Research - (2021) Volume 9, Issue 8
Clinical Assessment of Cardiopulmonary Changes that Occurs During Dental Work for the Dentist with PPE during COVID-19 Pandemic in Mosul City
Abdulhameed N Aldabagh, Ziad H Deleme* and Alyaa I Naser
*Correspondence: Ziad H Deleme, Department of oral and maxillofacial surgery, College of Dentistry, University of Mosul, Iraq, Email:
Abstract
During COVID-19 pandemic dental work must be changed to another form and quality and quantity and one of these basic changes is personal protective equipment that may has an effects on physiology of dentist،s body including cardiac and pulmonary and blood oxygenation specially if it is used for long periods and their effects on dental performance and time to dental work and make correct decisions during COVID-19 pandemic in dental centres and poly clinics and clinics. Aims of the study: were to find the changes in the readings of heart rate and blood pressure and oxygen saturation of the dentist whom utilizing personal protective equipment for more than one hour during dental work in the period of COVID-19 pandemic. Materials and Methods: A prospective study done first by choosing many centres and poly clinic and dental clinics in Mosul city that obey the protocol of dental work during COVID-19 pandemic and make a case sheet for the dentist with detailed personal and medical and surgical history, who work more than one hour with PPE continuously and check the blood pressure and pulse rate by digital sphygomonometry and pulse oximeter before wearing PPE and after one hour of his work, dentists volunteers divided in to group 1 whom age less than 35 years and group 2 more than 35 years and compare these data and make analysis. Results and discussion: There was a significant difference in the readings of MAP before and after the study tests for group 1only, and values for pulse rates and oxygenation of red blood cells were observed that there was a significant difference for both groups in which work duration was more than 60 minutes, so wearing the PPE has negligible effects on pulse rate and oxygen saturation but had an effects on blood pressure may be due to stress and psychological factors.
Keywords
Assessment, Cardiopulmonary, Dentist, PPE, COVID -19Introduction
The COVID-19 pandemic affecting whole world population and has resulted a frank death rate and disabilities all over the world. [1] First-line medical staff and sub staff and off course the dentists in the first line or COVID-19 war at high risk of the infection in contrast to the other population. [2] Dentists and oral and maxillofacial specialists are of higher jeopardy of other specialties to obtain the contagion. [3] The main manner of spread and getting infection by aerosols from patient’s mouth and direct touch to patient. [4] For that utilization of personal protective equipment (PPE) to decrease contagion is recommended by the WHO and CDC for all healthcare providers in general. [5,6] Soon after the introduction of surgical masks by Mikulicz, their usage converted to an ordinary repetition for the prerequisite health’s patient and doctor in equal, [7] information now a day reveal that wearing mask is an active non-pharmacologic modality to decrease the blowout of COVID-19 infection. [8] Dentists in the dental clinic are under frank corporeal distress, exhaustion, and even decline of treatment plane and quality of work. Even though significant data is affirming the effects of ambient atmosphere on both psychological and bodily routine work, so the final effect of new gest is changing the new work circumstances with the mask including warmth and wetness formed beneath surgical masks, in addition to the respired CO2 that may also be stuck beneath them, persuading a reduction in red blood cells oxygenation. “Normal blood O2 saturation” is defined as a fractional saturation of 90 to 97.5%, that is equal to an arterial oxygen partial pressure near 13.3 to 13.7 kPa. A small device named “pulse oximeter” that has the ability to identify the oxygen saturation of red blood cells fast, in a precise, and dependable manner. So oxygenated and reduced Hb absorb red and infrared light in a different way. Oxy-hemoglobin absorbs additional infrared light, whereas reduced Hb absorbs more red light. The relation of absorptions at the red and infrared wavelengths is evaluated by oximeter to provide the oxygen saturation