Research - (2021) Volume 9, Issue 6
Clinical Case Study ON Incidence and Management of Varicose Veins
R Sachin Raj, RNM Francis and P Sasikumar*
*Correspondence: P Sasikumar, Department of General Surgery, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, India, Email:
Abstract
Varicose veins are tortuous, widened veins in the subcutaneous tissues of the legs and are often easily visible. Their valves are usually incompetent so that reflux of blood occurs, and the resulting venous hypertension can cause symptoms. Varicose veins are widely seen as medically unimportant and deserving low priority for treatment. They are common, affecting nearly a third of adults in Western societies, and few people with varicose veins are ever harmed by them. However, they cause concern and distress on a large scale, most of which can be dealt with by good explanation and reassurance, or by a variety of treatments which are evolving rapidly at present. Patients can now be referred for more precise assessment and a greater range of therapeutic options than ever before. To study the various clinical presentations, complications of varicose veins and various modalities of management and outcome of various modalities of management.
Keywords
Varicose veins, Venous hypertension, Concern, Distress
Introduction
The term varicose is derived from latin word varix meaning ‘bent’. Varicose limb which has lost its valvular efficiency and as a product of the resultant venous hypertension in standing position becomes dilated, tortuous, elongated, and thickened. Varicose veins are known from antiquity since Hippocrates and treatment in its length and associated with varicose ulcer. Varicose veins of the lower limb are the most common vascular disorder affecting the human beings [1]. It is almost certainly the price we pay for the erect posture. Nowadays we have various options are available for treating varicose veins. Our renewed interest in the incidence and management of varicose veins has prompted a reappraisal of its basic components and how they are individually affected by biological, mechanical, and physical forces [2,3]. The goal of varicose veins management is safe and easy manipulation of the healing process we are closer to that goal than ever before.
Materials and Methods
This is a prospective clinical study of 100 cases of varicose veins and to assess the management and outcomes, during the period from March 2017 to October 2018 in our Department of General Surgery, Sree Balaji Medical College and Hospital.
All the cases underwent detailed evaluation regarding presenting symptoms, duration, and previous modality of treatment. Clinical examination was made as to which system was involved and to identify which superficial valves and perforators were incompetent. Deep vein patency was assessed. Abdominal and pelvic examinations were made to rule out secondary causes. Cardiovascular and peripheral pulses were assessed to exclude arterial disease.
Routine investigations and selective doppler assessment were done. Documentation was done using a stratified proforma which included demographic data of the patients studied; all the details of investigations carried out and the types of management provided to the patients enrolled in the study.
For all patients, haematological, biochemical, microbiological, and radiological investigations were carried out as enumerated in the proforma using standard procedures.
Inclusion criteria
All cases of varicose veins including Outpatients and inpatients in SBMCH between the period from MARCH 2017–OCTOBER 2018.
Exclusion criteria
All the patients with Varicose veins leaving the hospital before the treatment is complete.
Results
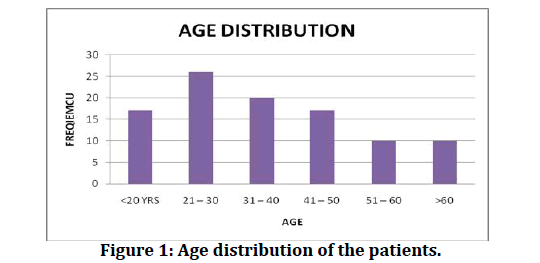
Among the study population, a majority of 26 % constituted between the age group 21–30 years followed by 20% between the age group 31–40 years, 17% between the age group 41- 50 years and less than 20 years, 10 % between the age group 51–60 & above 60 years (Table 1 and Figure 1). The study population was distributed as 62 % of males and 38 % as females (Table 2 and Figure 2).
Figure 1: Age distribution of the patients.
Figure 2: Gender distribution.
| Age | No of cases | Percentage |
|---|---|---|
| <20 YRS | 17 | 17 |
| 21 – 30 | 26 | 26 |
| 31 – 40 | 20 | 20 |
| 41 – 50 | 17 | 17 |
| 51 – 60 | 10 | 10 |
| >60 | 10 | 10 |
| Total | 100 | 100 |
Table 1: Age distribution of the patients.
| Sex | No of cases | Percentage |
|---|---|---|
| Male | 62 | 62 |
| Female | 38 | 38 |
| Total | 100 | 100 |
Table 2: Gender distribution.
