Review - (2022) Volume 10, Issue 9
CHONDROCALCINOSIS IN A HYPOTHYROID FEMALE, AN UNFORGOTTEN ENTITY-A CASE REPORT AND LITERATURE REVIEW
Karthika Rajendran, Manjani S*, Balamurugan S and Khowsalya Subrajaa
*Correspondence: Manjani S, Bhaarath Medical College and Hospital (BIHER), India, Email:
Abstract
Arthropathy related to calcium pyrophosphate (CPP) dihydrate crystals has received little critical attention, until recently, CPPD disease was known as pseudogout. CPPD is commonly idiopathic, CPPD can also be associated with a number of metabolic diseases including, hypothyroidism, primary hyperparathyroidism, hereditary hemochromatosis, hypomagnesemia and hypophosphatasia. Chondrocalcinosis is more common in knees that have undergone meniscectomy than in contralateral non operated knees. Here we present a case of 70-year-old hypothyroid female presented with bilateral knee pain for 10 years. Patient was planned for right side knee replacement and incidentally per operative was found whitish chalky deposits which were sent for histopathological examination which revealed histomorphology features favoring calcium pyrophosphate crystalline disease (CPPD).
Keywords
Chondrocalcinosis, Meniscectomy
Introduction
Arthropathy related to calcium pyrophosphate (CPP) dihydrate crystals has received little critical attention, until recently, CPPD disease was known as pseudogout. CPPD is commonly idiopathic, CPPD can also be associated with several metabolic diseases, Hypothyroidism primary hyperparathyroidism hereditary hemochromatosis hypomagnesemia, and Hypophosphatasia Chondrocalcinosis is more common in knees that have undergone meniscectomy than in contralateral non operated knees. The features of the disease may mimic other rheumatic and nonrheumatic conditions, with misdiagnosis being a common problem [1,2]. Prevalence increases with age; CPPD is more common in women than in men, with a ratio of 1.4:1.0 [3]. An autosomal dominant mode of inheritance was suggested in several reports. CC is age-related with an incidence of 5% in patients >70 years, and nearly 50% in patients >90 years. [4].The differential diagnosis to be considered are osteoarthritis, hemarthrosis, CPPD, and chondrosarcoma respectively.
Case Report
A 70-year-old Indian hypothyroid woman on regular medications initially presented to the orthopedic department with a primary complaint of joint pain involving the bilateral knee joint. Plain radiographs of the bilateral knee showed the presence of bilateral linear meniscal deposits and calcification. These radiographic findings were suggestive of osteoarthritis of the knee joint, so the patient was planned for total knee replacement surgery. Laboratory tests were done as Preanesthetic workup. Her complete hemogram revealed Hb-11.8 g/dl, PCV -35.4%, renal parameters were blood urea - 19 mg/dl, serum creatinine- 0.5 mg/ dl. Thyroid profile revealed T3-2.6pmol/l, T4- 3pmol/l, TSH- 5.5mui/, Plasma glucose, Uric acid, Creatine kinase, and transferrin saturation were normal. Liver function tests were within normal limits. Further investigation: Rheumatoid factor –negative and the patient underwent right side total knee replacement. And the meniscal tissue was sent in 10% formalin for histopathological examination. Grossly linear calcified gray white firm soft tissue mass one measuring 4.5 x1 x 1 cm and the other measuring 4 x 1.5 x 1 cm, the tissue was decalcified using 1% nitric acid before processing, and tissue sections of 5-micron thickness were taken and stained using H&E and van kossa stain. Multiple sections studied showed a synovial tissue enclosing aggregates of basophilic material composed of vague surrounded by a collar of chronic inflammatory cells, histiocytes, and giant cells. Also noted are areas of chondrocyte metaplasia and myxoid degeneration. Histomorphological features favored the diagnosis of calcium pyrophosphate crystalline disease (CPPD). Postoperative period was uneventful, follow up after six-month the patient had no acute episodes (Figures 1-7).
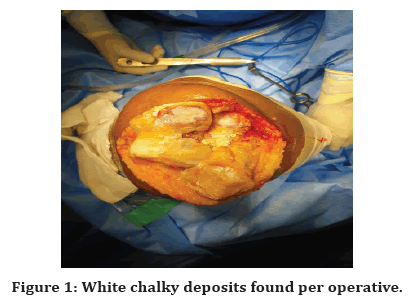
Figure 1. White chalky deposits found per operative.