of arterial pulsations which makes the basis of the device work [9]. increased HR during wearing a mask may produce an increase of the work of inhalation or muscle stress event [10]. So increased primary and secondary respiratory muscle work due to normal reflex mechanisms that may be responsible for the higher readings of CO in blood [11]. According to the previous mechanisms more venous blood return to heart and increase SV and stabilized blood pressure [12-16]. Measurement of blood pressure for checking the physical integrity of persons is also considering of particular importance [17] collection data of blood pressure (SBP & DBP) which recorded separately and also the age group also subdivided to two main categories as the tonicity of arterial walls quite different between the two age groups under and above 35 years old [18] Mean arterial pressure (MAP) is a prerequisite tool because it is a takes the middling of the arterial pressure over the whole heart cycle, which is estimated as “the diastolic pressure plus one-third of the pulse pressure”. It gives an amount of the average perfusion pressure of the systematic blood flow. MAP is” directly proportional to cardiac output”. For the most working purpose, an approximation to MAP can be obtained by applying the following “simple equation: Mean Arterial Pressure=Diastolic Pressure + (1/3 × Pulse Pressure) Pulse Pressure (mmHg) is the difference between systolic and diastolic blood pressures”. [19]
Materials and Methods
A prospective study had been recorded under number (UoM.Dent/H.14/21) by the research ethics committee in the college of dentistry university of Mosul in 19/1/2021, with randomly selected 50 dentists and oral surgeons and maxillofacial surgeons where included in the study from both sexes, whom employed in many centers and poly clinics and private dental clinics in Mosul city, 24 to 58 years old, Inclusion Criteria: Dentist wearing PPE, no history of systemic diseases or drug taken, no NSAIDs taken at day of examination. Exclusion Criteria: Medically compromised dentist, drug affect blood pressure or pulse rate taken, smokers, not well PPE, refused dentist. Those participants had vital sings within normal values, inhaling fresh apartment air and sitting during the dental work. For estimating whether the age had effects on blood pressure (BP), oxygen saturation of red blood cells (SpO2 and pulse rate (PR), participants grouped in to group 1: over 35 years and group 2: less 35 years. Mask used of disposable type germ-free one-way paper masks (Surgical Disposable 3 Ply Face Masks, YUDA medical company, China) been utilized and the mask wear in position that did not change throughout the work (never under the level of nose). Same digital fingertip oximeter (RoHS, China) was utilized to record the oxygenation of the blood saturation in the research, where the finger probe was applied to the second finger of the right hand (Figure 1) with presence of surgical gloves for sterility [20]. And electronic blood pressure monitor arm style (Microcomputer intelligent, Visionary Biomedicine, China) (Figure 2) where used to record the blood pressure systolic and diastolic by keeping the dentist relax and sitting down, palms up and the wrist band parallel to the heart, intake pipe parallel to arm arteries, wrap the wrist band around the left arm tightly in the opposite direction and paste together, then record the data and mean arterial pressure taken by the equation: Mean Arterial Pressure=Diastolic Pressure + (1/3 × Pulse Pressure) in which the pulse pressure= Systolic Blood Pressure−Diastolic Blood Pressure per mmHg. Volunteers were informed to act in normal behavior during the dental clinic. Research accomplished over a three-month duration extended from December 2020 to March 2021, dental clinic room temperature ranged from 18°C to 20°C, and the moistness from 35% to 40%. So the readings taken before dental work and before wearing the mask, SpO2 and PR and blood pressure data were documented. Later on after first hour, pulse oximetry device and electronic blood pressure monitor were applied again and SpO2 and PR and blood pressure readings were documented again [21]. T-test for statistical analysis done by using SPSS program Version 26. readings were regarded to be statistically significant in the range at p≤0.05.
Figure 1: Electronic blood pressure monitor.
Figure 2: Pulse oximeter.