Most of the people presented with symptoms persists more than 2 years before they seeked the medical attention.12% presented with in six months duration andanother 21% took for about at least 2 yrs. to medical consultation. Those who took 2 -5 yrs. constituted 28%those who took more than 5 yrs. constituted 13%. Time duration for the presentation between 3 months minimum and 20 years maximum (Table 3).
| Presentation | No of cases | Percentage |
|---|---|---|
| <6 months | 12 | 12 |
| 6 months– 2 yrs | 21 | 21 |
| 2 yrs– 5 yrs | 28 | 28 |
| 5 yrs – 8 yrs | 13 | 13 |
| 8 yrs – 10 yrs | 14 | 14 |
| >10 yrs | 12 | 12 |
| Total | 100 | 100 |
Table 3: Mean duration of presentation.
Manual labourer formed the largest proportion around 16%. Pregnant women and doctors formed 10% each. Those who stood for prolonged periods constitute students, salesmen, security & others which formed 64% (Table 4). Among the total women patients 26% (10 cases) were pregnant women (Table 5).
| Occupation | No of cases | Percentage |
|---|---|---|
| Manual working | 16 | 16 |
| Pregnant women | 10 | 10 |
| Doctors | 10 | 10 |
| Students | 14 | 14 |
| Salesmen | 14 | 14 |
| Security | 13 | 13 |
| Others | 23 | 23 |
| Total | 100 | 100 |
Table 4: Various occupations of the patients.
| Women | No of cases |
|---|---|
| Pregnant women | 10 |
| Total women | 38 |
Table 5: Ratio of pregnant women among the women patients.
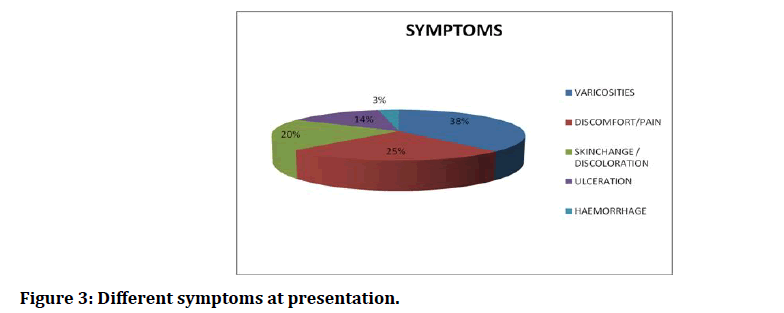
38% of the study population had symptoms related primarily to the dilated varicose veins.25% had discomfort or pain. Symptoms due to skin change and discolouration, ulceration and haemorrhage was presented with 20%, 14% and 3% respectively (Table 6 and Figure 3).
Figure 3: Different symptoms at presentation.
| Symptom | No of cases | Percentage |
|---|---|---|
| Varicosities | 38 | 38 |
| Discomfort/pain | 25 | 25 |
| Skin change/discoloration | 20 | 20 |
| Ulceration | 14 | 14 |
| Hemorrhage | 3 | 3 |
| Total | 100 | 100 |
Table 6: Different symptoms at presentation.
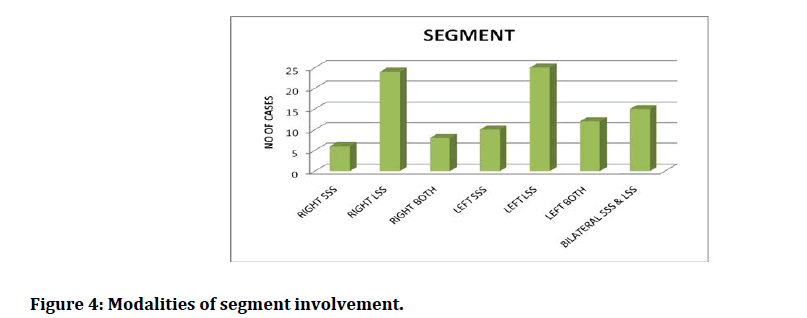
LSS was commonly involved around 49% and short saphenous around 16% while both in left and right constituted 8% and 12% respectively. Left sided lesions constituted 47% and right-sided lesions constituted only 38%. Bilateral made around 15% (Table 7 and Figure 4).