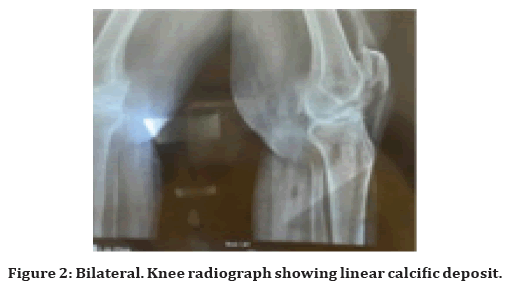
Figure 2. Bilateral. Knee radiograph showing linear calcific deposit.
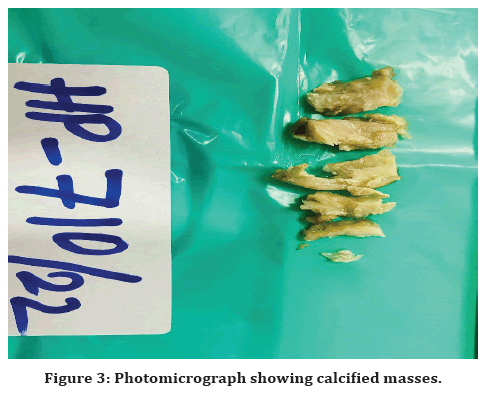
Figure 3. Photomicrograph showing calcified masses.
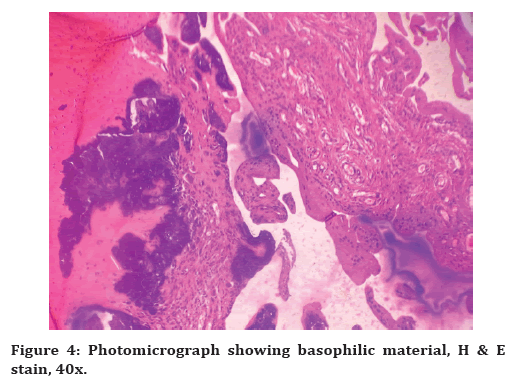
Figure 4. Photomicrograph showing basophilic material, H & E stain, 40x.
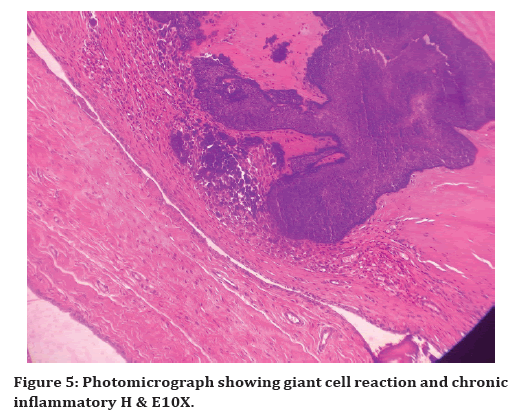
Figure 5. Photomicrograph showing giant cell reaction and chronic inflammatory H & E10X.
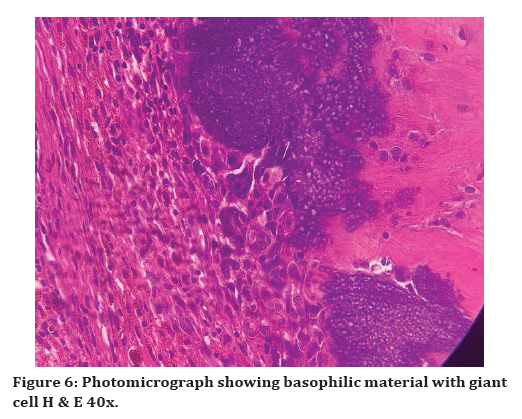
Figure 6. Photomicrograph showing basophilic material with giant cell H & E 40x.
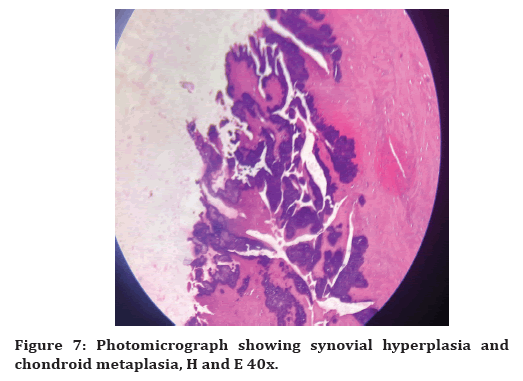
Figure 7. Photomicrograph showing synovial hyperplasia and chondroid metaplasia, H and E 40x.
