Case Report - (2023) Volume 11, Issue 2
Case Report on Nursing Management of Congenital Heart Disease with Miliary Tuberculosis
Samiksha D Tamgadge*, Sheetal Sakharkar, Madhuri Shambharkar, Shalini H Moon, Bali Thool and Bibin Kurian
*Correspondence: Dr. Samiksha D Tamgadge, Department of Medical Sciences, Datta Meghe Institute of Medical Sciences, Maharashtra, India, Email:
Abstract
Introduction: Miliary tuberculosis is a type of tuberculosis. Tuberculosis is a specific chronic disease which is infectious caused by Mycobacterium tuberculosis. Primarily, it affects the lungs which cause pulmonary tuberculosis. It can also affect the lungs, causing pulmonary tuberculosis. It also affects meninges, intestine, bones, joints, lymph glands, skin and other tissues. In children the primary infection may occur in a year. It is very harmful for the health of the children. Early diagnosis may help to cure quickly.
Clinical findings: Tachycardia, cough, high grade fever, rash.
Diagnostic evaluation: The patient’s physical and clinical examination was taken. The blood test was done to check if there is any kind of bacteria is present. Sputum examination was also done. Electroencephalogram (EEG) was done.
Therapeutic intervention: Inj. Ceftriaxone (800 mg) (BD), Inj. Vancomycin (320 mg) (BD), Inj. Pantop (20 mg) (OD), Inj. Lasix (8 mg), Syrup paracetamol (5 ml) (SOS), Tab. Metoprolol (25 mg) (BD). Oxygen therapy should be given.
Outcome: After taking the prescribed medications and treatment, the patient's condition is better than previous. Conclusion: After giving treatment to the patient. He is now better.
Keywords
Miliary tuberculosis, Coarctation of aorta, Patent ductus arteriosus, Tachycardia
Introduction
Miliary tuberculosis is the widespread dissemination of Mycobacterium tuberculosis. It is the result of haematogenous dissemination and is characterized by extensive miliary mottling of lungs and involvement of spleen, liver and other tissues. It may be found as pulmonary type or septicemic type or meningitic type [1].
Coarctation of aorta is a distinct narrowing or a long segment hypoplasia of the aortic arch, usually distal to the subclavian artery. The narrow aortic lumen may exist as preductal or postductal obstruction which depends upon the position of the obstruction in relation to the ductus arteriosus. The lesion obstructs blood flow through the aorta, resulting in increased pressure and effort of the left ventricle. This condition is more commonly found in male and may accompany other defects like VSD, PDA, tubular hypoplasia of the aortic isthmus and bicuspid aortic valve. It is a common association in turner syndrome [2].
Case Presentation
Patient's identification data
A male child of age 8 years from Umarkhed, Yavatmal, admitted to the PICU of AVBR hospital on 20/11/2021 with the known cause of congenital heart disease with miliary tuberculosis. His weight is 16 kg [3].
Present medical history
A male child of 8 years old was brought to AVBRH on 20 November 2021 by his parents with a complaint of fever, cough and increased work of breathing and admitted to PICU. He has a known cause of congenital heart disease with miliary tuberculosis; the child was weak and inactive on admission [4].
Past medical history
A male child of 8 years old, his mother says that at 3 years of life the child had bluish discoloration of palms and soles [5].
History of family
The family consists of four people. My patient has been diagnosed to have congenital heart disease with miliary tuberculosis. The parent’s marriage is a consanguineous marriage. Not a single member of the family was complaining about their health only my patient was admitted because of his abnormal symptoms [6].
Sign and symptoms
Tachycardia, cough, high grade fever, rash.
Etiology
The etiology of miliary tuberculosis is a kind of microorganism which causes tuberculosis. It's contagious and spreads when someone with an active tuberculosis infection in their lung coughs or sneezes the bacterium into the air, which is then inhaled by someone else. It can linger in the air for several hours [7].
The etiology of congenital heart disease and the exact cause is unknown in about 90% of cases. Heredity and consanguineous marriage are important etiological factors. Genetic disorders and chromosomal aberrations are also known to predispose congenital heart disease [8].
Diagnostic evaluation
The patient’s physical and clinical examination was taken. The blood test was done to check if there is any kind of bacteria is present. Sputum examination was also done. Electroencephalogram (EEG) was done [9].