Figure 4: Modalities of segment involvement.
| Side | Segment | No of cases | Percentage |
|---|---|---|---|
| Right | SSS | 6 | 6 |
| LSS | 24 | 24 | |
| Both | 8 | 8 | |
| Left | SSS | 10 | 10 |
| LSS | 25 | 25 | |
| Both | 12 | 12 | |
| Bilateral | SSS & LSS | 15 | 15 |
| Total | 100 | 100 |
Table 7: Modalities of segment involvement.
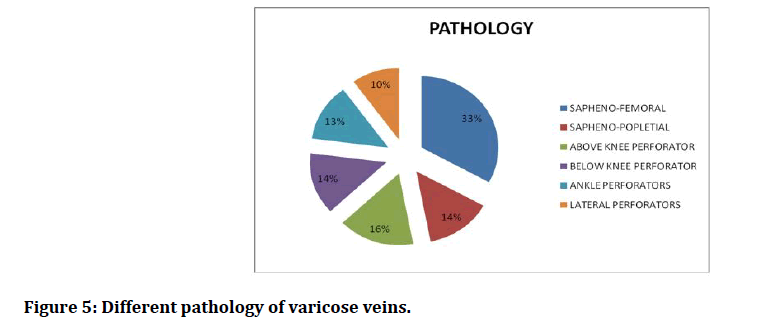
Sapheno-femoral incompetence constituted the bulk of the disease339 % of the present study. Sapheno-popletial incompetence & below knee perforator incompetence occurred each in %. Above knee perforator incompetence occurred in 16%. %. Ankle perforators incompetence was least common only in 13%. Lateral perforator incompetence was common in 1% (Table 8 and Figure 5).
Figure 5: Different pathology of varicose veins.
| Pathology | No of cases | Percentage |
|---|---|---|
| Sapheno- femoral incompetence | 33 | 33 |
| Sapheno- popletial incompetence | 14 | 14 |
| Above knee perforator | 16 | 16 |
| Below knee perforator | 14 | 14 |
| Ankle perforators | 13 | 13 |
| Lateral perforators | 10 | 10 |
| Total | 100 | 100 |
Table 8: Different pathology of varicose veins.
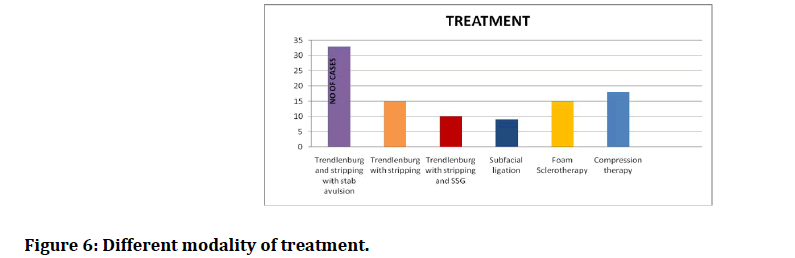
Trendlenburg and stripping with stab avulsion constitutes 33%, trendlenburg and stripping with constitutes 15% whereas trendlenburg with stripping and SSG is done in 20%. Subfascial ligation procedure is done in 9%. Foam sclerotherapy and compression therapy is done in 15% and 18% respectively (Table 9 and Figure 6).
Figure 6: Different modality of treatment.
| Treatment | No of cases | Percentage |
|---|---|---|
| Trendlenburg and stripping with stab | 33 | 33 |
| avulsion | ||
| Trendlenburg with stripping | 15 | 15 |
| Trendlenburg with stripping and SSG | 10 | 10 |
| Subfascial ligation | 9 | 9 |
| Foam Sclerotherapy | 15 | 15 |
| Compression therapy | 18 | 18 |
| Total | 100 | 100 |
Table 9: Different modality of treatment.
