Case Report - (2021) Volume 9, Issue 12
Case Report on Coronavirus Disease (COVID 19) Associated with Mucormycosis
Amruta Kothe*, Ruchira Ankar, Ranjana Sharma, Savita Pohekar, Sheetal Sakharkar and Vaishali Tembhare
*Correspondence: Amruta Kothe, Department of Medical Surgical, Smt. Radhikabai Meghe Memorial College of Nursing, Datta Meghe Institute of Medical Sciences (Deemed to be University) Sawangi (Meghe), India, Email:
Abstract
Introduction: Mucormycosis is the diseases caused by fungi (mucoroles) which grows rapidly, and the appearance is black, brown fuzzy. Mucormycosis usually infect people with an impaired immune system or with damage tissues. Mucormycosis is a rare but serious infection that complicates the course of severe COVID-19.
Patient history: The male patient of 44years old who was apparently admitted in Shalinitai Meghe Hospital and Research Centre on date 04/05/21 at casualty with chief complaint of high-grade fever, cough, shortness of breath, weakness. After all investigation done like RT-PCR, D-dimer, CBC, Ferritin, and ESR and finally diagnosed as Coronavirus disease (COVID19) and shifted to intensive care unit (ICU). After 16 days of ICU stay the patient develop signs of mucormycosis like pain, redness, and chemosis in the eye prominence.
Past history: Patient had no history of diabetes or any other debilitating conditions and no relevant family history.
Pharmacology: Patient was treated with antibiotic, antipyretic, steroids, vitamin C, multivitamin, and antifungal.
Management: Inj. Remdesivir, Inj Meropenem, Inj MPS, Inj Dexamethasone, Inj Febrinil, Syp Grilinctus, Syp Zincovit, Venti BIPAP, Tab Fluconazole.
Nursing management: Monitor the vital signs i.e., blood pressure, pulse, spo2, temperature, maintain oral hygiene, Maintain oxygen level and intake and output. BIPAP site observed and ensure that the patient is comfortable. Patient assessed for GCS, Glucose level, one side weakness and signs of mucormycosis.
Conclusion: There is higher risk of fungal infection like mucormycosis due to COVID -19 infection which is associated with impaired functioning of not only cellular but also humoral activity.
Keywords
COVID-19, Mucormycosis, Black fungus, Steroids
Introduction
Mucormycosis is the diseases caused by fungi (mucoroles) that grows rapidly and have a black, brown fuzzy appearance. Mucormycosis usually infect people with an impaired immune system or with damage tissues [1]. Coronavirus disease (COVID-19) has been managed with systemic glucocorticoids as a treatment by which fungal infections like mucormycosis (black fungus) are of concern with the clients [2]. Mucormycosis is a rare but serious infection that complicates the course of severe Covid-19 [3]. Due to profound lymphopenia and in advanced infection viral replication emphasize the inflammatory response and in the blood stream neutrophil and monocytes are influx leads to an imbalance between neutrophils and lymphocyte action making the patient more susceptible to systemic fungal infection like mucormycosis.
Incidence
Mucormycosis is a fatal infection. In case of brain involvement with black fungus infection then the mortality rises to 50%-80% [1]. It affects an estimated 14 in every 100,000 people in India. Globally Mucormycosis outbreak has being occurred. COVID 19 associated mucormycosis showed 94% clients had diabetes which was poorly controlled [4]. Mucormycosis is a disease associated with high mortality ranging from 25-62%. India contributes to 40% of global burden of this “rare mould” infection as it is called as western literature, with an estimated prevalence of 140 cases per million population.
Objective
• To know general idea regarding disease condition.
• To explore knowledge regarding pharmacology, medical and nursing management.
Patient information
Patient present history: The male patient of 44years old who was apparently admitted in SMHRC on date 04/05/21 at casualty with chief complaint of high-grade fever, cough, shortness of breath, weakness. After all investigation done like RT-PCR, D-dimer, CBC, Ferritin, and ESR and finally diagnosed as Coronavirus Disease (COVID19) and shifted to intensive care unit. Patient is on Venti–BIPAP as of not maintaining oxygen saturation. After 16 days of ICU stay the patient develop signs of mucormycosis like pain and redness, chemosis, swelling in the eye prominence (Figure 1).
