during regular dental radio graph examinations.
The involved tooth is usually associated with a longstanding pulpal infection and occurs as a result of the body's defence mechanism against the infection [6]. When diagnosing a condensing osteitis lesion, one should also consider idiopathic sclerosis, a periapical radiopaque lesion [7]. Because there are a lot of cavities and big fillings in the lower jaw molars, which can get pulpitis and pulp necrosis, the lower jaw's first molar is most likely to get condensing osteitis. The lower jaw's second molar comes in second [8].
The management of condensed osteitis depends on the condition of the affected tooth. Usually, with proper endodontic treatment, the condition will subside or decrease in size. However, if the lesion is the result of inadequate root canal treatment, it will not go away [1]. Condensing osteitis has a good prognosis because it can be successfully treated with appropriate endodontic procedures, and healing can include total regression of the sclerotic bone and inflammation.
Conclusion
In the current case, a long-standing carious tooth had a condensing osteitis lesion, which we treated with proper root canal therapy, a post, and a well-sealed crown. The lesion did not show any changes in size for the last two years. When the patient presented with symptoms during the follow-up visit, the recommended treatment was to extract the involved tooth and surgically remove the lesion, but she chose to wait and follow up instead.
References
- Yeh HW, Chen CY, Chen PH, et al. Frequency and distribution of mandibular condensing osteitis lesions in a Taiwanese population. J Dent Sci 2015; 10:291-295.
- Holly D, Jurkovic R, Mracna J. Condensing osteitis in oral region. Bratisl Lek Listy 2009; 110:713-715.
[Google Scholar] [PubMed]
- Dukic W, Filipovic-Zore I, Bago I. Condensing osteitis-case report. Acta Stomatol Croat 2006; 40:182-188.
- Jacobsson S. Diffuse sclerosing osteomyelitis of the mandible. Int J Oral Surg 1984; 13:363-385.
[Crossref] [Google Scholar] [PubMed]
- Gupta, Sonal, Shilpi Dutta, et al. Condensing osteitis-A Review and Case Report. 2023.
- Elfenbaum A. Condensing osteitis in the dental x-ray. Dent Dig 1967; 73:554-558.
[Google Scholar] [PubMed]
- Kawai T, Hirakuma H, Murakami S, et al. Radiographic investigation ofidiopathic osteosclerosis of the jaws in Japanese dental outpatients. Oral Surg Oral Med Oral Pathol 1992; 74:237-242.
[Crossref] [Google Scholar] [PubMed]
- Williams TP, Brooks SL. A longitudinal study of idiopathic osteosclerosis and condensing osteitis. Dentomaxillofac Radiol 1998; 27:275-278.
[Crossref] [Google Scholar] [PubMed]
Author Info
Department of Restorative Dentistry, Prince Sultan Medical Military City, Riyadh, Saudi ArabiaReceived: 14-Jun-2024, Manuscript No. JRMDS-24-138968; , Pre QC No. JRMDS-24-138968 (PQ); Editor assigned: 17-Jun-2024, Pre QC No. JRMDS-24-138968 (PQ); Reviewed: 01-Jul-2024, QC No. JRMDS-24-138968; Revised: 27-Dec-2024, Manuscript No. JRMDS-24-138968 (R); Published: 03-Jan-2025