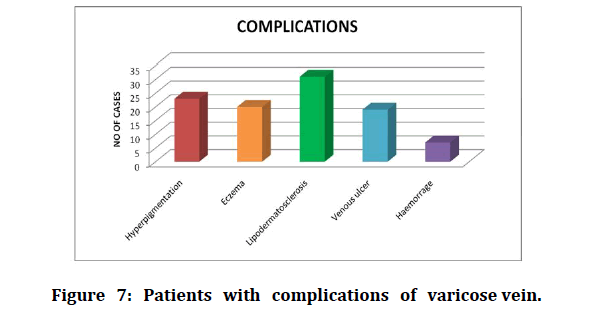
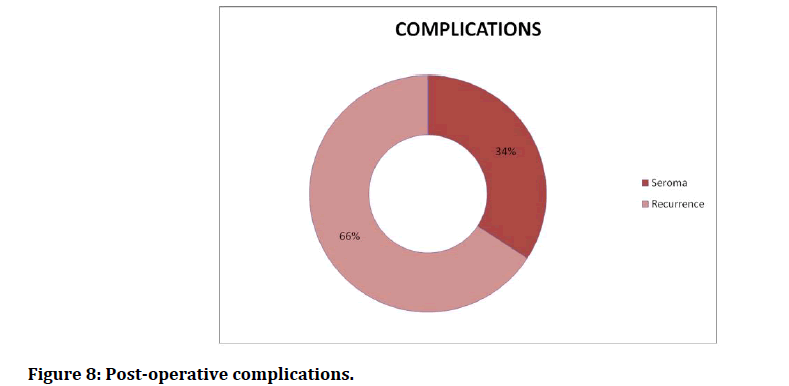
Among the total cases 23 % had hyperpigmentation, 20 % had eczema, 31 % had Lipodermatosclerosis, 19 % had venous ulcer and 7 & had haemorrhage (Table 10 and Figure 7). Among the 100 cases, 41 patients had complications out of which 34 % had seroma and 66%had recurrence (Table 11 and Figure 8).
Figure 7: Patients with complications of varicose vein.
Figure 8: Post-operative complications.
| Complications | No of cases | Percentage |
|---|---|---|
| Hyperpigmentation | 23 | 23 |
| Eczema | 20 | 20 |
| Lipodermatosclerosis | 31 | 31 |
| Venous ulcer | 19 | 19 |
| Hemorrhage | 7 | 7 |
| Total | 100 | 100 |
Table 10: Patients with complications of varicose vein.
| Complications | no of cases | Percentage |
|---|---|---|
| Seroma | 14 | 34 |
| Recurrence | 27 | 66 |
| Total | 41 | 100 |
Table 11: Post-operative complications.
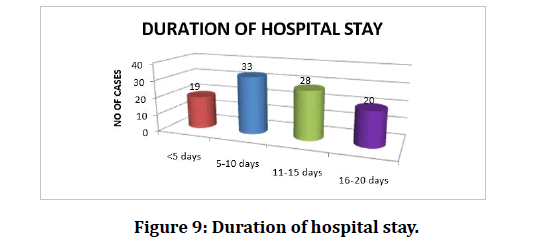
33 % of the people stayed mean duration 5 -10 days in hospital. 28% people stayed for the duration about 11-15 days. 20% people sxdtayed for the duration about 16-20 days in the hospital and 19 people stayed for less than 5 days in the hospital. Minimum 4 days maximum 19 days is duration of hospital stay for the patient (Table 12 and Figure 9).
Figure 9: Duration of hospital stay
| Duration of hospital stay | No of cases | Percentage |
|---|---|---|
| <5 days | 19 | 14 |
| 5-10 days | 33 | 29 |
| 11- 15 days | 28 | 28 |
| 16- 20 days | 20 | 15 |
| TOTAL | 100 | 100 |
Table 12: Duration of hospital stay.
Discussion
This study was conducted among 100 patients with varicose veins of Sree Balaji Medical College and Hospital between March 2017 and October 2018 for a period of 18 months. According to Evans CJ, FowkesFGR, Male and female ratio constitutes for about 1:2, Males constitute 62 % of our study and females 38 %. Male:female ratio 1.6:17.The age group which affects predominately economically productive people between 20 to 40 yrs. Mean age of presentation is around 2 years. 12 patients less than six months and longest duration are more than 10 years. Varicose vein being a benign disorder hence people do not seek medical attention early except for haemorrhagic varicose veins. Manual worker constitutes 16% of our study. Occupations like manual labourer, salesman, farmers, security guards constitute around 50%. 38% of the people seek medical attention due to varicosities and one fourth of patient complaints discomfort or pain. Ulceration and haemorrhage were about 14 % and 3 %respectively, In my study Left sided lesions were more common than right side. Varicosities is the most common presenting symptom. Long saphenous segment is more common than short saphenous segment. Both systems were involved in 15% of people.Sapheno-femoral incompetence is the most observed pathology. Of the perforators below knee perforator is commonly involved and lateral perforator least. Trendlenburg procedure with stripping and stab avulsion with subfacial ligation of perforation was most done.