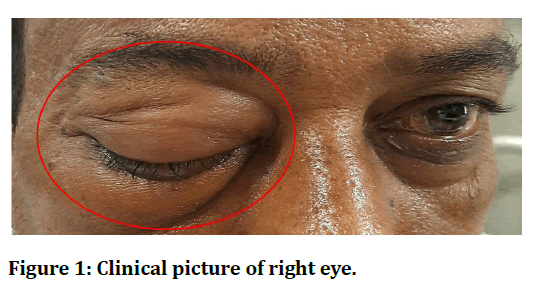
Figure 1. Clinical picture of right eye.
Past history: Patient had no history of diabetes or any other debilitating conditions and no relevant family history. Patient was not having any history of communicable disease, asthma, tuberculosis, or any hereditary disease.
Causes: Uncontrolled diabetes mellitus: As of decreased ability of their neutrophils to phagocytose as well as suffering from diabetic have peripheral nerve damage which reduces the blood supply that increase the chance of infection. Immunosuppression by steroids: Already COVID-19 affects immune system, and the treatment of COVID-19 involves steroids that suppress immune system due to these factors there is risk of attack of mucoromycetes. Prolonged ICU stay: Oxygen therapy in ICU in which humidifier is used are prone to get fungal infection as of exposure to moisture. Co-morbidities Post transplant, malignancy, Voriconazole therapy: Drug that suppresses the immunity which leads to attack the fungal infection.
Clinical finding: Sinusitis, one sided facial pain, swelling over eye prominence, eschar and black over bridge of nose/ palate, toothache, loosening of teeth, jaw involvement, blurred or double vision with pain, fever, skin lesion, thrombosis and necrosis, chest pain, pleural effusion, haemoptysis, worsening of respiratory symptoms.
Diagnosis evaluation
• History collection-Done.
• Physical examination-Done.
• X-ray–Done (Figure 2).
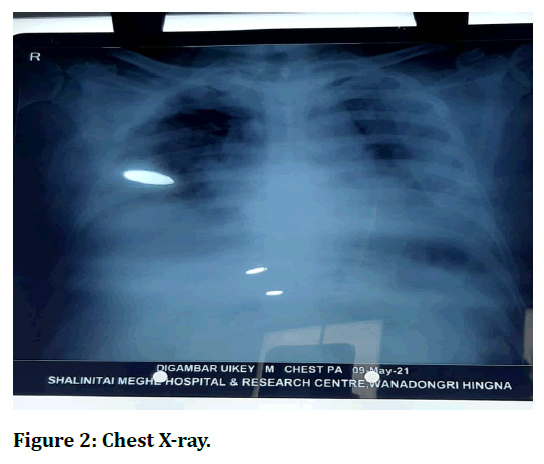
Figure 2. Chest X-ray.
• HRCT-Score was 21/25.
• Others: CBC, KFT, LFT, ESR, D-DIMER, RT PCR, FERRITIN, RBS, CRP, LDH.
Blood investigation report (Date 21. 5.2021) (Table 1)
| Investigation | Patient Value | Normal Value | Justification |
|---|---|---|---|
| Complete blood count | |||
| HB% | 14.5gm% | 13-15.4 gm% | Normal |
| MCV | 99cub. micron | 80-90 cub. Micron | Increased |
| MCH | 31.30% | 30-36.5 % | Normal |
| Total RBC Count | 4.68 millions/cu.mm | 4.5-6 millions/cu.mm | Normal |
| Total WBC Count | 16100 /cu.mm | 4000-11000/cu.mm | Increased |
| Total platelet count | 2.49 Lacs/cu.mm | 1.5-4 Lacs/cu.mm | Normal |
| KFT | |||
| Urea | 40mg% | 18-40 mg% | Normal |
| Creatinine | 0.80% | 7-1.5mg% | Normal |
| Sodium | 143meq/L | 136-145 mEq/L | Normal |
| Potassium | 3.27mEq/L | 3-5 mEq/L | Normal |
| LFT | |||
| Total protein | 5.49gm% | 6-8gm% | Normal |
| Albumin | 3.18% | 3-5gm% | Normal |
| Total bilirubin | 1.05mg% | 0.3-1 mg% | Normal |
| Bilirubin conjugated | 0.21 mg % | 0.1-3 mg% | Normal |
| D-dimer | 4.09 | ||
| FERRITIN | 697.7mmHg | 80-100mmHg | Increased |
| LDH | 801 I.U/L | 200-400 I.U/L | Increased |
| RBS- Glucose Plasma Random | 129mg% | 70-150mg % | Normal |
| ESR | 57 mm/ 1st hr | 1-10 mm/1st hr | Increased |
Table 1: Blood investigation report (Date 21. 5.2021).
The details are mentioned in Table 1.