Results
The average age of study groups was (35.32 years), male dentist to female dentist ratio was 2:1. An over view for comparative results between two groups shown in (Table 1).
| Group | age | pBPs | pBPd | MAP pre | PRp | Spo2p | BPs | BPd | MAP post | PR | Spo2 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 ≤ 35 | 30.48 | 123.96 | 79.2 | 94.12 | 90.32 | 95.96 | 124.76 | 80.6 | 65.88 | 89.2 | 93.96 |
| 2 ≤ 35 | 40.16 | 130.48 | 85.08 | 100.21 | 91.96 | 94.6 | 130.72 | 85.44 | 100.53 | 90.32 | 93.04 |
Table 1: The average values of study for both groups.
At the end of research, we found that it was a statistically significant differences in the MAP before and after the study tests for group 1, while we did not found any difference in the values of MAP before and after the study tests for group 2, (p=0.05) (Figure 3)., When pre-work and post work values for PR comparison, found that there was a statistically significant difference for both groups in which work duration was 60 minutes (p≤0.05) (Figure 4). Once the data for SpO2 of red blood cells were compared, we observed a significant difference between pre-work and post–work readings for both groups (p ≤ 0.05) (Figure 5) (Tables 2 and Table 3).
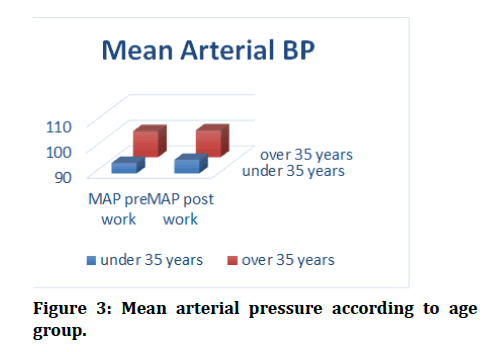
Figure 3: Mean arterial pressure according to age group.
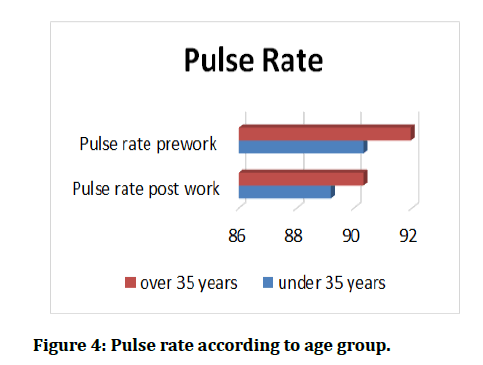
Figure 4: Pulse rate according to age group.
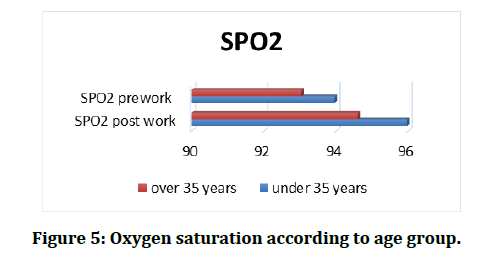
Figure 5: Oxygen saturation according to age group.
| Parameter pair | Correlation | Sig. | Sig. (2-tailed) |
|---|---|---|---|
| Pre-BP systolic & post-BP systolic | 0.986 | 0 | 0 |
| Pre-BP diastolic & BP diastolic | 0.978 | 0 | 0 |
| Pre-MAP & post-MAP | 0.775 | 0 | 0 |
| Pre-PR & Post-PR | 0.945 | 0 | 0.002 |
| Pre-Spo2 & Post-Spo2 | 0.913 | 0 | 0 |
Table 2: Paired Samples Correlations between parameters for group 1 ≤ 35.
| Parameter pair | Correlation | Sig. | Sig. (2-tailed) |
|---|---|---|---|
| Pre-BP systolic & post-BP systolic | 0.976 | 0 | 0.161 |
| Pre-BP diastolic & BP diastolic | 0.868 | 0 | 0.475 |
| Pre-MAP & post-MAP | 0.902 | 0 | 0.364 |
| Pre-PR & Post-PR | 0.888 | 0 | 0.001* |
| Pre-Spo2 & Post-Spo2 | 0.841 | 0 | 0.000* |
Table 3: Paired samples correlations between parameters for group 2 ≥ 35.