Congenital heart disease
Diagnosis of the condition can be confirmed by chest xray, barium swallow, EEG, M-mode echocardiography, cardiac catheterization and angiocardiography [10].
Miliary tuberculosis
The laboratory investigation should include isolation of AFB bacteriology examination, histopathology, immunediagnosis and other supportive investigations. The effective confirmatory investigation is the bacteriological isolation of the AFB. Sputum examination or laryngeal swab or peritoneal fluid in abdominal TB and CSF study in CNS involvement are very useful to confirm the diagnosis. Also the test like histological studies, immunodiagnosis of anti-tubercular antibodies and antigen by the radioimmunoassay, tuberculin test, BCG test, blood examination and radiology. My patient's 2D echo report paediatric.
Physical examination
My patient is conscious. Any of the abnormalities are not seen except murmur sound is present while auscultation.
Therapeutic intervention
• Inj. Ceftriaxone (800 mg) (BD)
• Inj. Vancomycin (320 mg) (BD)
• Inj. Pantop (20 mg) (OD)
• Inj. Lasix (8 mg)
• Syrup paracetamol (5 ml) (SOS)
• Tab. Metoprolol (25 mg) (BD)
Nursing perspectives: I have prepared 3 nursing diagnosis with the help of Nanda nursing diagnosis priority wise.
Congenital heart disease
Nursing diagnosis:
• Impaired gas exchange related to disturbed pulmonary blood flow.
• Cardiovascular output is reduced related to functions of the myocardium.
• Intolerance to physical activity related to hypoxia.
Nursing intervention based on the above nursing diagnosis:
• Relieving respiratory distress by semi upright position, clearing oral and nasal secretions, oxygen therapy, administering prescribed medications, (diuretic, bronchodilators) and prevention of aspiration with continuous monitoring of respiratory pattern (ABG analysis, respiratory status).
• Improving cardiac output by uninterrupted rest, minimum exercise (as play and other activities of daily living), maintaining normal body temperature and comfortable environment, administering medications and monitor child's condition (vital signs, heart sound).
• Improving oxygenation and activity tolerance by continuous monitoring by pulse oximetry, oxygen therapy (by face mask or nasal cannula) and emotional support with physical rest.
Miliary tuberculosis
Nursing diagnosis:
• Risk for infection related to inadequate primary defences.
• Ineffective airway clearance related to secretions that are thick and viscous.
• Risk for impaired gas exchange related to reduction in the effective lung surface area.
Nursing intervention based on the above nursing diagnosis:
• Advice the patient to cough or sneeze and expectorate into tissue rather than spit. Investigate proper tissue disposal and hand-washing methods. Encourage others to follow suit.
• Ask the patient to take positions like semi fowler’s or high position so that he could breathe properly. Teach the patient about deep breathing exercises.
• Provide supplemental oxygen as appropriate. Foster them to take good bed rest and restrict the activities.
Nursing management:
• Maintain the patient's baseline data.
• The specific management is done with antitubercular drugs.
• Bactericidal drugs are given as per physician's order.
• Provide medications with right dose, route and frequency.
• Before administering medications check its expiry date. If it is expired then discard it.
• Reducing pain and fever and anxiety by explanation, reassurance and answering.
• Good diet and balanced intake of protein and vitamins are essential.
• Fresh air, sunshine, hygienic measures, necessary rest and ambulation should be promoted.
• Follow-up at regular interval even by home visit and involvement of family members in continued care are essential part of management.
Results and Discussion
A male child of 8 year old from Umarkhed, Yavatmal was admitted to PICU AVBRH on 21 November 2021 with chief complaint of fever, cough and increased work of breathing. Investigations were conducted as soon as he was admitted to the hospital, and appropriate treatment was initiated. He showed little improvement after receiving the treatment and the treatment is still ongoing. All the investigations were done to assess the clinical conditions. The management is done. Antipyretics (paracetamol, mefenamic acid) and tepid sponge should be given to treat fever and medications like Inj. Ceftriaxone (800 mg) (BD), Inj. Vancomycin (320 mg) (BD), Inj. Pantop (20 mg) (OD), Inj. Lasix (8 mg), Syrup paracetamol (5 ml) (SOS) and Tab. Metoprolol (25 mg) (BD). Hydration and nutrition status to be maintained. Some children may require airway clearance and oxygen therapy. Rest, a comfortable position and sanitary measures should all be available (Figure 1).