Medical management
Now patient treatment in the intensive care unit (Table 2).
| Drug | Mechanism of action | Dose/route | Indication | Contraindication |
|---|---|---|---|---|
| Inj Meropenem (Broad spectrum antibiotic) | It penetrates bacterial cell and interfere vital cell wall component that leads to cell death. | 1gm/IV/TDS | Bacterial meningitis, Intra-abdominal infection | Seizures, diarrhoea, decreased blood platelets, CKD |
| Inj Remdesivir (antiviral) | It acts as nucleoside analog that inhibits RdRp also acts as antiviral that target coronavirus replication. | 200mg stat/IV and 100mg OD for 4days | Coronavirus | Neonates, Adults and Paediatric with severe renal impairment |
| Inj MPS (corticosteroid ) | It is a synthetic pregnane steroid hormone and decrease the inflammatory cycle. | 40mg /IV OD | Arthritis, psoriasis, allergic disorder, endocrine disorders. | Tuberculosis, diabetes, herpes simplex infection. |
| Inj Dexa (corticosteroid) | It synthesis of enzymes need to decrease inflammation and causes suppression by producing lymphocytopenia. | 4mg/IV BD | Cerebral edema, shock, meningitis. | Hypersensitive |
| Inj Lomoh (anticoagulant) | It prevents formation of blood clots and prevents blockage in blood vessels by activating certain blood clotting proteins. | 0.4ml subcutaneous OD | Deep vein thrombosis, pulmonary embolism | Hypersensitive |
| Inj Febrinil (analgesic and antipyretic) | It works by blocking the release certain chemical that cause pain and fever. | 900mg SOS | Headache, migraine, fever, pain | Hypersensitive |
| Tab Fluconazole (antifungal) | It exerts fungistatic effect by inhibiting fungal cytochrome. | 300mg OD | Candidiasis, meningitis, UTI | Hypersensitive |
| Inj Pan (antacid) | It inhibits the final step in gastric acid production. | 40 mg/IV OD | Heartburn, acidity | Interstitial nephritis, systemic lupus erythematous |
| Inj Emset (antiemetic) | It inhibits serotonin. | 4mg /IV TDS | Nausea, vomiting | Hypersensitive, Client taking apomorphine |
| Tab Fabridone (anti-inflammatory and antifibrotic) | It inhibits transforming growth factor beta. | 400mg BD | Idiopathic pulmonary fibrosis. | hypersensitivity |
| Syp Grilinctus | It acts on the brain cough centre as inhibits prostaglandins. | 10ml/TDS/oral | Cough, Throat irritation | hypersensitivity |
| Syp Zincovit (multivitamin) | It improves body’s immune function due to presence of selenium. | 10ml/TDS/oral | Nutritional supplement | hypersensitivity |
Table 2: Medical management.
Nursing management
The nurse oversees prescribing the medication and assessing their positive and detrimental effects on the patients. The pharmacologic therapy type and dosage is determined by the combination of these effects. Actions to assess clinical effectiveness in nursing include:
Observe for signs of respiratory fatigue such as shortness of breath and impaired cough.
Keep intake and output records to determine negative equilibrium.
Observe for any signs of fungal infection especially for mucormycosis as client receiving steroids and ventilation support.
Strict diabetic monitoring to control glucose level and prevent from complication.
Nursing diagnosis
Ineffective breathing pattern related to hypoxia as evidenced by shortness of breath.
• Strictly monitoring of oxygen saturation.
• Provide prop up position.
• Administer oxygen support as per physician order.
Acute pain related to inflammation of nerves as evidenced by pain scale assessment.
• Assess the baseline data to know the quality, severity, location, onset, duration, precipitating and relieving factors of pain.
• Provide comfortable position.
• Administer analgesic as per physician order.
Impaired physical mobility related to neuromuscular impairment as evidenced by decreased muscle strength.
• Perform active range of motion to all joints two times a day.
• Maintain skin integrity.
Anxiety related to change in health status and threat to self-concept as evidenced by expression of helplessness.
• Encourage for relaxation therapy.
• Provide information prior to every procedure.
Collaborative problems/ potential complication
• Blindness.
• Organ dysfunction.
• debridement (loss of body tissue).
• Death.
Continuing care
A referral to the home care may be suggested for a hospitalized patient depending upon the physical condition of the patient and the availability of family assistance. The patients with COVID 19 associated with Mucormycosis had impaired physical stamina and blindness which need home transfer assistance after hospitalization. The home care nurse’s assessment of the home’s physical environment is important. Suggestions to adapt the home environment to meet limitation of the patient’s activity are significant.