SSG combined with the above procedure was done in 10% of the patients. Lipodermatosclerosis was the common complication. Hyperpigmentation was seen in 23 % of patients. 19 % of the patients presented with venous ulcers. Eczema was seen in 10 % of patients and 5% of the patients presented with haemorrhage. Meanhospital stay was 11 days. Minimum stay in the hospital was 4 days and the maximum was 19 days [4-35].
Conclusion
In my study Varicose veins was relatively common among the youth and middle age groups. Risk factors for the development of varicose veins were prolonged standing and multiparity. Clinical presentations ranged from mild to severe varicosities, with ulcer and Lipodermatosclerosis being the most severe forms. At present, Duplex ultrasound scanning is the most reliable investigative tool in making diagnosis of varicose veins in terms of valve incompetence along GSV and SSV, deep vein thrombosis and perforator incompetence. Treatment includes conservative management, sclerotherapy, and surgery. Conservative management was advised in patients who are pregnant and patients with contra indications for surgery. These patients were advised to wear compression stockings. Sclerotherapy was advised in patients with reticular veins. Surgical procedure includes Trendlenburg procedure, stripping of the vein and sub facial ligation of the perforators. Surgical intervention has been revolutionized by the development of endovenous techniques like radiofrequency abalation, laserabalation, foam sclerotherapy and sub facial endoscopic perforator surgery.
Funding
No funding sources.
Ethical Approval
The study was approved by the Institutional Ethics Committee.
Conflict of Interest
The authors declare no conflict of interest.
Acknowledgements
The encouragement and support from Bharath University, Chennai is gratefully acknowledged. For provided the laboratory facilities to carry out the research work.
References
- Laing W. Chronic venous diseases of the leg. London: OYce of Health Economics, 1992; 1–44.
- Evans CJ, Fowkes FGR, Hajivassiliou CA, et al. Epidemiology of varicose veins-A review. Int Angiol 1994; 1.
- Stanhope JM. Varicose veins in a population of New Guinea. Int J Epidemiol 1975; 4:221-225.
- Da Silva A, Widmer LK, Martin H, etal. Varicose veins and chronicvenous insuffciency-prevalence and risk factors in 4376 subjects of the Basle Study II. Vasa 1974; 3:118–25.
- Callam MJ, Harper DR, Dale JJ, et al. Chronic ulcer of the leg: Clinical history. Br Med J 1987; 294:1389 –1391.
- Alexander House Group. Consensus paper on venous leg ulcers. Phlebology 1992; 7:48–58.
- Mirji P, Emmi S, Joshi C. Study of clinical features and management of varicose vein. J Clin Diagnostic Res 2011; 5:1416 -1420.
- Lateef MA. Clinical pathological study of primary varicose vein in the lower limb. Br J Surg 1995; 82:855-856.
- De Backer G. Epidemiology of chronic venous insufficiency. Angiology 1997; 48:569-576.
- Al-Mulhim AS, El-Hoseiny H, Al-Mulhim FM, et al. Surgical correction of main stem reflux in the superficial venous system: Does it improve the blood flow of incompetent perforating veins?. World J Surg 2003; 27:793-796.
- Dur AHM, Mackaay AJC. Duplex assessment of clinically diagnosed venous insufficiency. Br J Surg 1992; 79:155-161.
- Mofidi R, Bello AO, Mofidi A, et al. Feasibility of day case varicose vein surgery in a district general hospital. Irish J Med Sci 2000; 169:37-39.
- Cambell WB. Varicose vein, an increasing burden for the NHS. Br Med J 1990; 300:7634.
- Smith PC, Thomas PS, Scurr JH, et al. Causes of venous ulceration: A new hypothesis. Br Med J 1988; 296:1726-7.
- Baiely. Short practice of surgery-Venous disorders 24th Edn. Marc Christopher Winslet 2005; 960-62.