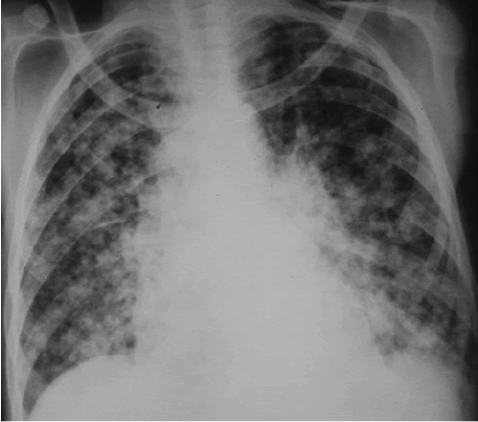
Figure 1: Miliary tuberculosis in a patient.
Diagnostic evaluation outcome
After taking treatment, the patient is better. Also he is responding to the medications. His fever has gone after taking the prescribed medications. His urine output is satisfactory and also oxygen therapy is continued.
Conclusion
My patient was admitted in PICU, AVBRH with a known case of congenital heart disease with miliary tuberculosis. He came with the chief complaint of fever, cough, increased work of breathing and fatigue. After getting proper treatment his condition is better.
References
- Khan MK, Islam MN, Ferdous J, et al. An overview on epidemiology of tuberculosis. Mymensingh Med J 2019; 28:259-266.
[Google Scholar] [PubMed]
- Fukuda J, Shingo Y, Miyako H. Primary tuberculous osteomyelitis of the mandible: A case report. Oral Surg Oral Med Oral Pathol 1992; 73:278-280.
[Crossref] [Google Scholar] [PubMed]
- Hime NJ, Zurynski Y, Fitzgerald D, et al. Childhood interstitial lung disease: A systematic review. Pediatr Pulmonol 2015; 50:1383-1392.
[Crossref] [Google Scholar] [PubMed]
- Sharma SK, Mohan A. Miliary tuberculosis. Microbiol Spectr. 2017; 5.
- Hamdan MA. Coarctation of the aorta: A comprehensive review. Prevalence 2006; 50:30.
- McKenna L, Sari AH, Mane S, et al. Pediatric tuberculosis research and development: Progress, priorities and funding opportunities. Pathogens 2022; 11:128.
[Crossref] [Google Scholar] [PubMed]
- Gallicchio CT, Alves ST, Ramos HI, et al. Association of Turner's syndrome and hypopituitarism: A patient report. J Pediatr Endocrinol Metabol 2003; 16:901-906.
[Crossref] [Google Scholar] [PubMed]
- Doshi AR, Chikkabyrappa S. Coarctation of aorta in children. Cureus 2018; 10.
[Crossref] [Google Scholar] [PubMed]
- Campbell M. Natural history of coarctation of the aorta. Heart 1970; 32:633-640.
[Crossref] [Google Scholar] [PubMed]
- Tamgadge S, Sakharkar S, Umate R. Case report on congenital heart disease with miliary tuberculosis. J Pharmaceutical Negative Results. 2022; 13:1038-1041.
Author Info
Samiksha D Tamgadge*, Sheetal Sakharkar, Madhuri Shambharkar, Shalini H Moon, Bali Thool and Bibin Kurian
Department of Medical Sciences, Datta Meghe Institute of Medical Sciences, Maharashtra, IndiaCitation: Samiksha D Tamgadge, Sheetal Sakharkar, Madhuri Shambharkar, Shalini H Moon, Bali Thool, Bibin Kurian, Case Report on Nursing Management of Congenital Heart Disease with Miliary Tuberculosis, J Res Med Dent Sci, 2023, 11 (02): 029-031.
Received: 07-Mar-2022, Manuscript No. JRMDS-22-56233; , Pre QC No. JRMDS-22-56233(PQ); Editor assigned: 10-Mar-2022, Pre QC No. JRMDS-22-56233(PQ); Reviewed: 24-Mar-2022, QC No. JRMDS-22-56233; Revised: 31-Jan-2023, Manuscript No. JRMDS-22-56233(R); Published: 28-Feb-2023