Results
Although a causal relationship between thyroid hormones and pseudo gout is not very clear, thyroid hormones are potent stimulants of hypertrophy of growth plate chondrocytes and differentiation of articular chondrocytes. This case study emphasizes that chondrocalcinosis should be included in the differential diagnosis of arthritis and myalgia associated with hypothyroidism.
Discussion and Conclusion
Metabolic diseases and crystal-induced arthropathies are characterized by deposits of crystal and/ or noncrystalline (amorphous) calcium phosphates in synovial membranes (synovium) and periarticular soft tissues [5]. Both OA and CC are common in the elderly, the distinction between primary OA and CPPD arthropathy is indistinct and the role that each process plays in the pathogenesis of the other is not completely understood. Being that CPPD crystals are pro-inflammatory particles, it has long been assumed that these crystals might increase the risk of OA progression, as suggested by the association of rapidly destructive hip OA with CPPD crystal deposition. Rare extra-articular tophaceous CPPD deposition and sclero-choroidal calcifications, most often asymptomatic, have been reported mainly in association with metabolic diseases like hypothyroidism as in our case study. In a study by. Dorwart, et al. suggested an association between pseudo gout and hypothyroidism when 10% of their patients had underlying hypothyroidism, as with his study this present case also had hypothyroidism on treatment [6]. An earlier study by yang et al revealed that the most common finding in pseudo gout is calcification in and around the knee joint [7]. Similar findings were noted in the present case. The critical location of a CPPD deposit plays an important role in the development of neurological symptoms in these patients [8]. In a study done by Nakamura et al, it was found that Tophaceous pseudo gout may recur after complete or incomplete surgical excision, but in the present case study, the patient did have a history of any previous surgery [9]. Histologically, chondroid metaplasia in and around the areas of CPPD deposition was found with tophaceous pseudo gout [10]. Metaplastic chondrocytes could play an important role in the initial precipitation of CPPD crystals, and synovial chondrometaplasia was observed with pyrophosphate arthropathy, the present also shows histomorphological features of chondroid metaplasia. Another differential diagnosis to be considered is chondrosarcoma. A foreign body type granulomatous reaction containing histiocytes and giant cells is a helpful finding to distinguish it from chondrosarcoma. Similar findings were found in the present study.
References
- Rosenthal AK, Ryan LM. Calcium pyrophosphate deposition disease. N Engl J Med 2016; 374:2575-2584.
- Pascual E, Sivera F, Andres M. Mixed crystal disease: A tale of 2 crystals. J Rheumatol 2020; 47:1158.
- Gupta S, Vashiya R. Chdrocalcinosis: A common but poorly understood joint disease. Apollo Med 2018; 15:201.
- Wickrematilake G. Calcium pyrophosphate dihydrate deposition disease in young patients: Two case reports. Arch Rheumatol 2017; 32:80-83.
- Bély M, Apáthy A. Metabolic diseases and crystal induced arthropathies technic of non-staining histologic sections-A comparative study of standard stains and histochemical reactions. Clin Arch Bone Joint Dis 2018; 1.
- Dorwart BB, Schumacher HR. Joint effusions, chondrocalcinosis and other rheumatic manifestations in hypothyroidism. A clinicopathological study. Am J Med 1975; 59:780–790.
- Yang BY, Sartoris D, Resnick D, et al. Calcium pyrophosphate dehydrate crystal deposition disease: frequency of tendon calcification about the knee. J Rheumatol 1996; 23:883–888.
- Macmullan P, McCarthy G. Treatment and management of pseudogout: Insights for the clinician. Ther Adv Musculoskelet Dis 2012; 4:121-31.
- Nakamura O, Kaji Y, Yamagami Y, et al. A rare case of tumoral calcium pyrophosphate dihydrate crystal deposition disease of the wrist joint. Case Rep Orthop 2015; 2015:313291.
- Ishida T, Dorfman HD, Bullough PG. Tophaceous pseudogout (tumoral calcium pyrophosphate dihydrate crystal deposition disease). Hum Pathol 1995; 26:587-593.
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Indexed at, Google Scholar, Cross Ref
Author Info
Karthika Rajendran, Manjani S*, Balamurugan S and Khowsalya Subrajaa
Bhaarath Medical College and Hospital (BIHER), IndiaReceived: 05-Sep-2022, Manuscript No. jrmds-22-73735; , Pre QC No. jrmds-22-73735(PQ); Editor assigned: 06-Sep-2022, Pre QC No. jrmds-22-73735(PQ); Reviewed: 20-Sep-2022, QC No. jrmds-22-73735(Q); Revised: 23-Sep-2022, Manuscript No. jrmds-22-73735(R); Published: 30-Sep-2022