Discussion
Although using face mask and face shield (PPE) were utilized commonly by general dentists worldwide but the presence of COVID-19 pandemic makes it is usage mandatory in addition to emotional and physical activity and accurateness can be affected by the assistance of the dentist, tiredness commonly occur post the first hour of dental work. The amplified endogenously warmness of the dentist, as well as numerous features of the clinic room circumstances even in close atmosphere underneath the mask may also undesirably disturb the work of dentist.
Masks may have airway resistance, also lowering the oxygen saturation in blood levels may results from the higher levels of CO2 content of the inhaled air due to the expired CO2 that accumulated underneath face mask; In this research we have record SpO2 of arterial pulsations by a pulse oximeter device and observed a significant reduction in the red blood cells Oxygen saturation level of the dentist’s post-work, that is not related to continued sitting or anxiety. [21]
Pulse oximeter, currently regarded as a typical tool, simple device utilized to calibrate SpO2 within a satisfactory precision reading. Its effectiveness had been assessed lower than both standard (decent perfusion, SpO2 within a normal value without unimportant influences) and adverse conditions.
In spite of some device restrictions in the cases of carboxyhemoglobinemia, gesture artefact, existence of dyes, alteration in generalized vascular resistance, lowering blood pressure, nail stain, vasoconstriction, and iron deficiency, [22,23], it has been presented that physical age, sex, heaviness, body heat, Hb. concentration and pulse pressure (PP) have slight influence on precision of pulse oximeter devices in sensing low SpO2 in blood [24].
Most of pulse oximeter devices had a whole mean error of ≤ 1.0% in comparison to external other SpO2 devices [25,26]. Pulse oximeter devices restricted not to provide reading ≥ 100%, and these limits increase the incidence of false positive readings and creates unfairness and inaccurate calculations.
The dentist's post work SpO2 in blood level is declined more than one percent while the changeability of the SpO2 sensors is ≤1% [27]. Thus it is believed that wearing the surgical masks assist in reduction of oxygen inhale, but this happened may be due to psychosomatic limit over natural inhalation of the dentist.
Since this study is the former clinical research in recording a significant change in blood pressure readings involving MAP and no significant change in PR of the dentist post-work due to wearing the surgical mask for one hour in dental clinic with minimal non-significant change in SpO2.
Conclusion
As a conclusion of this study, wearing the PPE by the dentists or other health care providers has negligible effects on pulse rate of the heart and oxygen saturation in the red blood cells but had effects on blood pressure systolic and diastolic and means arterial pressure may be due to stress and psychological factors.
References
- https://www.who.int/emergencies/diseases/novel-coronavirus-2019 [Accessed 13 Sep 2020].
- Nguyen LH, Drew DA, Graham MS, et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health 2020; 5:e475–83.
- Stephenson K, Sowerby LJ, Hopkins C, et al. The UK national Registry of ENT surgeons with coronavirus disease 2019. J Laryngol Otol 2020; 1–5.
- Sommerstein R, Fux CA, Vuichard-Gysin D, et al. Risk of SARS-CoV-2 transmission by aerosols, the rational use of masks, and protection of healthcare workers from COVID-19. Antimicrob Resist Infect Control 2020; 9:100.
- WHO. Rational use of personal protective equipment (PPE) for coronavirus disease (COVID-19)-2020.
- Ramanathan Swaminathan, Bimantha Perera Mukundadura, Shashi Prasad. Impact of enhanced personal protective equipment on the physical and mental well-being of healthcare workers during COVID-19, Postgrad Med J 2020.
- Romney MG. Surgical face masks in the operating theatre: Re-examining the evidence. J Hospital Infection 2001; 47:251-256.
- Brooks JT, Butler JC. Effectiveness of mask wearing to control community spread of SARS-CoV-2. JAMA 2021; 325:998.