- Murad MH, Coto-Yglesias F, Zumaeta-Garcia M, et al. A systematic review and meta-analysis of the treatments of varicose veins. J Vas Surg 2011; 53:49S-65S.
- Lee AJ, Evans CJ, Allan PL, et al. Lifestyle factors and the risk of varicose veins. J Clin Epidemiol 2003; 56:171-179.
- Campbell WB, Decaluwe H, MacIntyre J, et al. Most patents with varicose veins have fears or concerns about the future, in addition to their presenting symptoms. Eur J Vasc Endovasc Surg 2006; 31:332-334.
- Bradbury A, Evans C, Allan P, et al. What are the symptoms of varicose veins? Edinburgh vein study cross sectional population survey. BMJ 1999; 318:353-36.
- Chengelis DL, Bendick PJ, Glover JL, et al. Progression of superficial venous thrombosis to deep vein thrombosis. J Vasc Surg 1996; 24:745-749.
- Caggiati A, Bergan JJ, Gloviczki P, et al. Nomenclature of the veins of the lower limbs: An international interdisciplinary consensus statement. J Vasc Surg 2002; 36:416-422.
- Rautio T, Ohinmaa A, Perala J, et al. Endovenous obliteration versus conventional stripping operation in the treatment of primary varicose veins: A randomised controlled trial with comparison of the costs. J Vasc Surg 2002; 53:958-65.
- Merchant RF, DePalma RG, Kabnick LS. Endovascular obliteration of saphenous reflux: A multicenter study. J Vasc Surg 2002; 35: 1190-6.
- Niclini PH. Treatment of primary varicose veins by endovenous obliteration with the VNUS closure system: Results of a multicentre study. Eur J VascEndovasc Surg 2005; 29:433-439.
- Min RJ, Khilnani N, Zimmet SE. Endovenous laser treatment of saphenous vein reflux: Long term results. J Vasc Interv Radiol 2003; 14:991-996.
- Mundy L, Merlin TL, Fitridge RA, et al. Systematic review of endovenous laser treatment for varicose veins. Br J Surg 2005; 92:1189-94.
- Hobbs JT. Surgery and sclerotherapy in the treatment of varicose veins. Arch Surg 1974; 109:793-796.
- Bountouroglou DG, Azzam M, Kakkos SK, et al. Ultrasound-guided foam sclerotherapy combined with sapheno-femoral ligation compared to surgical treatment of varicose veins: early results of a randomised controlled clinical trial. Eur J VascEndovasc Surg 2006; 31:93-100.
- Cabrera J, Cabrera J, Garcia-Olmedo MA. Treatment of varicose long saphenous veins with sclerosant in microfoam form: Long-term outcomes. Phlebology 2000; 15:19-23.
- Forlee MV, Grouden M, Moore DJ, et al. Stroke after varicose vein foam injection sclerotherapy. J Vasc Surg 2006; 43:162-164.
- Campbell WB, Kumar AV, Collin TW, et al. The outcome of varicose vein surgery at 10 years: Clinical findings, symptoms and patient satisfaction. Ann R CollSurg Engl 2003; 85:52-57.
- Bradbury A, Evans C, Allan P, et al. What are the symptoms of varicose veins? Edinburgh vein study cross sectional population survey. BMJ 1999; 318:353-356.
- Ruckley CV. Socio-economic impact of chronic venous insufficiency and leg ulcers. Angiology 1997; 48:67-69.
- Nicolaides AN. The investigation of chronic venous disorders: A consensus statement. Circulation 2000; 102:126-63.
- Coon WW, Willis PW, Keller JB. Venous thromboembolism and other venous disease in the tecumseh community health study. Circulation 1973; 48:839-846.
Author Info
R Sachin Raj, RNM Francis and P Sasikumar*
Department of General Surgery, Sree Balaji Medical College & Hospital Affiliated to Bharath Institute of Higher Education and Research, Chennai, Tamil Nadu, IndiaCitation: R Sachin Raj, RNM Francis, P Sasikumar, Clinical Case Study ON Incidence and Management of Varicose Veins, J Res Med Dent Sci, 2021, 9(6): 36-46
Received: 02-Mar-2021 Accepted: 09-Jun-2021 Published: 16-Jun-2021