Discussion
Coronavirus disease (Covid-19) has already claimed more than one million lives worldwide. In the management of Covid-19 supportive care plays a vital role in the absence of an effective vaccine or antiviral therapy [5]. Glucocorticoids like Inj MPS 40mg, Inj dexamethasone 4mg and Inj remdesivir are the drugs which are proven to be beneficial in COVID -19 management with low dose and short durations. Due to the corticosteroid’s intake, there may be chances of uncontrolled hyperglycaemia hence diabetic patient are more vulnerable of mucormycosis [6]. Similar case of mucormycosis of mandible with unfavourable outcome was reported by Oswal et al. [6]. Studies on different opportunistic fungal infections were reported by Dubey et al. [7] and Choudhary et al. [8]. Related studies on Covid-19 were reviewed [9-12].
Strength
The male patient of 44years old tolerated all the medication and had better response around 1 month to the therapeutic treatment of the hospital which has been given.
Informed Consent
Before taking this case, information was given to the patients and relatives and informed consent was obtained from patient as well as relative.
Conclusion
The mortality in coronavirus disease associated mucormycosis (87.5% in current series) may be even higher than the observed in non-COVID patients. Control of hyperglycaemia, early treatment with liposomal amphotericin B and surgery are essential for successful management of mucormycosis. To improve outcomes of mucormycosis early diagnosis and timely management are necessary. Due to the early diagnosis and treatment of secondary fungal infections can substantially reduce morbidity and mortality.
References
- https://www.bbc.com/news/world-asia-india-57027829
- https://www.who.int/emergencies/diseases/novel-coronavirus-2019/advice-for-public?gclid=CjwKCAjw_JuGBhBkEiwA1xmbRXSeITVXNgemsYXubcLrXihoO4XaXKTiVeHuRzxUZqK6neFjUI9rRxoCe6EQAvD_BwE
- Garg D, Muthu V, Sehgal IS, et al. Coronavirus disease (Covid-19) associated mucormycosis (CAM): Case report and systematic review of literature. Mycopathologia 2021; 186:289–98.
- https://www.bbc.com/future/article/20210519-mucormycosis-the-black-fungus-hitting-indias-covid-patients
- Singh AK, Singh R, Joshi SR, et al. Mucormycosis in COVID-19: A systematic review of cases reported worldwide and in India. Diabetes Metab Syndr 2021; 15.
- Oswal NP, Gadre PK, Sathe P, et al. Mucormycosis of mandible with unfavorable outcome. Case Reports Dent 2012; 2012.
- Dubey A, Lanjewar A, Ghewade B, et al. Mediastinal actinomycosis: A rare section mediastinal pseudotumour. J Clin Diagnostic Res 2020; 14.
- Choudhary SV, Koley S, Mallick S, et al. Proximal subungual onychomycosis caused by aspergillus flavus in a HIV-positive patient. Indian J Dermatol Venereol Leprol 2009; 75:410–412.
- Arora D, Sharma M, Acharya S, et al. India in “flattening the curve” of COVID-19 pandemic-triumphs and challenges thereof. J Evolution Med Dent Sci 2020; 9:3252-6.
- Bawiskar N, Andhale A, Hulkoti V, et al. Haematological manifestations of covid-19 and emerging immunohaematological therapeutic strategies. J Evolution Med Dent Sci 2020; 9:3489-3495.
- https://www.jemds.com/data_pdf/Parth%20Godhiwala--CR-d.pdf
- Gupta K, Emmanouil D, Sethi A. Use of nitrous oxide‐oxygen inhalation sedation in the COVID‐19 era. Int J Paediatr Dent 2021; 31:433.
Author Info
Amruta Kothe*, Ruchira Ankar, Ranjana Sharma, Savita Pohekar, Sheetal Sakharkar and Vaishali Tembhare
Department of Medical Surgical, Smt. Radhikabai Meghe Memorial College of Nursing, Datta Meghe Institute of Medical Sciences (Deemed to be University) Sawangi (Meghe), Wardha, Maharashtra, IndiaCitation: Amruta Kothe, Ruchira Ankar, Ranjana Sharma, Savita Pohekar, Sheetal Sakharkar, Vaishali Tembhare, Case Report on Coronavirus Disease (COVID 19) Associated with Mucormycosis, J Res Med Dent Sci, 2021, 9(12): 82-86
Received: 22-Sep-2021 Accepted: 23-Nov-2021