- Mayers JR. Patient monitors. In: Morgan EG, Mikhail MS, Murray MJ, et al. Clinical anesthesiology. 3rd Edn Lange; Mc Graw Hill, 2002; 86-126
- Busse MW, Maassen N, Konrad H. Relation between plasma K+ and ventilation during incremental exercise after glycogen depletion and repletion in man. J Physiol 1991; 443:469–476.
- Lee HP, Wang DY. Objective assessment of increase in breathing resistance of N95 respirators on human subjects. Ann Occup Hyg 2011; 55:917–921.
- Lässing J, Schulze A, Kwast S, et al. Effects of custom-made mouthguards on cardiopulmonary exercise capacity. Int J Sports Med 2021; 42:448-55.
- Fikenzer S, Uhe T, Lavall D, et al. Effects of surgical and FFP2/N95 face masks on cardiopulmonary exercise capacity. Clin Res Cardiol 2020; 109:1522-30.
- Ryan KL, Cooke WH, Rickards CA, et al. Breathing through an inspiratory threshold device improves stroke volume during central hypovolemia in humans. J Applied Physiol 2008; 104:1402-9.
- Convertino VA, Cooke WH, Lurie KG. Inspiratory resistance as a potential treatment for orthostatic intolerance and hemorrhagic shock. Aviation Space Environ Med 2005; 76:319-25.
- Fagoni N, Bruseghini P, Adami A, et al. Effect of lower body negative pressure on phase I cardiovascular responses at exercise onset. Int J Sports Med 2020; 41:209-18.
- Clegg CJ, Mackean DG. Advanced biology: Principles and applications. London: John Murray Publishers Ltd 1999.
- Ramendra Nath Kundu, Subir Biswas, Mithun Das. Mean arterial pressure classification: A better tool for statistical interpretation of blood pressure related risk covariates. Cardiol Angiol Int J 2017; 6:1-7.
- Pocock G, Richards CD. The human body: An introduction for the biomedical and health sciences. 1st ed. New York: Oxford University Press Inc. 2009.
- Amrata Srivastava, Rajeev Chitguppi. Accuracy of pulse oximeter readings while preventing cross contamination by wearing gloves before testing. 2020.
- Beder A, Büyükkoçak Ü, Sabuncuoğlu H, et al. Preliminary report on surgical mask induced deoxygenation during major surgery. Neuro 2008; 19:121-6.
- Jensen LA, Onyskiw JE, Prasad NG. Meta-analysis of arterial oxygen saturation monitoring by pulse oximetry in adults. Heart Lung 1998; 27:387-408.
- Sinex JE. Pulse oximetry: Principles and limitations. Am J Emergency Med 1999; 17:59-66.
- Villanueva R, Bell C, Kain ZN, et al. Effect of peripheral perfusion on accuracy of pulse oximetry in children. J Clin Anesthesia 1999; 11:317-22.
- Kagle DM, Alexander CM, Berko RS, et al. Evaluation of the ohmeda 3700 pulse oximeter: steady-state and transient response characteristics. J Am Society Anesthesiol 1987; 66:376-80.
- Ralston AC, Webb RK, Runciman WB. Potential errors in pulse oximetry: I. Pulse oximeter evaluation. Anaesthesia 1991; 46:202-6.
- Romney MG. Surgical face masks in the operating theatre: re-examining the evidence. J Hospital Infection 2001; 47:251-6.
Author Info
Abdulhameed N Aldabagh, Ziad H Deleme* and Alyaa I Naser
Department of oral and maxillofacial surgery, College of Dentistry, University of Mosul, IraqCitation: Abdulhameed N Aldabagh, Ziad H Deleme, Alyaa I NaserClinical Assessment of Cardiopulmonary Changes that Occurs During Dental Work for the Dentist with PPE during COVID-19 Pandemic in Mosul City, J Res Med Dent Sci, 2021, 9(8): 318-322
Received: 05-Aug-2021 Accepted: 19-Aug-2021
